Elderly people are at higher risk for stroke, and their survival resp. Chances of recovery are lower than those of younger individuals. Gian Marco de Marchis, MD, Basel, and neurologist Prof. Gary Ford, Oxford, provided information on the “burden of disease” in stroke and on recanalization myths in elderly patients.
British neurologist Prof. Gary Ford, Oxford University and Oxford University Hospital (UK), provided information on the “burden of disease” in stroke. Every year, 15 million people worldwide suffer a stroke, and six million die as a result. Years of life lost to strokes increased 24% from 1993 to 2013. This trend will continue as people grow older – by 2080, there will be more than twice as many people over 85 as there are today. This will be a major challenge for the healthcare system, as there are already too few nursing staff in many industrialized nations.
More strokes in patients with comorbidities
Demographic trends also affect stroke centers: the average age at first stroke, for example, has increased from 72 years (2003-2005) to 75 years (2013-2017) at Lausanne University Hospital (CHUV). As more people survive a first stroke, second and third strokes are occurring more frequently – often in people with many comorbidities or pre-existing disabilities. Patient frailty, characterized by weakness, slow movements, decreasing energy, lower mobility, weight loss, and higher sensitivity to stressors, will also play an increasingly important role in stroke treatment. And the more frail the patients, the longer the hospital stay. In recent years, the rate of stroke patients who have dementia has also increased; they have a significantly worse outcome than those without dementia (higher mortality, more nursing home admissions). The impact of preexisting comorbidities on outcome in revascularization therapies is largely unknown because of a lack of good studies.
However, Prof. Ford did not want to paint the future black: “Age-related comorbidities can be delayed or even prevented by good prevention.” This includes, first and foremost, lowering elevated blood pressure and consistently treating other cardiovascular risk factors. “There are still primary care providers who think blood pressure should not be lowered in people over 80 because it increases the risk of falls,” the speaker said. “However, there is no evidence for this association.” Other important factors in prevention include sufficient physical activity and a balanced diet.
Recanalization myths in elderly patients.
PD Dr. med. Gian Marco De Marchis, Stroke Center, University Hospital Basel, addressed and corrected various misconceptions related to stroke in elderly patients.
- “Elderly patients no longer benefit from intravenous thrombolysis.” That this is not true was shown by a meta-analysis with data from over 6700 individuals: Patients over 80 benefited from thrombolysis (IVT) as much as younger patients in certain cases, even when just over 4.5 hours had elapsed from symptom onset to IVT [1].
- “Age is the most important risk factor for poor outcome, so endovascular therapies are futile in elderly patients.” Another meta-analysis proves the opposite [2]. Patients over 80 years of age have a poorer prognosis than younger patients – as is the case with virtually all diseases – but even those over 80 years of age have a better chance of a good outcome with endovascular therapy (EVT).
- “Patients with dementia have a higher risk of bleeding when treated with IVT.” About 10% of all stroke patients have dementia. This is not surprising because the same risk factors, such as smoking, hypertension, obesity, and diabetes, are involved in the pathogenesis of stroke and dementia. Dementia patients are less likely than other patients to be treated with IVT. Often, the reason is not an external factor such as contraindications or a late arrival time at the hospital, but simply the decision of the attending physician. Several studies show that patients with dementia do not have a higher incidence of bleeding and that, on average, their condition three months after stroke is no worse than that of stroke patients without dementia [3].
Are DOACs useful in elderly patients?
One in ten people over 75 years of age has atrial fibrillation, so anticoagulation should be given. But what about the efficacy and safety of vitamin K antagonists (VKA) and direct oral anticoagulants (DOAC) in the elderly? It is undisputed that the risk of bleeding is increased in elderly patients. “Encouragingly, the proportion of patients older than 75 years in the pivotal trials for each DOAC was above 30%,” the speaker said. Therefore, the evidence of the data for this age group is good. A meta-analysis including 22,381 patients with AF showed that DOACs were more effective than VKAs in preventing stroke or systemic embolism in patients older than 75 years [1].
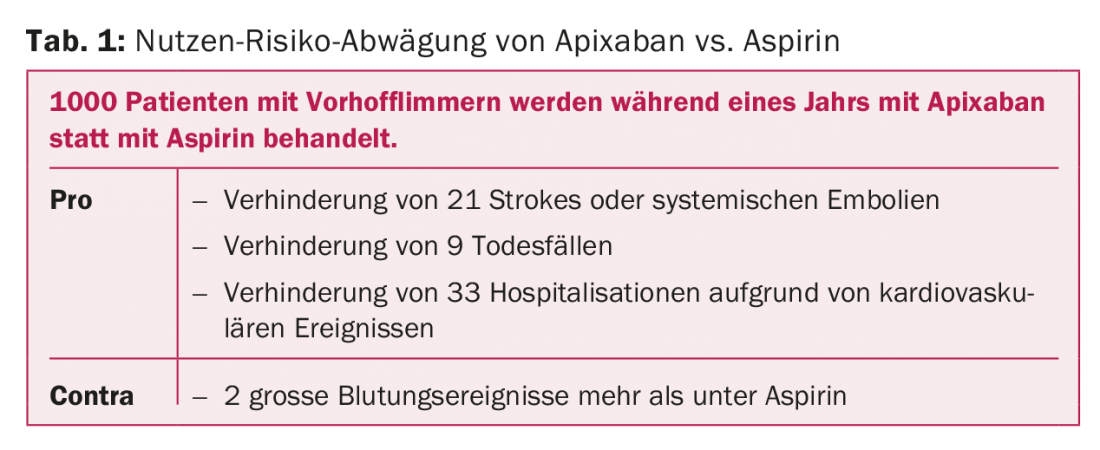
Since there are no randomized-controlled trials comparing the individual agents, this comparison is only possible via indirect data. Great caution is warranted in their interpretation, as the study populations of the individual DOAC studies differ substantially. These show that all four DOACs on the market are all equally effective and safe. Although apixaban shows a lower bleeding risk than dabigatran and rivaroxaban, “this is likely due to differences in study populations,” Dr. De Marchis pointed out. This difference should not be overstated. Thus, these differences were not confirmed in the DOAC studies of deep vein thrombosis. He also drew attention to the fact that patients with limited life expectancy or dementia and people living in nursing homes are underrepresented in such studies. Thus, more studies examining the effects and safety of DOAC in the particularly vulnerable, frail elderly are needed. At the same time, available data suggest that these patient groups may also benefit from all four DOACs. There are also myths about anticoagulation in the elderly that prevent good care. One is: “The elderly are more likely to fall, so they should receive aspirin rather than an anticoagulant, regardless of their CHADS score.” Studies clearly show that this is a misconception, as the risk of bleeding is only marginally higher under therapy with apixaban instead of aspirin [4]. However, many strokes and cardiovascular events can be prevented (Table 1).
Anticoagulation in elderly patients – Conclusion.
- Age alone should not be a reason for exclusion of recanalization therapy for stroke.
- Even mild dementia should not preclude recanalization therapy.
- At the same time, not all patients with dementia are suitable for all therapies. Clinical decisions should always be individualized and based on an open discussion with the affected person as well as their family members. One size does NOT fit all!
- All DOAC are safe and effective for the treatment of elderly patients.
- Comparing individual DOACs to each other may result in misleading results because the corresponding baseline data are not comparable.
- Elderly patients with AF who are not eligible for therapy with a VKA may benefit from a DOAC.
Source: Swiss Cerebrovascular Society Annual Meeting, January 11-12, 2018, Lausanne.
Literature:
- Emberson J, et al: Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014; 384: 1929-1935.
- Goyal M, et al: Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723-1731.
- Gensicke H, et al: Intravenous Thrombolysis in Patients Dependent on the Daily Help of Others Before Stroke. Stroke 2016; 47: 450-456.
- Connolly SJ, et al: Apixaban in patients with atrial fibrillation. N Engl J Med 2011; 364: 806-817.
CARDIOVASC 2018; 17(1): 32-34