Removal of colorectal liver metastases is prognostic. Oncologic and surgical technical criteria are used to assess resectability.
Colorectal cancer (CRC) is the third most common cancer in the Western world. 50% of all patients with colorectal cancer develop hepatic metastases, and the liver is the most commonly affected organ. 14-20% of patients have liver metastases at the time of diagnosis, while the rest are diagnosed during the course of their disease. Hepatic metastasis is classified as stage IV colorectal cancer disease and has an average 5-year survival rate of 10-15%. In patients with tumors that respond well to established chemotherapy and can be removed with modern surgical as well as interventional radiological techniques, this survival rate is significantly higher at 25-40%. The survival benefit of more than 20% also applies to patients with extensive liver metastases that were initially classified as non-resectable and only became removable after aggressive chemotherapy.
Timely referral of a patient with extensive hepatic colorectal metastasis to a specialized center is an important factor in putting these findings into practice in Switzerland.
What is the oncosurgical strategy for liver metastases?
The goal of treatment for patients with liver metastases is long-term tumor control. Surgical resection of liver metastases helps to achieve this goal. Selection of patients who qualify for potentially curative surgery is an interdisciplinary process. The suitability of a patient for resection is based on several criteria: Patient’s general condition, oncologic appropriateness, and technical resectability.
Which patients can be resected?
From a surgical-technical point of view, it is important to maintain an adequate reserve of functional liver parenchyma during liver surgery. Resection of too much liver tissue leads to postoperative organ failure, which has a high mortality and must be avoided at all costs. Assessment of technical resectability involves a multifaceted analysis of liver anatomy, histology, and function that is best performed by a team of hepatobiliary surgeons, radiologists, hepatologists, and pathologists. Technical resectability is a matter of ensuring, according to modern criteria, that future liver volume (“future liver remnant”, FLR) and liver function after resection are adequate. In this regard, liver volumetry allows accurate quantification of the expected FLR volume. For patients with a normally functioning liver parenchyma, the guideline is that a reduction in liver volume down to 20-25% (corresponding to about two liver segments) can be tolerated. Patients who are expected to have liver damage due to previous chemotherapeutic treatment need an FLR volume of at least 30-35%, and those with liver cirrhosis even more. An important innovation in recent years has been the trend toward parenchyma-sparing surgery, which means that resection planning is often guided by nonanatomic resections rather than the anatomic boundaries of individual liver segments. Thus, maximum sparing of healthy liver tissue can be achieved.
How is liver function assessed preoperatively?
There are few common tests that help to better assess liver function. The easily determined “liver values” in blood tests (e.g., bilirubin) are not sensitive enough to reflect the subtle changes in function after chemotherapy. The indocyanine green test has a higher sensitivity, but is hardly used in Europe in German-speaking countries. In Winterthur, we consider the gold standard to be liver scintigraphy, also called HIDA scan. It provides very sensitive information about the function of precisely those areas of the liver that remain after resection, the so-called “liver reserve”. In addition, a biopsy of the non-tumor affected liver may also provide important clues to the presence of fibrotic remodeling or even cirrhosis, which would severely limit the regenerative capacity of the liver and make extensive liver resection impossible.
Is it possible to make the remaining liver larger?
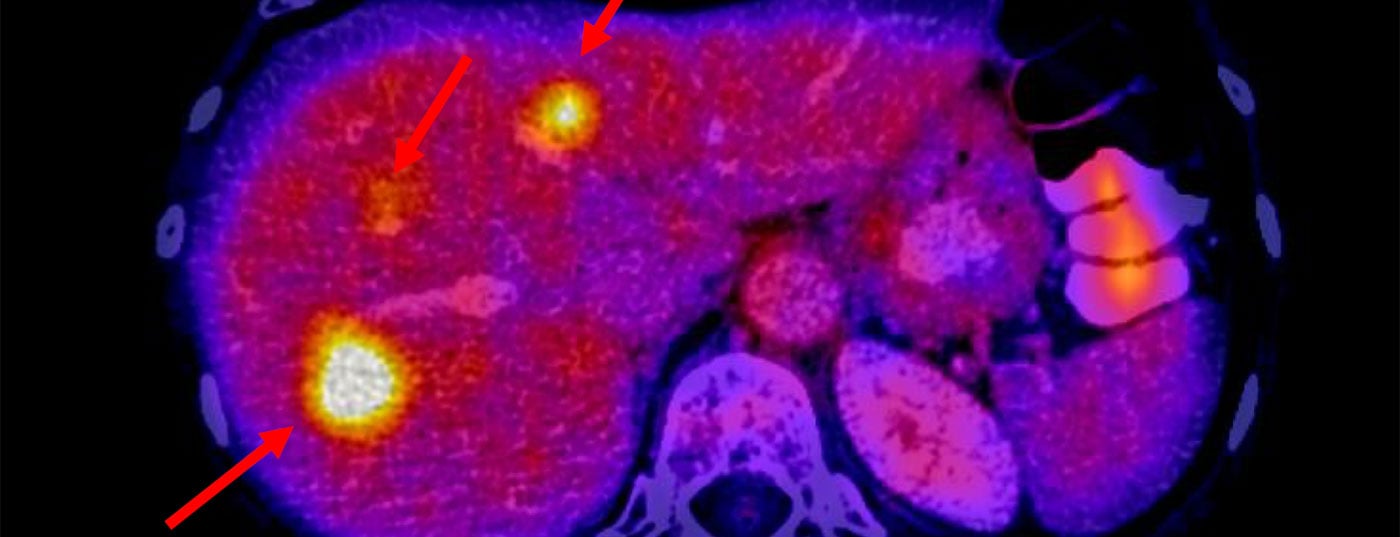
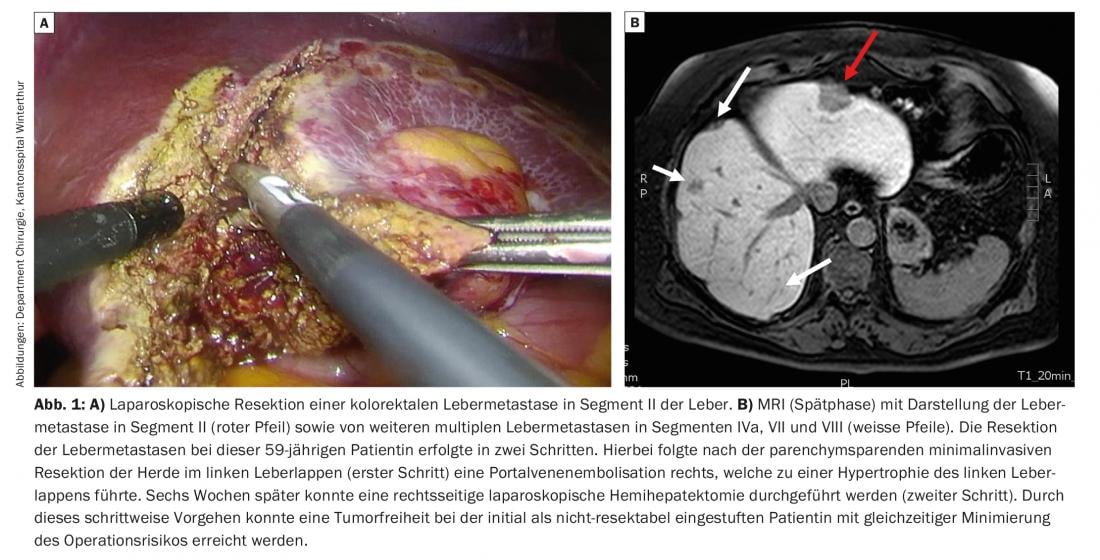
Most patients do not have extensive tumor involvement of the liver (e.g., small-volume metastases), and resection of all foci can often be performed safely and effectively; in 80% of cases, this is even possible laparoscopically (Fig. 1). In this regard, the minimally invasive procedure has the particular advantage of faster patient recovery and also causes less intra-abdominal adhesions, which is an advantage for the patient if the procedure is repeated. If the liver reserve turns out not to be large enough, certain methods can be used to grow the liver before resection. This involves blocking portal vein flow either by embolization (percutaneous portal vein embolization, PVE) or by surgical ligation (portal vein ligation, PVL), resulting in growth of the opposite side of the liver.
How does a PVE work?
In PVE, special plastic preparations or coils are inserted into the portal vein branches supplying the portion of the liver to be resected. Occlusion of the portal veins leads to hypertrophy of the segments to be left (i.e., the FLR). In the case of bilobar colorectal metastases, two operations are often performed consecutively. In the first operation, the metastases in the future remaining liver parenchyma are removed (Fig. 1) – followed by percutaneous PVE and then in a second operation by resection of the still tumor-involved embolized liver areas. These procedures allow extended liver resection to be performed in patients who have been classified as technically non-resectable due to an insufficient FLR at initial evaluation. This two-stage surgical procedure reduces the risk of postoperative liver failure. Long-term survival in patients treated with two surgeries is the same as in patients treated with only one surgery.
What is ALPPS?
In addition to PVE, other strategies are under discussion to stimulate liver regeneration. For example, the modification of the FLR can be achieved operationally in a two-step operation called “ALPPS”. In the first step, the liver parenchyma is cut in addition to the ligation of a portal vein branch. As a result, the future retained liver fraction (FLR) hypertrophies much more rapidly than with portal vein occlusion alone. The second step is to complete the hepatectomy. The primary advantage of this technique is that the probability of complete tumor resection is even higher with this strategy than with the conventional methods PVE and PVL. However, there is evidence that fast-growing liver tissue does not perform quite as well as slow-growing liver tissue. In addition, there is some concern about the complication rate of this surgery, which is still quite high.
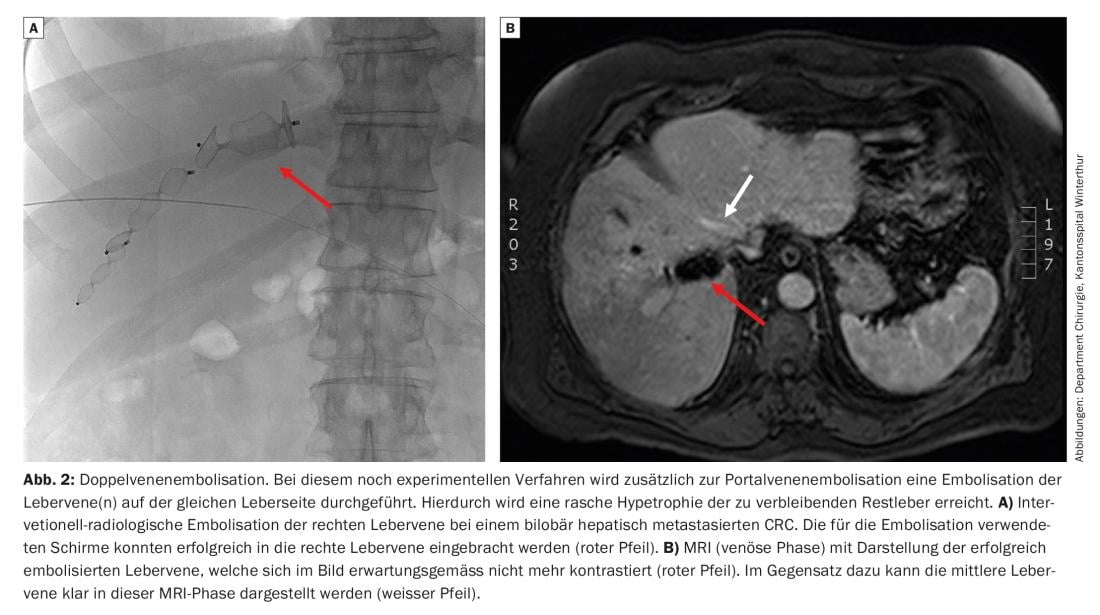
Further developments in liver tissue manipulation are currently being explored. These include, for example, the innovative double vein embolization, in which the ipsilateral hepatic vein is embolized percutaneously in addition to the PVE (Fig. 2) . This method can achieve equally rapid hypertrophy of the FLR, similar to ALPPS, without the need for two operations.
Is it possible to make the metastases smaller?
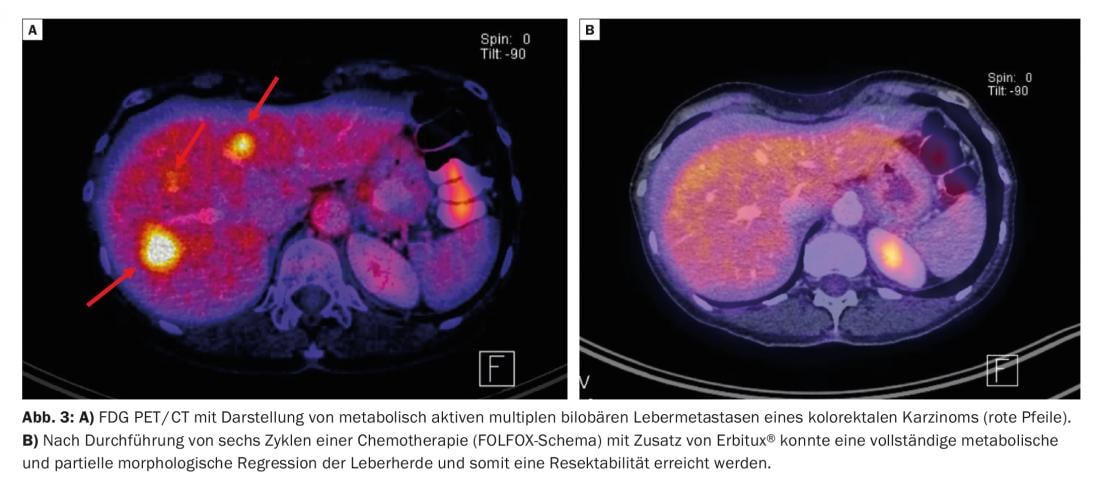
Patients with extensive metastases are often unsuitable candidates for liver resection because of the extent and anatomic distribution of the liver foci. In addition to manipulating liver volume, chemotherapy can lead to an impressive size reduction (so-called downsizing) of the initial tumor burden. The oncological combination therapies used here, such as the FOLFOX regimen, are often combined with antibodies for tumor growth factors such as cetuximab and bevacizumab (Fig. 3) . These therapies result in more than 50% of initially non-resectable patients becoming resectable after all due to this downsizing.
Take-Home Messages
- Removal of colorectal liver metastases can be curative and prolongs survival. Determination of resectability is based on oncologic and surgical criteria.
- From an oncologic perspective, the possibility of complete removal of all vital both intra- and extrahepatic tumor areas must be given with curative intent.
- From a technical perspective, resectability is achieved when all vital metastases can be removed with microscopically negative resection margins and sufficient residual liver volume. In this regard, the treating interdisciplinary team has at its disposal a number of well-established procedures aimed at both manipulation of liver reserve and reduction of tumor involvement. Even in cases of extensive metastasis to the liver, curative therapy is pursued.
Further reading:
- Adams RB, et al: Selection for hepatic resection of colorectal liver metastases: expert consensus statement. HPB (Oxford) 2013 Feb; 15(2): 91-103.
- Folprecht G, et al: Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol 2010 Jan; 11(1): 38-47.
- Guiu B, et al: Extended liver venous deprivation before major hepatectomy induces marked and very rapid increase in future liver remnant function. Eur Radiol 2017 Aug; 27(8): 3343-3352.
- Ironside N, et al: Systematic review of perioperative and survival outcomes of liver resections with and without preoperative portal vein embolization for colorectal metastases. HPB (Oxford) 2017 Jul; 19(7): 559-566.
- Jones RP, et al: Effect of specialist decision-making on treatment strategies for colorectal liver metastases. Br J Surg 2012 Sep; 99(9): 1263-1269.
- Nordlinger B, et al: Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet 2008; 371: 1007-1016.
- Olthof PB, et al: Hepatobiliary scintigraphy to evaluate liver function in associating liver partition and portal vein ligation for staged hepatectomy: Liver volume overestimates liver function. Surgery 2017 Oct; 162(4): 775-783.
- Ruers T, et al; EORTC Gastro-Intestinal Tract Cancer Group: radiofrequency ablation combined with systemic treatment versus systemic treatment alone in patients with non-resectable colorectal liver metastases: a randomized EORTC Intergroup phase II study (EORTC 40004). Ann Oncol 2012 Oct; 23(10): 2619-2626.
- Tomlinson JS, et al: Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 2007 Oct 10; 25(29): 4575-4580.
- Schadde E, et al: Monosegment ALPPS hepatectomy: extending resectability by rapid hypertrophy. Surgery 2015; 157: 676-689.
- Schadde E, et al: Prediction of Mortality After ALPPS Stage-1: An Analysis of 320 Patients From the International ALPPS Registry. Annals of surgery 2015; 262: 780-785.
HAUSARZT PRAXIS 2018; 13(1): 20-23
InFo ONCOLOGY & HEMATOLOGY 2019; 7(6): 17-19.