Chronic inflammatory bowel diseases place high demands on the treating physicians. Attention must be paid to a variety of factors. In addition, the focus is on the patient – his or her individual risk, wishes and expectations of the therapy.
The management of patients with inflammatory bowel disease (IBD) is complex and multifaceted, as attention must be paid to a variety of factors. These factors include, for example, the pattern of disease involvement (localization, activity), extraintestinal manifestations (such as cutaneous or articular symptoms), clinical course, and drug-therapeutic history. Furthermore, patient-related risks such as pregnancy, advanced age, st. n. or current tumor disease as well as patient preferences regarding a certain therapy (e.g. due to possible side effects or mode of application) and the cost of treatment play an essential role.
Ulcerative colitis
In ulcerative colitis, inflammation exists ascending from the rectum with variable intensity and extent. In cases of mild to moderate inflammation, therapy with 5-ASA preparations (mesalazine/mesalamine/5-aminosalicylic acid) is started first. These drugs are used for both remission induction (elimination of inflammation) and remission maintenance (prevention of recurrence) of ulcerative colitis. Depending on the extent of the disease, various topical 5-ASA therapeutics are used initially (suppositories, enemas, and foams), which are supplemented with oral 5-ASA preparations depending on response.
In the case of isolated, mild to moderate inflammatory rectal involvement (proctitis), local therapy with 1 g 5-ASA (as suppository)/day started (e.g. daily Salofalk® Supp 1 g, Pentasa® Supp 1 g, asazine® Supp 3× 500 mg). If this treatment is not effective enough, an additional oral 3 to max. 4 g 5-ASA added (e.g. daily Asacol® 3× 800 mg, Salofalk® Gran 3 g, Pentasa® Depotgran 2× 2 g, Asazine® 3× 800 mg). If the disease extends to the left flexure (descending colon, sigmoid colon, and rectum), initial mild to moderate inflammation is treated with an enema in the evening with at least 1 g and maximum up to 4 g 5-ASA started (e.g. daily Salofalk® Clysms 2 g or 4 g, Asacol® Rectal Foam Clysms 2 g or 4 g, Pentasa® Klysma 1 g/day). Again, if insufficient efficacy, additional treatment with oral 3-4 g 5-ASA would be given. Pancreatitis (inflammation affecting the entire colon) is started directly with an oral 5-ASA preparation.
If successful, long-term therapy for (steroid-free) remission maintenance with 5-ASA therapeutics is recommended. The European ECCO guidelines [1] recommend an oral 5-ASA dose of 2 g/day. The Swiss Drug Compendium gives the 5-ASA emission dose up to max. 1.2 g/day, which in our opinion is not comprehensible. Local therapy is administered (in addition to or instead of oral treatment) with 2× 500 mg 5-ASA Supp or 5-ASA Klysmen containing 2000 mg.
In general, local 5-ASA therapy is usually (wrongly!) neglected by both the physician and patient. For example, in the rectum, topical 5-ASA therapy achieves higher mucosal concentrations than oral treatment [2].
For remission maintenance, the probiotic E. coli Nissle can also be used (e.g. Mutaflor® in the dose of 1-2 caps./day). E. coli Nissle (bacteria of strain Nissle 1917) showed comparable efficacy to 5-ASA with respect to remission maintenance in ulcerative colitis in several randomized controlled trials [3].
If 5-ASA preparations are not effective enough due to excessive inflammatory activity of the colitis, therapy escalation with oral corticosteroids must be initiated. Here, cortisone is started with approx. 1 mg/kg body weight/day, with 60 mg/day usually being sufficient and (if there is an appropriate response) reduced by approx. 10 mg/week at weekly intervals. If more than two relapses occur per year despite extended remission-maintaining 5-ASA therapy, treatment with immunosuppressants would have to be initiated.
Estimation of inflammatory activity
On the one hand, the clinic can help to assess the effectiveness of the therapy. Successful therapy is manifested by a reduction in the number of bowel movements with improved consistency and less (or complete disappearance of) blood and less abdominal pain. On the other hand, the determination of calprotectin in stool helps us to estimate the inflammatory activity of colitis, the course of the disease and the success of therapy.
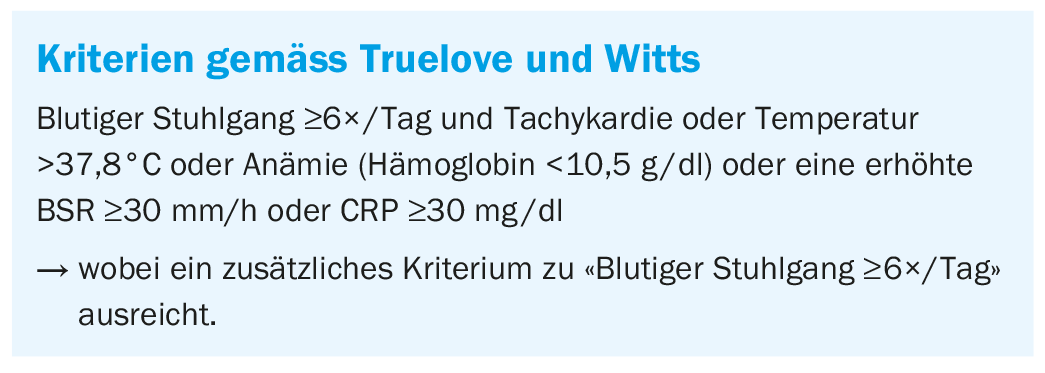
If the inflammatory activity of IBD cannot be controlled even with oral steroids (persistent or progressive symptoms of the patient) or if evidence of severe inflammation (meeting the Truelove/Witts criteria [4], box) should become apparent, it is highly recommended to contact a gastroenterologist directly. It must be evaluated whether hospitalization of the patient is necessary for further diagnostics (endoscopy, abdominal imaging, stool examinations, etc.) and therapy (e.g., with corticosteroids i.v., TNF-α blockers, ciclosporin or tacrolimus). Furthermore, in severe cases, interdisciplinary close-meshed care of the patient must be ensured (emergency team, internist, gastroenterologist and visceral surgeon).
Crohn’s disease
In principle, Crohn’s disease can become inflammatory at any site in the gastrointestinal tract. Furthermore, the disease may present with fistulization, stenosis, or luminal inflammation or mixed forms and may also show extraintestinal manifestations. An acute episode of Crohn’s disease can be treated with 1 mg prednisone/kg body weight with subsequent weekly dose reduction (as already described for ulcerative colitis). In case of ileocecal infestation, budesonide 9 mg/day can be used for treatment (dose reduction in the course). Immunosuppressants are used for colonic, small bowel, or upper gastrointestinal activity. 5-ASA therapy is no longer a standard option in Crohn’s disease.
Immunosuppressants
Patients who suffer from more than two relapses per year or have continuously increased disease activity should be managed with immunosuppressants. These include azathioprine, 6-mercaptopurine, or methotrexate. Because of a number of possible side effects, close medical monitoring is necessary when using thiopurines. Methotrexate is a good alternative in patients with Crohn’s disease, especially in those patients who also have joint symptoms [5,6].
Biologics
In addition to steroids, 5-ASA and immunosuppressants, there are now a number of monoclonal antibodies which, under the umbrella term “biologics”, have a significant role in the treatment of inflammatory bowel disease. Fortunately, homing receptor blockers and interleukin-12/23 blockers are now available in addition to the TNF blockers that have been on the market for 20 years. The big question for the treating physician is which of these drugs to use in which patient. This decision is not always easy and sometimes causes headaches even for experienced specialists. Unfortunately, there are not many predictive factors that would make a clear algorithm useful. The extent of inflammatory activity, the presence of extraintestinal manifestations, or even concomitant diseases such as heart failure, psoriasis, and multiple sclerosis influence the choice of medication.
TNF blockers should be used especially when the goal is to treat extraintestinal manifestations in addition to intestinal inflammation or to rapidly induce remission. Particularly in patients with pronounced inflammation, these drugs should be used and their dosage adjusted accordingly by determining sebum levels in the serum. Long-term therapy with TNF blockers is certainly possible, but a loss of efficacy of about 10% per year must be expected with these drugs. If infliximab is chosen as a therapeutic agent, a combination with an immunosuppressant is helpful, as this increases efficacy and reduces antibody development against the TNF blocker. In Switzerland, infliximab and adalimumab are available for ulcerative colitis and Crohn’s disease, while certolizumab has been approved only for Crohn’s disease and golimumab only for ulcerative colitis.
Homing receptor blockers: Currently, vedolizumab is approved in Switzerland as an α-4-β-7 antibody. Other antibodies with a similar mechanism of action will soon follow. With vedolizumab, the α-4-β-7-indicrin is highly selectively blocked on lymphocytes. α-4-β-7 binds MADCAM, which is predominantly found in the intestine. This is one of several steps in how lymphocytes are slowed down in the vessels and subsequently pass through the endothelium to their target site, e.g. the mucosa. After blockade of α-4-β-7, inflammatory cells can then no longer migrate to the site of inflammation in the intestine. Vedolizumab is characterized by an extremely good side effect profile and also appears to have very good long-term efficacy. However, this drug takes several weeks to become fully effective and is therefore less suitable for fulminant relapses. Extraintestinal manifestations appear to be less efficiently treated with this drug than with TNF blockers. Complete mucosal healing may occur with vedolizumab [7].
Ustekinumab: This interleukin-12/23 antibody is approved for Crohn’s disease in Switzerland. It binds to the P40 subunit of IL-12 and IL-23 cytokines and prevents signaling and interaction with the IL-12 receptor. This leads to decreased cellular activity and cytokine production. Initial therapy is given as an infusion, and maintenance therapy is then given as subcutaneous injections. This drug is excellent in patients who have psoriasis in addition to Crohn’s disease. Besides, it is a potent drug in patients with refractory disease. In clinical practice, it is often used when patients no longer respond to TNF blockers. Ustekinumab is also characterized by an excellent side effect profile; known side effects include headache and nasopharyngeal infections. Ustekinumab can also be used as long-term therapy [8].
All of the above drugs are effective in a maximum of two-thirds of patients, i.e. as long as there are no predictive factors, a change of drug may have to take place if there is no response. Unfortunately, this also means that there are still a few patients who do not go into remission with any of the drugs mentioned.
Take-Home Messages
- 5-Aminosalicylates remain an important mainstay of acute therapy and remission maintenance in ulcerative colitis.
- Rectal therapy with 5-ASA in the form of suppositories, clysms, or foam products should be preferred for distal colitis.
- If there are more than two episodes/year, immunosuppressive therapy should be started.
- Calprotectin is valuable for estimating disease activity and progression.
- If there is evidence of severe inflammation of colitis, a specialist should be contacted.
- Biologics can also put severe courses of IBD into remission.
Literature:
- Harbord M, et al: Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 2: Current Management. JCC 2017; 11: 769-784.
- Pimpo MT, et al: Mesalazine vanishing time from rectal mucosa following its topical administration. JCC 2010; 4: 102-105.
- Kruis W, et al: Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 2004; 53: 1617-1623.
- Truelove SC, Witts LJ: Cortisone in ulcerative colitis; final report on a therapeutic trial. British Medical Journal 1955; 2: 1041-1048.
- Dignass A, et al: Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. JCC 2012; 6: 991-1030.
- Dignass A, et al: The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Current management. JCC 2010; 4: 28-62.
- Noman M, et al: Vedolizumab Induces Long-term Mucosal Healing in Patients With Crohn’s Disease and Ulcerative Colitis. JCC 2017; 11: 1085-1089.
- Sandborn WJ, et al: Long-term efficacy and safety of ustekinumab for Crohn’s disease through the second year of therapy. APT 2018; 48: 65-77.
HAUSARZT PRAXIS 2019; 14(1): 7-10











