Treatment options for patients with diabetes and chronic kidney disease (CKD) have improved significantly thanks to new therapeutic options from the SGLT-2-i, GLP-1-RA and MRA drug classes. The new guidelines issued last year by KDIGO (Kidney Disease: Improving Global Outcomes) aim to provide practical guidance for use in everyday clinical practice. How barriers to implementing these recommendations can be overcome was discussed at this year’s European Renal Association (ERA) Congress.
Type 2 diabetics make up a large proportion of the CKD patient population – up to 40% have chronic kidney disease (CKD ) [3]. This is not only prognostically unfavorable with regard to microvascular complications, but is also associated with an increased risk of cardiovascular events**. Because randomized-controlled trials have shown that multifactorial care improves prognosis, the KDIGO guideline suggests a multi-pronged strategy that addresses different levels [1,4–7]. In the latest version of the KDIGO guidelines, the evidence base on sodium-glucose cotransporter-2 inhibitors (SGLT-2-i) and glucagon-like peptide-1 receptor agonists (GLP-1-RA) was added compared with the previous version, and a new section on mineralocorticoid antagonists (MRA) was added (Box ) [1]. If these currently available drugs are used in a timely manner, a significant slowing of renal function loss can be achieved and the overall prognosis can be improved, explained Frederik Persson, MD, Senior Research at Steno Diabetes Center Copenhagen (Denmark) [2]. As in previous guidelines, the recommendations are not limited to drug interventions, but again promote lifestyle factors and self-management as important components within multimodal disease management.
** e.g. myocardial infarction, cardiac arrhythmia or heart failure
| T2D and CKD: key recommendations of the 2022 KDIGO guidelines. |
| Under what conditions is an SGLT-2-i recommended as an add-on? Regarding glycemic control, metformin is still considered first-line therapy in type 2 diabetes (T2D) when the estimated glomerular filtration rate (eGFR) is ≥30 ml/min per 1.73 m2 but early addition of an SGLT-2-i is recommended: at an eGFR of ≥20 ml/min per 1.73 m2 SGLT-2-i can be initiated and, depending on tolerability, continued until dialysis or transplantation is initiated. In the previous version of the guideline, the eGFR threshold was still 30 ml/min per 1.73m2. |
| What is the situation regarding GLP-1 RA? When SGLT2-i and metformin are insufficient to achieve blood glucose goals, or when SGLT2-i or metformin cannot be used, GLP-1 RA are the preferred blood glucose-lowering drugs. |
| When should an MRA be prescribed? A selective nonsteroidal MRA (finerenone) may be added to first-line therapy for T2D and a high residual risk of renal disease progression and cardiovascular events. Specifically, with an eGFR ≥25 ml/min per 1.73m2, normal serum potassium concentration, and albuminuria (≥30 mg/g [≥3 mg/mmol]) despite maximum tolerated dosing of an RAS inhibitor (RAS inhibition is recommended for patients with albuminuria and hypertension). |
| What does the guideline say regarding statin therapy? It is recommended that the prescription of a statin be considered in all patients with T2D and CKD. |
| to [1,2] |
Screen T2D patients for CKD
Unlike cancer, there are no structured screening programs for chronic metabolic diseases such as diabetes, Dr. Persson pointed out [2]. However, considering that diabetes is the most common cause of chronic kidney disease (CKD), it is advisable to regularly assess risk factors for the development of nephropathy in type 2 diabetic patients receiving primary care, the speaker said [2]. The KDIGO guideline advises to determine eGFR and albumin creatinine ratio (ACR) at regular intervals as a prerequisite for the implementation of treatment recommendations [8]. Albuminuria is a very sensitive parameter for the diagnosis of chronic renal failure [9].
That a holistic approach to diabetes care and the importance of screening CKD risk patients propagated in guidelines bears fruit is shown by the example of a study from Denmark, where corresponding efforts have been intensified in recent years, the speaker reported [2]. Namely, researchers analyzed a large dataset of from three cross-sectional studies of type 2 diabetics (n=5592) conducted between 2009-2017. This found that the rate of annual ACR measurement in the context of general medical care increased from 57.2% to 82.8% during 2012-2020 [10]. Since CKD is often hardly associated with symptoms in the early stages, such screenings are an extremely important element in disease management.
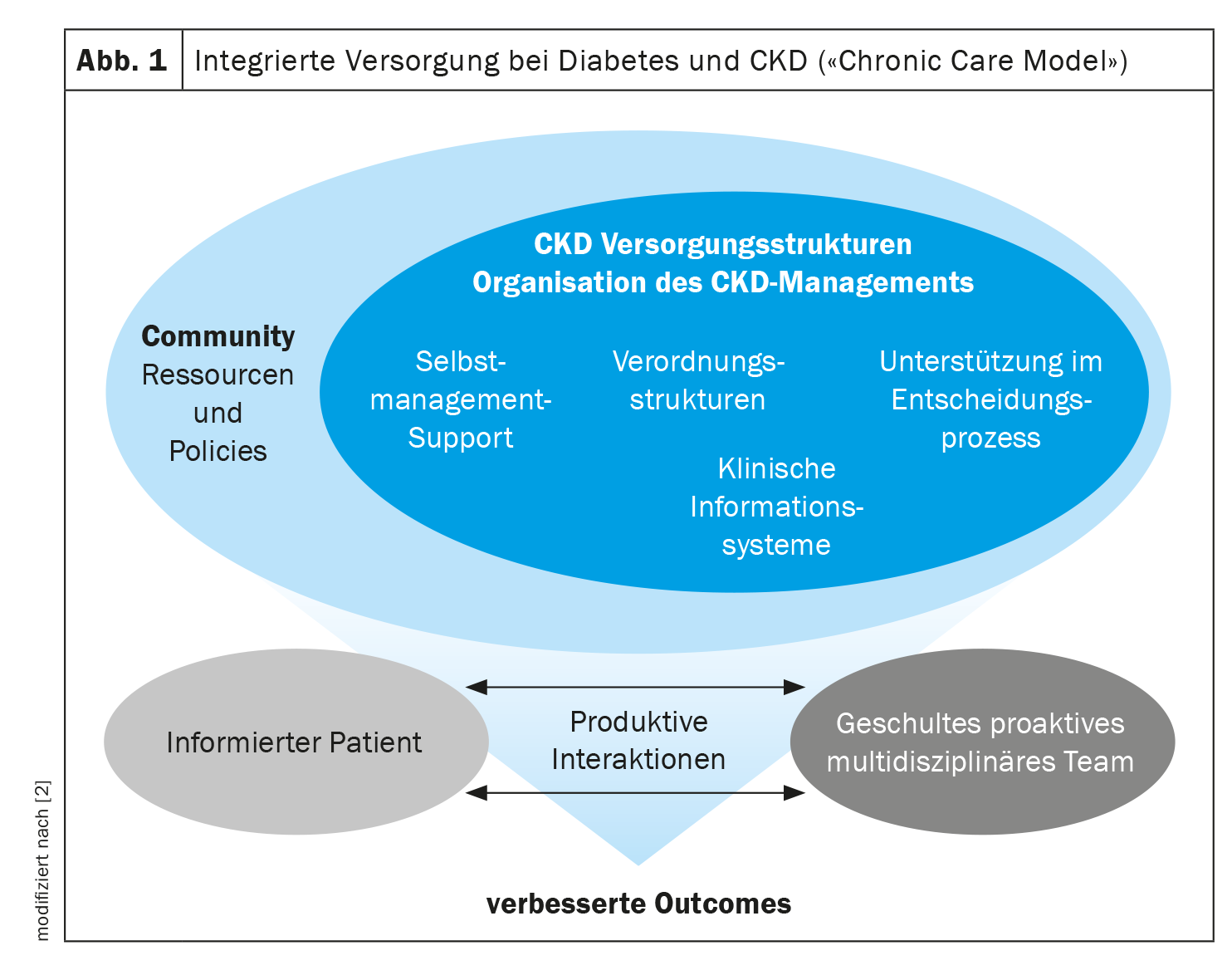
Integrated multidisciplinary care
In order to identify CKD at an early stage and to implement the recommendations of the KDIGO guidelines, collaboration between different actors in the health care system is necessary, Dr. Persson emphasized [2]. Barriers to successful implementation of guideline recommendations may be at several levels. The speaker pointed out that it is important to reflect on outdated ways of thinking and create evidence that the new treatment options are useful and sustainable. This can also take the wind out of the sails of the argument of high medication costs. After all, from a health economic perspective, delaying costly renal replacement procedures through timely initiated modern pharmacotherapies is a sustainable investment, according to a statement in the current KDIGO guidelines [1]. However, implementation of the optimal treatment strategy may also encounter barriers at the individual patient level. Here, motivational factors in particular are brought into the field. For example, there are patients who do not see why they should now take yet another medication [2]. Education is needed here by demonstrating the evidence-based benefits of each therapeutic regimen. In addition, Dr. Persson emphasized the importance of interdisciplinary collaboration and cited examples of successfully implemented integrated care systems (Fig. 1) in Denmark, Sweden, and the United Kingdom [2]. In each case, it was a patient-centered approach that had resulted in high patient satisfaction. A proactive multidisciplinary team is an important prerequisite, said the speaker, citing an example from everyday clinical practice at the Steno Diabetes Center: there, good experience has been made with the fact that at every second patient appointment, the examination by the general practitioner was coupled alternately with a consultation with the nephrologist or the endocrinologist. This not only facilitates the best possible patient care, but also promotes the interdisciplinary exchange of knowledge.
Congress: ERA Congress
Literature:
- Rossing P, et al.: Executive summary of the KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease: an update based on rapidly emerging new evidence. Kidney Int 2022; 102(5): 990–999.
- «Implementation of the KDIGO Diabetes Guideline for the European context», Dr. Frederik Persson, MD, Annual Congress of the European Renal Association Congress (ERA), 18.06.2023.
- Seidu S, et al.: 2022 update to the position statement by Primary Care Diabetes Europe: a disease state approach to the pharmacological management of type 2 diabetes in primary care. Prim Care Diabetes 2022; 16(2): 223–244.
- Chan JC, et al.: Effects of structured versus usual care on renal endpoint in type 2 diabetes: the SURE study: a randomized multicenter translational study. Diabetes Care 2009; 32: 977–982.
- Chan JCN, et al.: Effect of a web-based management guide on risk factors in patients with type 2 diabetes and diabetic kidney disease: a JADE randomized clinical trial. JAMA Netw Open 2022; 5: e223862.
- Gaede P, et al.: Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet 1999; 353: 617–622.
- Ueki K, et al.: Effect of an intensified multifactorial intervention on cardiovascular outcomes and mortality in type 2 diabetes (J-DOIT3): an open-label, randomised controlled trial. Lancet Diabetes Endocrinol 2017; 5: 951–964.
- de Boer IH, et al.: Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Diabetes Care. Published online October 3, 2022. https://doi.org/10.2337/dci22-0027, (last accessed Aug 31, 2023).
- Medix, www.medix.ch/wissen/guidelines/chronische-niereninsuffizienz,(last accessed Aug. 31, 2023).
- Persson F, et al.: Improving frequency of urinary albumin testing in type 2 diabetes in primary care – An analysis of cross-sectional studies in Denmark. Prim Care Diabetes 2021; 15(6): 1007–1011.
HAUSARZT PRAXIS 2023; 18(9): 43–44