Differential diagnosis plays an important role in the workup of epigastric pain. The correct interpretation of the leading symptom, pain pattern and localization can lead the way to successful therapy. There are a variety of possible causes ranging from liver, gallbladder or pancreatic diseases to ventriculi or duodeni ulcer. Frequently, however, no organ pathological findings are detectable at all in chronic abdominal complaints, since they are functional gastrointestinal disorders.
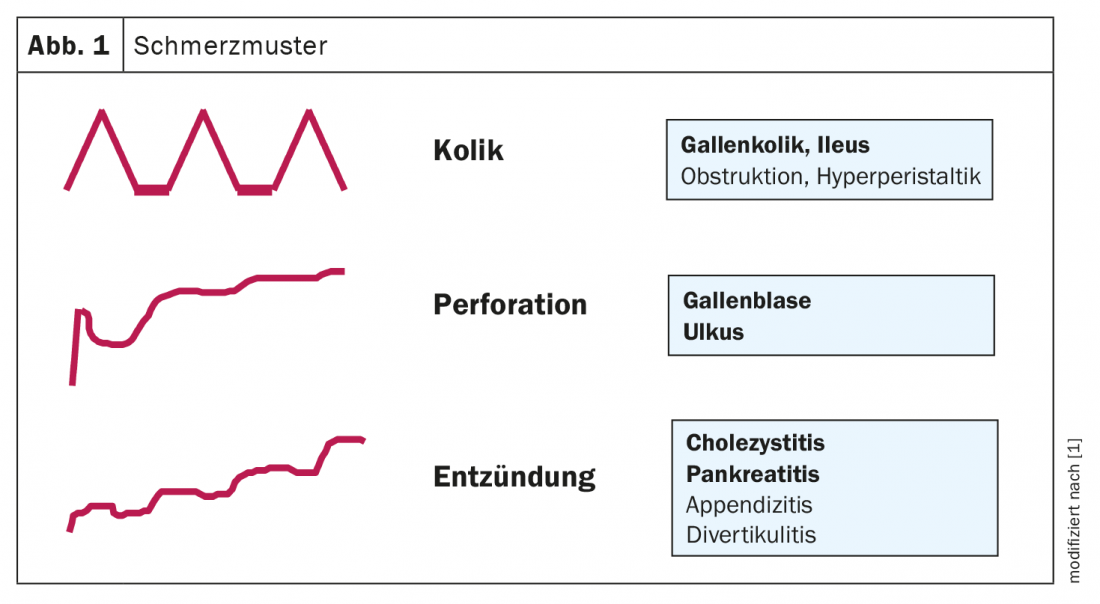
More than 50% of chronic recurrent abdominal pain is not due to organ pathology, explains PD Dr. med. Heiko Frühauf, Center for Gastroenterology and Hepatalogy AG, Zurich [1]. In addition to the temporal course of pain pattern and localization, it is crucial for the differential diagnostic assignment with what kind of leading symptom the upper abdominal pain is associated, said the speaker. Chronic recurrent epigastric pain may be accompanied by reflux symptoms or diarrhea. While the former suggests reflux disease or a functional gastrointestinal disorder, diarrhea is more likely to indicate irritable bowel syndrome or inflammatory bowel disease. Asking about the pain pattern is also an important part of taking the history (Overview 1, Fig. 1). Acute abdominal pain is typically a sharp pain, which is often accompanied by vomiting, and sometimes there is fecal retention. In the case of right-sided abdominal complaints, he said, liver or biliary diseases or even the pancreas should be considered first and foremost. An important leading symptom is the appearance of defensive tension (peritonitis), sometimes shock symptoms are added and sepsis, it is something that is usually seen in an acute emergency room.
Heartburn – gastroscopy if reflux symptoms are suspected
In patients complaining of heartburn and a feeling of pressure behind the sternum, the pain is typically localized to the epigastrium. The reflux symptoms can lead to esophagitis and usually occur intermittently after voluminous meals and also at night. It is important to differentiate from ulcer symptoms, functional diseases, esophageal spasms, and also from cardiac symptoms such as coronary artery disease. Gastroscopy with histology sampling is the mainstay of diagnostics, and functional diagnostics using ph-manometry to detect pathologic acid reflux in the esophagus is considered the gold standard.
Therapy consists of the administration of proton pump blockers (PPI); prokinetics may also be used if delayed gastric emptying is suspected .
Feeling of fullness – distinguish functional dyspepsia from irritable bowel syndrome
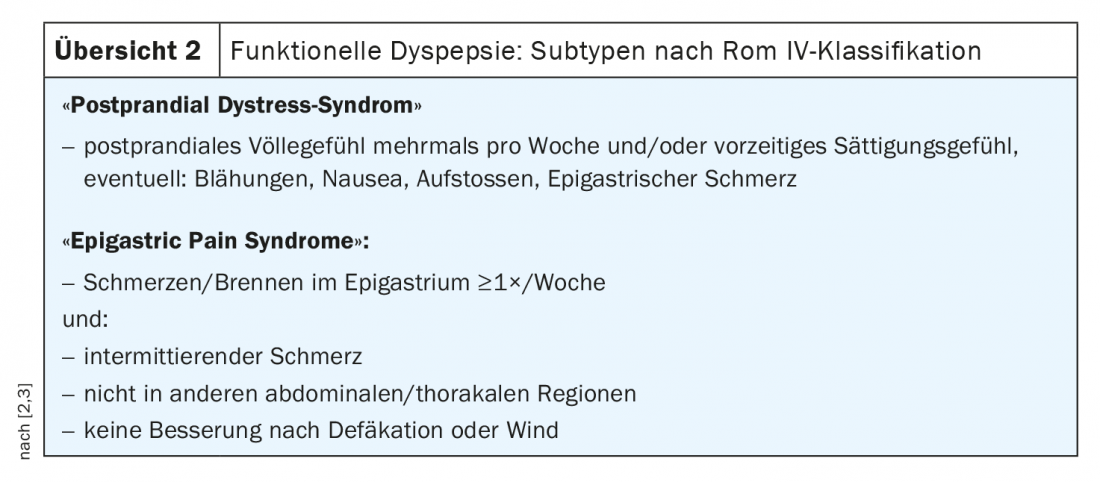
According to the ROM IV classification, Functional Dyspepsia is characterized by abdominal discomfort, early satiety respectively feeling of fullness and epigastric pain, for example in the form of a burning pain sensation in the upper abdomen or behind the breastbone. An important criterion is that the symptoms cannot be explained by an organic cause and have persisted for at least 6 months [2,3]. Functional dyspepsia is divided into two subtypes: “postprandial dystress syndrome” (dyspepsia of the motility type) and “epigastric pain syndrome” (syndrome with epigastric pain, formerly also: dyspepsia of the reflux type, overview 2) .
Dyspeptic complaints can also be caused by lactose intolerance or a bacterial imbalance. This is typically fluctuating, food-dependent pain. A lactose H2 breath test can provide with revealing diagnostic information. “And an important part of the diagnosis is a gastroscopy with the analysis of the duodenal juice, and specifically with the question of bacterial overgrowth,” adds the Dr. Frühauf. Treatment depends on the triggering cause; in the case of a significantly increased bacterial count in the small intestine, antibiotic therapy or an appropriate lactose-free diet may be necessary. Although the administration of lactase (Lacdigest®) [4] is not a standard therapy for lactose intolerance, it is an option, especially if the diet cannot be followed.
Postprandial complaints – ventriculi or duodenal ulcer possible
If the pain symptoms manifest themselves food-dependently postprandially, this indicates that it might rather be a ventriculic ulcer; if the pain occurs in the fasting state, for example at night, and improves after food intake, this is more indicative of the presence of a duodenal ulcer. Typical is a rather strong pain at the beginning, which increases in the course. Alcohol consumption is a classic trigger; in duodenal ulcers, Helicobacter pylori is also a possible bacterial cause. Differential diagnoses include coronary or cardiac problems, but also radicular or musculoskeletal pain. “Diagnosis is made by gastroscopy with histology sampling, and treatment again consists of administration of proton pump blockers (PPI) and, if necessary, Helicobacter pylori eradication if detected,” Dr. Frühauf summarizes. Ulcers and reflux diseases account for about one-third of all causes of dyspeptic complaints, and in about 60% of cases they are functional gastrointestinal complaints. It should be mentioned in the patient interview that often no organ pathological findings are detectable.
Nausea and vomiting – biliary colic?
In biliary colic, symptoms are typically localized to the right side of the upper abdomen, possibly radiating to the shoulder area or back. “If you can elicit such a pain localization on examination and history, you need to think about gallstones,” the speaker explained. There are also rare forms, for example, when a gallstone is lodged in the infundibulum of the gallbladder and squeezes the bile duct. The pain symptomatology is typically colicky. The pain starts postprandially, lasts for about 1-4 hours, then subsides, and later returns.
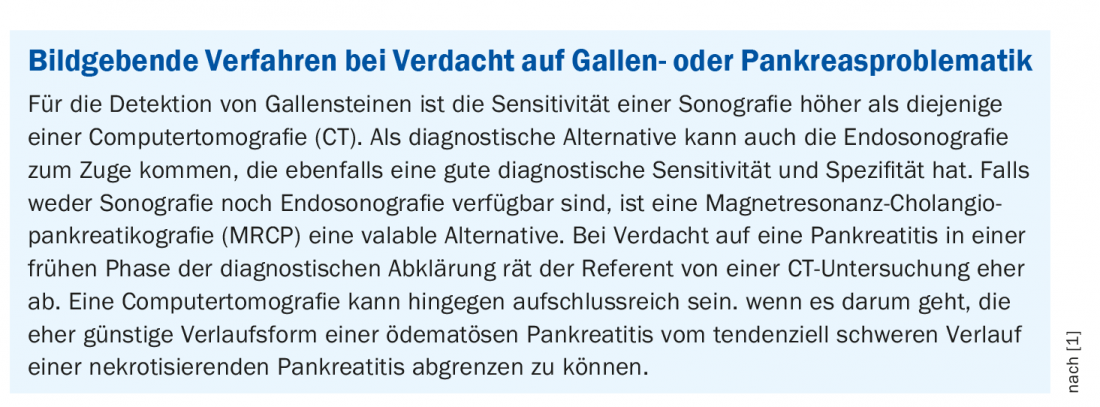
The mainstay of diagnosis of gallstone disease is abdominal sonography, with endosonography and magnetic resonance cholangiopancreaticography (MRCP) when appropriate. With regard to therapy, Dr. Frühauf initially recommends antispasmodic substances (e.g. Buscopan®) or non-steroidal anti-inflammatory drugs (NSAIDs) such as Novalgin® [4] for pain relief. To permanently relieve patients of their symptoms, gallstones in the bile duct must be removed endoscopically. In cases of colic due to stones in the gallbladder, the entire gallbladder is removed, including the stones inside (cholecystectomy). It is one of the most commonly performed operations in visceral surgery.
Fever – cholecystitis or pancreatitis?
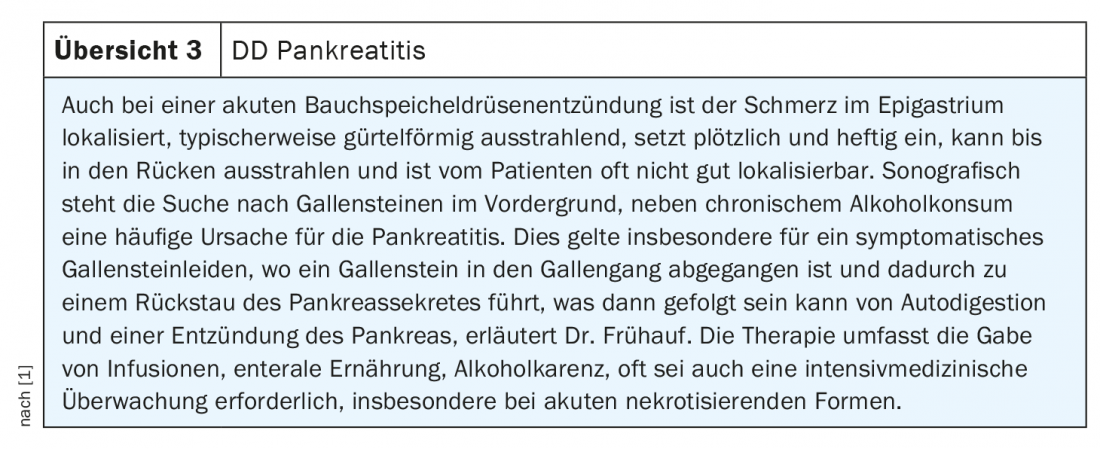
If upper abdominal pain is accompanied by fever as a leading symptom, cholangitis or even cholecystitis should be considered. “The pain typically increases slowly but steadily as inflammatory pain, still sets in acutely, but not quite as acute or severe as perforation,” explains Dr. Frühauf (Fig. 1). Ultrasound examination plays an important role in diagnostic methods; other imaging methods may also be used if necessary (Box). Furthermore, a positive Murphy sign is considered indicative. It is important to differentiate other inflammatory diseases such as pleurisy or pneumonia. “If you have sonographically diagnosed this typical three-layered wall, wall thickening and pressure pain, you should also initiate therapy immediately. Initiation of cholecystectomy in the acute phase,” the gastroenterologist explains. It has been scientifically proven that one should not wait until the inflammation improves. “In other words, that’s where interdisciplinary management is required early on for primary care physicians and internists,” Dr. Frühauf emphasizes. An important differential diagnosis is acute pancreatitis (review 3).
Source: FomF General and Internal Medicine
Literature:
- Frühauf H: Upper abdomen: pressure and pain. PD Dr. med. Heiko Frühauf, FomF General and Internal Medicine, Zurich, 05.12.2020.
- Stanghellini V, et al: Gastroduodenal Disorders. Gastroenterology 2016; 150: 1380-1392.
- Talley NJ, et al: Functional dyspepsia. Curr Opin Gastroenterol 2016; 32: 467-473.
- Swiss Drug Compendium, https://compendium.ch/ (last accessed 01.03.2021).
FAMILY DOCTOR PRACTICE











