In more than half of all patients with plaque psoriasis, there is an infestation of the nails . In addition, nail involvement is considered a clinical warning signal for the development of psoriatic arthritis. Topical therapies alone are often insufficient. The use of highly effective biologics makes it possible to achieve good symptom control even in severe forms of the disease. However, it often takes a little longer for the full effects of treatment to develop than for skin symptoms.
Nail psoriasis affects 50-79% of patients with cutaneous psoriasis and up to 80% of those with psoriatic arthritis [1]. The appearance of nail changes is often perceived as stigmatizing and usually leads to a significant reduction in quality of life. Typical clinical features of nail involvement include subungual hyperkeratosis, onycholysis, spotted and oily nails. The infestation of the nails can occur on one as well as on several fingers and toes and, if left untreated, can lead to loss of the nail. Histological and mycological clarification may be useful for the differential diagnosis of fungal infections. The NAPSI score is recommended to assess the severity of psoriasis on the fingernails and toenails.
Screen for psoriatic arthritis when nails are affected
Nail psoriasis is more often associated with longer disease duration, psoriatic arthritis, and severe skin symptoms compared with plaque psoriasis without nail involvement [2]. That nail psoriasis may be a predictor for the subsequent development of psoriatic arthritis is shown by the fact that many affected individuals have subclinical enthesiopathy [3]. This is important to consider, emphasizes Alexander Egeberg, MD, Herlev and Gentofte Hospital, Copenhagen (DK). Because of the high association with psoriatic arthritis, patients with nail psoriasis should always be evaluated for possible joint involvement [8].
Consider biologics for severe forms of nail psoriasis.
The treatment of nail infestations remains a therapeutic challenge, and topical therapies alone are often not sufficiently effective. Systemic therapy for nail psoriasis should be considered especially in cases of concomitant severe skin involvement, PsA, or severe nail involvement (NAPSI* >10) with severely impaired quality of life or functional limitations [4,5].
* NAPSI = Nail Psoriasis Severity Index
Both biologics and certain conventional systemic therapies have demonstrated efficacy in nail psoriasis, but the extent of clinical improvement varies. Biologics can now also be used to effectively treat severe forms of nail psoriasis, although treatment success is slower in the case of nail infestation than in the case of skin lesions. Dr. Egeberg supports the use of biologic systemic agents in psoriasis patients with nail involvement and states that there is evidence that biologic therapy reduces the incidence risk of psoriatic arthritis in those affected.
Individual benefit-risk profile as selection criterion
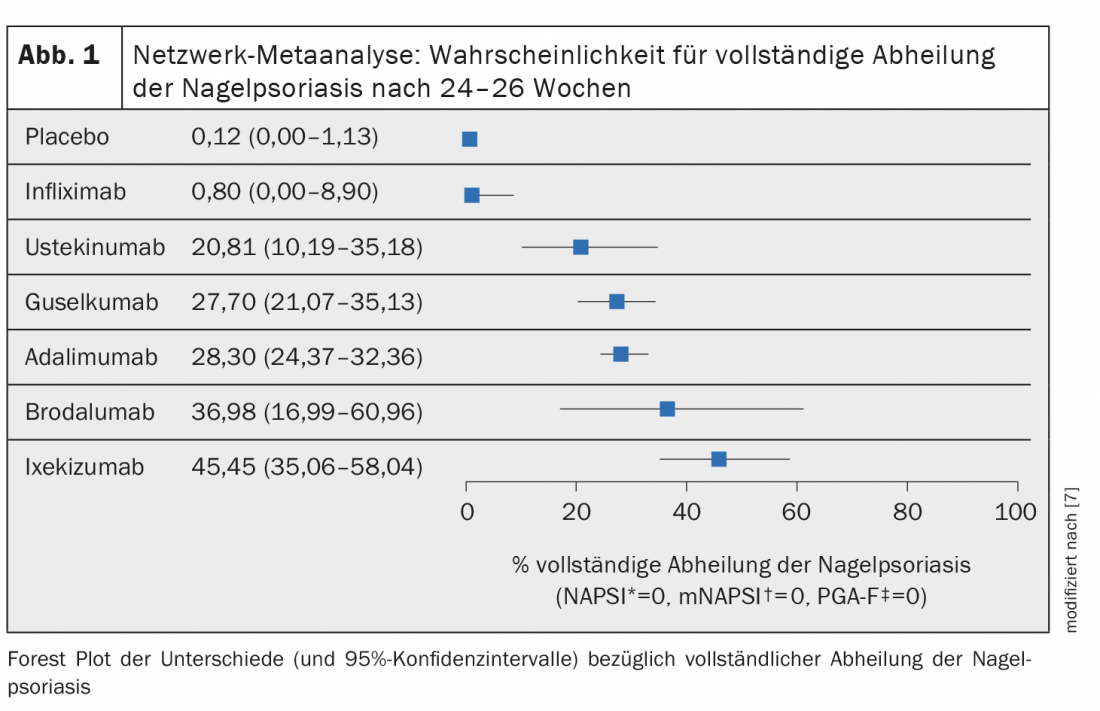
Network meta-analyses could be used to make indirect comparisons of the efficacy of different drugs. Reich et al. have calculated the probability of achieving complete healing (NAPSI*=0, mNAPSI#=0, PGA-F**=0) at 24-26 weeks in their network meta-analysis for six biologics [7]. All of the included biologics except infliximab were shown to be superior in placebo comparisons, including ixekizumab (anti-IL-17) and guselkumab (anti-IL-23) (Fig. 1). The results of another network meta-analysis confirm that biologics are an effective treatment option in psoriasis patients with nail infestation [7]. When deciding on therapy, it should be borne in mind that the treatment of psoriasis and its various manifestations should always be tailored to the individual findings and level of suffering, and possible comorbidities should also not be disregarded. Nail infestation is particularly common in patients with psoriatic arthritis.
# mNAPSI = modified NAPSI
** PGA-F= Physician’s Global Assessment of Fingernail Psoriasis.
Congress: European Academy of Dermatology and Venereology
Literature:
- Bardazzi F, et al: Nail Psoriasis: An Updated Review and Expert Opinion on Available Treatments, Including Biologics. Acta Derm Venereol 2019; 99(6): 516-523.
- Augustin M, et al: Nail psoriasis in Germany: epidemiology and burden of disease. Br J Dermatol 2010; 163(3): 580-585.
- Ash ZR, et al: Psoriasis patients with nail disease have a greater magnitude of underlying systemic subclinical enthesopathy than those with normal nails. Ann Rheum Dis doi:10.1136/annrheumdis-2011-200478
- de Vries AC, et al: Interventions for nail psoriasis. Cochrane Database Syst Rev 2013 (1): CD007633
- Sánchez-Regaña M, et al. (en representación del Grupo Español de Psoriasis de la Academia Española de Dermatología y Venereología): Evidence-based guidelines of the Spanish psoriasis group on the use of biologic therapy in patients with psoriasis in difficult-to-treat sites (nails, scalp, palms, and soles). Actas Dermosifiliogr 2014; 105(10): 923-934.
- Huang IH, et al: Small molecule inhibitors and biologis in treating nail psoriasis: a systemic review and network meta-analysis. J Am Acad Dermatol 2021; 85: 135-143.
- Reich K, et al: Network meta-analysis comparing the efficacy of biologic treatments for achieving complete resolution of nail psoriasis. J Dermatolog Treat 2021 Mar 1; 1-9.
- Egeberg A: Treatment of Nail Psoriasis: Choosing the right biologic. Alexander Egeberg, MD, EADV Annual Meeting, Sept. 29-Oct. 2, 2021.
- “Psoriasis can also affect the nails,” BVDD, www.bvdd.de/aktuelles-presse/presse-newsletter/details/schuppenflechte-kann-auch-die-naegel-befallen, 04/2018 (last accessed Jan. 06, 2022).
DERMATOLOGIE PRAXIS 2022; 32(1): 18-20 (published 7.2.22, ahead of print).