In an international comparison, Switzerland is one of the countries with the lowest consumption of antibiotics. Nevertheless, there is still room for improvement in this country too. Analyses show that five potentially self-limiting infections account for around 80% of antibiotic prescriptions in the outpatient sector. At the SGAIM Autumn Congress, the current situation was highlighted and tools were presented that can help to reduce antibiotic consumption.
“The WHO considers antibiotic resistance to be one of the biggest health problems of the 21st century,” reported Simon Gottwalt, Head of Human Resources for the Swiss National Strategy on Antibiotic Resistance at the Federal Office of Public Health (FOPH) [1]. According to the World Health Organization (WHO), antimicrobial resistance is one of the “Top 10 Public Health Threats” [1]. An estimated 1.3 million people worldwide die every year from infections with resistant pathogens; this is also referred to as a silent epidemic. “Antibiotic prescribing in Switzerland is already relatively low, but there is still room for improvement, especially in certain indications that are responsible for a large proportion of antibiotic prescriptions,” said the speaker [1]. These include acute otitis media, tonsillopharyngitis, uncomplicated urinary tract infections, bronchitis and sinusitis.
Swiss National Strategy on Antibiotic Resistance (StAR)
In order to prevent the emergence of new resistances and limit their transmission and spread, the Swiss National Strategy on Antibiotic Resistance (StAR) has been launched in Switzerland [1,2]. This is a “One Health” approach, with the main objective being to maintain the effectiveness of antibiotics for humans and animals. The four federal offices FOPH (Federal Office of Public Health), FSVO (Federal Food Safety and Veterinary Office), FOAG (Federal Office for Agriculture) and FOEN (Federal Office for the Environment) are pursuing this common goal on a cross-sectoral basis and in cooperation with the stakeholders concerned. In 2022, outpatient medical care accounted for 86% of all antibiotic prescriptions in Switzerland. This shows that, as in other countries, the majority of antibiotic prescriptions are made in the outpatient sector. Antibiotic consumption is calculated on the basis of defined daily doses per 100,000 inhabitants. Further information on antibiotic consumption and the antibiotic resistance situation in Switzerland can be found in the Swiss Antibiotic Resistance Report 2022 (Overview 1) [3]
| Overview 1: Important tools for the appropriate use of antibiotics |
| The National Strategy on Antibiotic Resistance Switzerland (StAR) aims to prevent the emergence of new resistances and to limit their transmission and spread. |
| The “Swiss Antibiotic Resistance Report (SARR) is the national report published every two years on the situation of antibiotic resistance in Switzerland. |
| The Sentinella network , which monitors prescriptions, has been integrated into the SARR in the human medicine sector. |
| With the application ANRESIS Guide application from the Swiss Center for Antibiotic Resistance displays the current resistance data clearly and intuitively. This supports the use of antibiotics tailored to the local resistance situation. The SSI guidelines are also linked |
| The Swiss Society of Infectious Diseases (SSI) regularly develops and publishes guidelines as an aid to optimizing the use of antibiotics in line with the latest knowledge; Link to the current national antibiotic prescribing guidelines. |
| The publication “Development of tools to implement shared decision-making for guideline-recommended antibiotic prescriptions in primary healthcare physician practices in Switzerland” [7] provides a lot of useful information on the topic of “Shared decision making” and can be downloaded from the homepage of the Bern Institute of Family Medicine can be downloaded |
Around half of all antibiotic prescriptions could be avoided
The more and inappropriately antibiotics are prescribed, the more resistance there is. “This also applies to the outpatient sector,” says Gottwalt [1]. Current analyses show that significantly fewer antibiotics are prescribed in German-speaking Switzerland than in French-speaking Switzerland or Ticino. But there is also potential for improvement in German-speaking Switzerland. It is estimated that around 50% of antibiotic prescriptions could be avoided. In 2017, the results of a nationwide survey of Swiss GPs were published [4]. 250 doctors responded and provided 9961 patient files. In total, 32.1% of patients were prescribed antibiotics. For tonsillitis/pharyngitis, acute otitis media, acute rhinosinusitis and acute bronchitis, the prescribing rates of 44.4%, 69.6% and 47.4% respectively clearly exceeded the specified maximum value of 20%, and for acute bronchitis the rate of 41.5% was well above the target maximum value of 30% [4].
What about the choice of antibiotics prescribed?
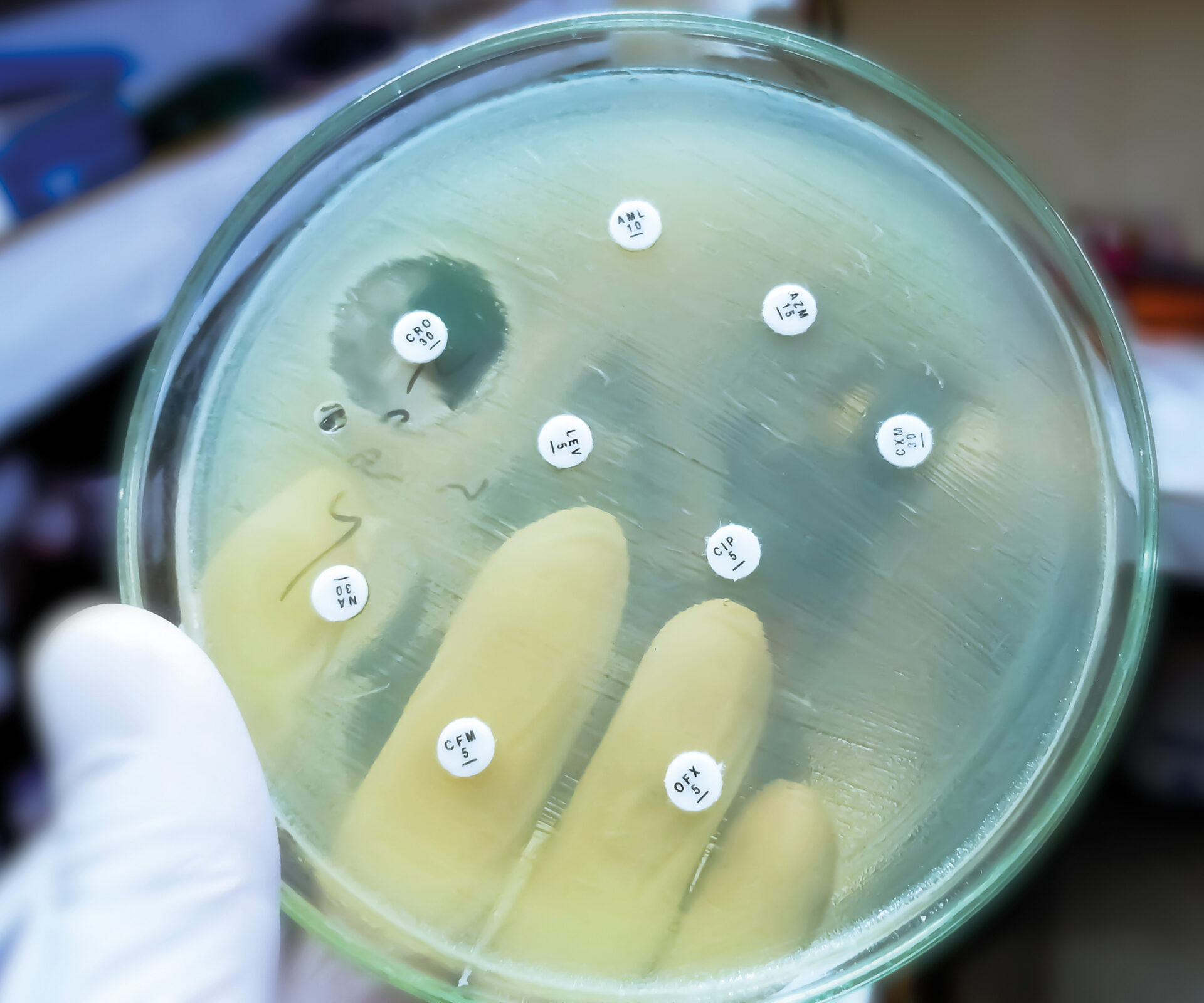
In addition to the frequency of antibiotic prescriptions, it also plays a role which antibiotic agents are prescribed. The study by Glinz et al showed that the proportion of non-recommended antibiotics was above the recommended maximum of 20% (31.5-88.7% for all conditions) for all diagnoses mentioned and 37.2% of women with UTIs were prescribed quinolones, which is well above the recommended maximum of 5% [4]. Figures from the Sentinella reporting system also show that fluoroquinolones are frequently prescribed for uncomplicated urinary tract infections, which should not be the case according to the guidelines, Gottwalt explained [1]. There is also still potential for optimization in the choice of antibiotics in the paediatric field: Around 70% of antibiotic prescriptions in children relate to upper respiratory tract infections. The recommended (simple) penicillins or aminopenicillins are not always used for this purpose. Macrolides, which have a problematic profile for the selection of resistance, are probably used too frequently for the treatment of respiratory tract infections [5]. The current national antibiotic prescribing guidelines were presented by Prof. Dr. med. Stefan Kuster, Chief Physician, Clinic for Infectiology/Hospital Hygiene, Cantonal Hospital St. Gallen. These and other practice-relevant aids for rational and appropriate prescribing of antibiotics are linked in Overview 1 [6].
Congress: SGAIM Fall Congress
Literature:
- «Antibiotic prescription in primary care: Current situation and relevance for Switzerland», Simon Gottwalt, SGAIM Herbstkongress, 21.–22.09.2023.
- Swiss National Strategy on Antibiotic Resistance (StAR), www.star.admin.ch/star/de/home/sarr/sarr.html,(last accessed 29.11.2023)
- Swiss Antibiotic Resistance Report (SARR),
www.star.admin.ch/star/de/home/sarr/sarr.html,(last accessed 11/29/2023) - Glinz D, et al.: Quality of antibiotic prescribing of Swiss primary care physicians with high prescription rates: a nationwide survey. J Antimicrob Chemother 2017; 72(11): 3205–3212.
- “How are antibiotics prescribed in Switzerland today? ” www.bag.admin.ch/bag/de/home/krankheiten/infektionskrankheiten-bekaempfen/antibiotikaresistenzen/wie-werden-heute-in-der-schweiz-antibiotika-verschrieben.html,(last accessed 29.11.2023)
- «Nationale Antibiotika-Verschreibungsrichtlinien: Was ist neu, was ist geplant?», Prof. Dr. med. Stefan Kuster, SGAIM Herbstkongress, 21.–22.09.2023.
- «Konsultationshilfsmittel für Praxen und Qualitätszirkel», Dr. Dr. med. Adrian Rohrbasser, SGAIM Herbstkongress, 21.–22.09.2023.
HAUSARZT PRAXIS 2023; 18(12): 34–35