Immune disturbance appears on skin as a consequence of immunosuppression. The article describes a panel of cutaneous disorders occurring in immunosuppressed HIF infected pateients and follow the trends of the epidemy profile in patiens living and aging with a chronic, treated infection.
For more than 30 years now, HIV infection has spread all over the world and has become one of the most challenging human health fights against an infectious agent. Actually, we are used to meet well controlled HIV patients who consult us for the same problems like immunocompetent individuals. At the beginning of the HIV epidemic dermatologists were largely involved in the diagnosis and management of AIDS patients, particularly before the use of highly active antiretroviral therapy. Immune disturbance appears on skin as a consequence of immunosuppression, and opportunistic agents present skin tropism [1–3]. When antiretroviral therapy (ART) was introduced widely, new problems concerning the skin emerged: adverse drug reactions to antiretrovirals, lipodystrophy syndrome, and cancers. We will not point out HIV as STI and associated specific prevention, which is a topic itself that could fill another article. We hereby will describe a panel of cutaneous disorders occurring in immunosuppressed HIV infected patients and follow the trends of the epidemy profile in patients living and aging with a chronic, treated infection.
The clinical signs directly related to HIV or directly linked to immunity loss
These manifestations are mostly inflammatory and should particularly warn any physician. Some are not completely understood and other pathophysiological mechanisms apart from a simple drop in CD4 count have been suggested [2].
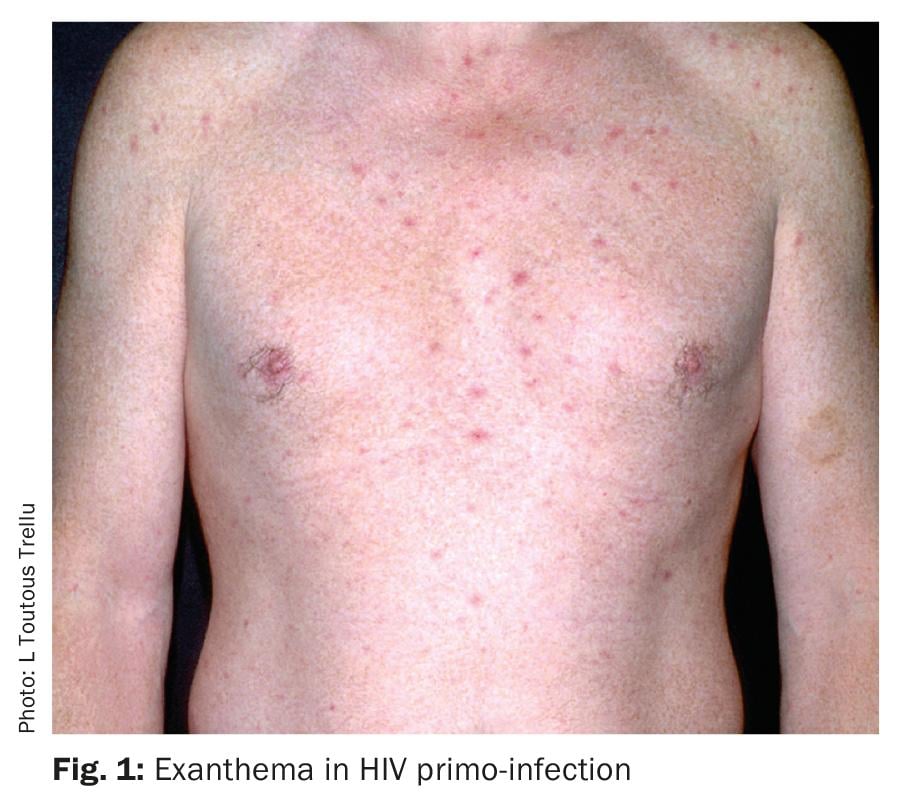
HIV Primo-infection: Primo-infection is expressed clinically in almost half of cases. The typical exanthema occurs in 70% of the clinical manifestations and has been well described as erythematous macules on the trunk, face and limbs; often associated with mucous ulcers in the genital or buccal area. It is associated with fever, pharyngitis, myalgias, arthralgia, fatigue suggestive of a flu syndrome with exanthema or mononucleosis syndrome [4]. Differential diagnosis with other viral eruptions or drug adverse events may be difficult, but in adults, the anamnesis should quickly eliminate them. If not, HIV testing should be proposed. The most common association is secondary syphilis; the two microbial agents may be contracted together in an at-risk sexual context.
The physiopathology of the virus in the skin has not been reported in the acute phase. In chronic HIV infection, several hypotheses regarding the virus’ relationship and consequences on the skin have been reported [2] (Fig. 1).
Pruritic papular folliculitis: This entity is regularly encountered in AIDS patients or those with a low CD4 count (<200/mm3). The dermatosis is localized on the face and trunk, sometimes mimicking benign excoriated acne. However, the extent of itching and the presence of macular and urticarial plaques mixed with the pustules and crusts help to diagnose HIV-associated dermatosis. Its occurrence is either related to low immunity or to the immune reconstitution inflammatory syndrome. Management and evolution over time is driven by response to ART, and symptoms are relieved by topical anti-inflammatory drugs such as steroids and calcineurin inhibitors [5]. A skin biopsy confirming the diagnosis of HIV-specific papular pruritic folliculitis is recommended, because of the differential diagnosis of bacterial, fungal or viral (herpetic) folliculitis or lymphoma (Fig. 2).

Itch and prurigo: Itch in HIV may be related to xerosis, which is present in almost 50% of patients. Nutritional and neurological etiologies may be involved. Some cases seem to be linked to the HIV RNA load in the peripheral blood. Viral hepatitis C coinfection is an aggravating factor. It is known that active uncontrolled HVC infection induces pruritis, independently of any cholestasis or renal insufficiency. Atopic dermatitis can appear at any stage of HIV infection, but typically presents when immunity is still high or has been recovered under ART.
The management of resistant and disseminated itch, either sine materia or including prurigo lesions, include the use of topical steroids, anti-histamines, tricyclic antidepressant drugs and Ultra Violet A or B light phototherapy are classically used while awaiting immune- and HIV-control under antiretroviral.
Red fingers: Patients present distal finger erythema associated with telangiectasia different from the small angiomas seen in liver cirrhosis. Many cases were coinfected with hepatitis C virus. Since the advent of HVC-efficient treatments and HIV control, we rarely encounter patients with red fingers [6].
Pigmentation modifications: Skin pigmentation disorders are observed during chronic viral infection and may present as diffuse cutaneous hypopigmented plaques associated with vitiligo, or localized on the nails or mucous membrane. Diffuse body hyperpigmentation was observed in very sick, untreated immunosuppressed patients (Fig. 3).

Several mechanisms have been suggested, such as endocrine dysregulation and nutritional deficiency. Nail hyperpigmentation associated with zidovudine and localized patchy hyperpigmentation associated with emtricitabine (another nucleoside analogue) are well known and still regularly diagnosed under the new antiretroviral associations.
Seborrheic dermatitis: Seborrheic dermatitis is one of the most frequent cutaneous signs with xerosis in HIV infection, and is observed in up to 40% of seropositive patients, and up to 80% of patients with AIDS. When HIV status is unknown in the presence of severe seborrheic dermatitis, general practitioners or dermatologists should request a HIV test.
Psoriasis: The prevalence of psoriasis in HIV-1 seropositive individuals is similar to that of their seronegative counterparts. However, psoriasis lesions in AIDS tend to be more severe, with palmo-plantar and inverse-pattern lesions that can be extensive and recalcitrant. Onset of psoriasis in an individual at risk for HIV disease may be an indication for HIV testing. Psoriatic arthritis and Reiter’s syndrome in HLA B27 carriers are more frequent in HIV infected patients, and clinical manifestations are severe. A dramatic improvement of cutaneous psoriasis is observed under ART. This highly sensitive variation to immunity fluctuation may be explained by the etiology associated with lymphocyte activation in psoriasis. Treatment of psoriasis in HIV well controlled patients follows the same recommendations like in HIV-negative patients; anti-TNF biologics have been adequately prescribed.
Opportunistic infections and AIDS-defining diseases
This part illustrates the severity of disease. These skin disorders are actually encountered in patients from endemic areas without access to ART, in patients tested to late for HIV or non adherent to treatment because of social or psychological troubles.
Common bacterial infections: Recurrent superficial or deep folliculitis, furoncles, abcesses associated to Staphylococcus sp or streptococcus sp are the most common skin infections when immunity is low.
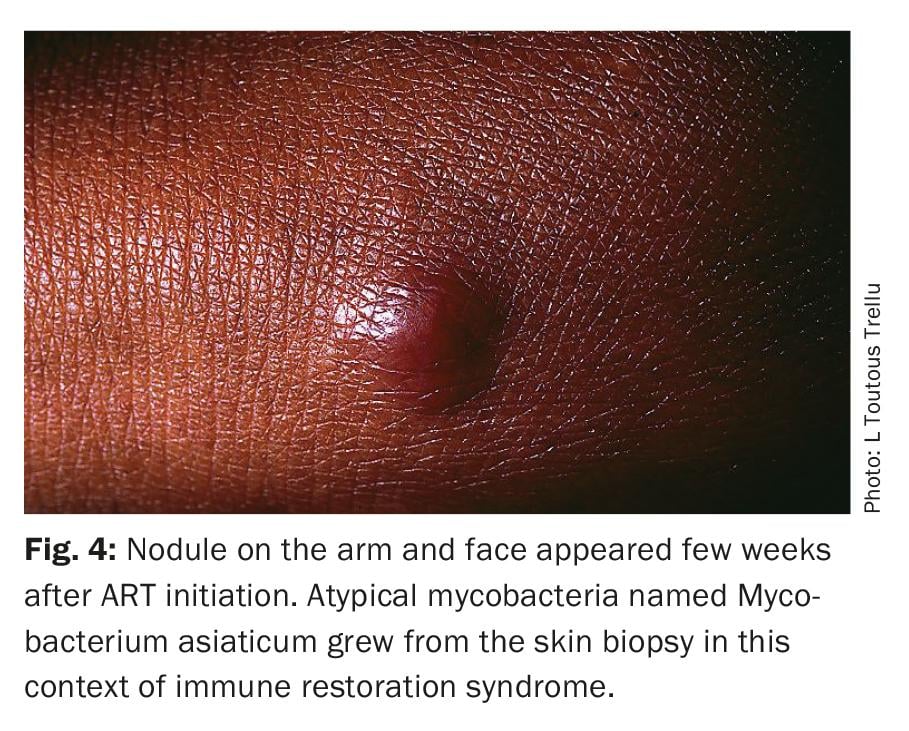
Atypical mycobacteria: Many species of atypical mycobacteria have been isolated from AIDS patients. Most involve blood, chest or abdominal organs. Cutaneous lesion may occur in disseminated infections ressembling as septic emboli lesions, and may appear locally (Fig. 4).
Fungus and parasitic infections: When the host is fragile, dermatophytes, molds and yeasts grow more on the nails, feet, hands and skin folds. Extensive and resistant local nail hypertrophy, leuconychy or skin plaques are common in AIDS. Diffuse oral candidiasis has become one of the clinical pictures of AIDS. Patients suffer from dysphagia. Candida albicans resistance can occur, and other resistant species of Candida such as parapilosis or glabrata grow. Bacteria folliculitis is the most frequent but Candida sp or Pityrosporon sp folliculitis may be identified when the CD4 count is very low. Systemic treatments using fluconazol or itraconazol are needed and topical antifungal drugs are preferred when lesions are superficial or localized.
Histoplasma sp and Cryptococcus neoformans have a disseminated expression in severely immunosuppressed HIV patients. Cutaneous involvement allows a quick microbiological and histological diagnosis.
The protozoan Leishmania sp may be very extensive and treatment challenging in immunocompromised HIV+ patients.
Viruses
Herpes simplex virus (HSV): Herpes simplex virus infections are very common, most of them are genital with frequent recurrences. Harboring HSV2 is associated with a higher risk of acquiring HIV. Each herpetic clinical event should be treated bearing in mind that HSV induces contagious muco-cutaneous lesions. An exceptional presentation of HSV can be a clinical and/or a virological-resistant chronic HSV (Fig. 5) – that means a muco-cutaneous genital lesion which lasts more than four weeks and which does not heal despite standard oral acyclovir treatment. A specific management is recommended [7].

Varicella zoster virus (VZV): Varicella zoster virus infection is probably the most frequent viral infection after HSV. Again, when this infection occurs in an individual under the age of 50 with HIV status unknown, he/she should be urgently tested for HIV. Atypical clinical presentations have been described, including necrotic, extensive and chronic VZV.
Ebstein Barr virus (EBV): In benign oral hairy leukoplakia (OL) the virus is isolated in a replicative form by superficial tongue biopsies. Lesions completely disappear with immunity improvement. Malignant side of EBV shows EBV in B lymphocytes and has been closely associated with occurrence of B lymphoma in HIV positive individuals. A 100% association with EBV is known for brain B lymphoma in these patients.
Molluscum contagiosum: Molluscum contagiosum is usually seen in immunocompetent children aged two to seven years, or in the armpits, inner thighs or pubis in young adults (<25 years old). In sexually active young adults, a HIV test is recommended. When molluscum contagiosum is present in patients known for HIV, it reflects a severe immunosuppression. Atypical forms – sometimes presenting as a tumor – or extensive forms have been described. A histological confirmation is necessary in order to eliminate disseminated opportunistic infections resembling this benign cutaneous infection, e.g. cryptococcus neoformans, histoplasma sp. The recovery of immunity under HAART is the main treatment objective even if surgical treatment to esthetic ends is required.
Human Papilloma virus (HPV): With increasing immunodeficiency, HPV infection emerges from latency, presenting clinically as verruca, condylomata acuminata (genital warts), in situ squamous cell carcinoma or invasive carcinoma. There is an increasing variety of HPV and among these, oncogenic HPV occurs with more advanced immunosuppression.
Epidermodysplasia verruciformis-like syndrome: An epidermodysplasia verruciformis-like syndrome has been described in HIV infected patients. The description is similiar to the congenital epidermodysplasia verruciformis which is characterized by hypopigmented macules or erythematous papules on the face, arms and trunk and associated with HPV types 5, 8, 17 and 20. Malignant transformation to a squamous cell carcinoma is common. Anal and cervico-vaginal HPV remain a permanent management challenge for any physician with HIV patients, because the virus keeps a strong oncogenic pathogenecity despite ART [8]. The rate of anal neoplasia is almost twice as high in HIV-infected versus seronegative men who have sex with men (MSM). High grade ano-genital neoplasia has also been also reported more often in HIV positive than HIV negative women. Close follow-up and local surgical treatments (cryosurgery, laser, electro-surgery, surgery) are necessary. Additionally topical 5-Fluoro uracil, or immunomodulator imiquimod should be regularly applied on small or extended lesions. Studies recommend the HPV preventive vaccination in this high risk population [8].
Human Herpes Virus 8 (HHV8) Kaposi sarcoma: An exciting discovery was made in the early ART era in 1994 when Chang et al. showed the association of kaposi sarcoma with a virus classfied in the herpesviridae family, namely Human Herpes Virus 8 (HHV8) [9]. The tumor had a high morbidity and mortality rate among men having sex with men and African patients. The sarcoma’s evolution closely follows that of immunity. When immunity is very low, sarcoma invades the skin, lymphatic nodes, chest and serous cavity. Thus, CD4 count improvement and stabilization remains the main therapeutic objective in the absence of a specific treatment against the virus. Prognosis factors are CD4 count and early diagnosis in a localized clinical stage. HHV8 viremia was also shown as a prognosis factor. Cytotoxic chemotherapy (doxorubicin, bleomycin, vincristin), vascular proliferation modulators or inhibitors (taxanes) are used in most severe cases in addition to ART. The only complete remission is observed in individuals with AIDS-kaposi sarcoma who quickly achieve good immunity control. In South and West Africa, the disease led to >50% mortality, despite well conducted ART with associated chemotherapy (Fig. 6).

Castleman’s disease and primary effusion lymphoma are the other severe diseases associated with HHV8. They are exceptional in HIV negative individuals.
Management of skin disorders in HIV infection
With the decrease in opportunistic diseases, the need for specialists and specific organ diagnosis and management also decreased. We propose four main targets for a dermatologist who care the chronic infection.
- Diagnose and manage cutaneous adverse drug reactions.
Several generations of drugs: In the first years of epidemy, cutaneous drug reactions were very common. The relation with immunosuppression and the higher risk of developing drug intolerance was largely reported. Drugs involved were those used in toxoplasmosis and prophylaxis and treatment of pneumocystis, such as sulfadiazine, trimethoprim-sulfamethoxazole, dapsone and aminopenicillin, frequently used in repeated bacterial infections in these patients. First antiretrovirals did not show frequent toxidermia, except hyperpigmentation and zidovudine (see above). In 1998 years, new antiretroviral molecules such as effavirenz, nevirapine and abacavir induced more frequently severe toxidermia and lead to rigorous follow-up.
The case of abacavir remains very interesting in the pharmacology history: genetic association between HLA-B*5701 and abacavir hypersensitivity syndrome is one of the strongest to be found for a drug. Since the description of this genetic basis, systematic screening of HLA-B*5701 is proposed to any HIV positive patient who requires abacavir [10]. Since 2010 new molecules such as integrase inhibitors, new protease inhibitors and nucleosides analogues are much less toxic. However any cutaneous adverse reaction under these drugs should imply a well documented pharmacovigilance notification (photographies, biopsies).
Lipodystrophy syndrome: The lipodystrophy syndrome was described in treated HIV patients in 1998, a few months after the use of antiretroviral associations with protease inhibitors. The first descriptions considered the morphological troubles related to fat distribution and drugs, but then metabolic association with atherogenic lipid abnormalities, low HDL cholesterol, insulin resistance and hyperglycaemia was rapidly shown. Now, we face the concept of a multivisceral inflammatory secondary chronic disease with cardio vascular events, bone, liver and kidney intrinsic anomalies – all in all showing an accelerated aging process influenced by chronic viral infection.
The management of the lipodystrophy syndrome is primarily based on antiretroviral best choice. Despite optimized treatment, we still encounter patients suffering from lipodystrophy in the present day. This can present as either old infected patients with remaining body shape change, or metabolic disorders in newly treated patients or a self body image modified by the chronic disease. A significant decrease in quality of life and psycho-social impact need a multidisciplinary approach (http://lipodystrophie.hug-ge.ch).
HIV-associated facial lipoatrophy is a true topic for dermatologists. Fillers (poly-L-lactic acid, hydroxyapatite and hyaluronic acid) and autologous fat are currently used worldwide in this indication. In Switzerland they are reimbursed but as they are classified in devices, we lack of serious evaluations used for therapeutic drugs. Tolerance and satisfaction are acceptable, but numerous studies led by sponsors should give a more objective idea on their reliability.
Fat accumulation on the neck, abdomen and arms is the most disturbing for patients. Subcutaneous fat can easily be removed by surgical liposuction and excision. However, deep intra-abdominal fat, which often induces abdominal discomfort and pain, remains inoperable. Recurrences after fat removal have been observed but do seem not to occur as frequently with the latest antiretroviral released on the market.
- Diagnose and manage the immune restoration syndrome (IRS).
Under ART, the immune reconstitution may be excessive and unbalanced, producing pathologies with «over»-inflammation. The clinical definition concerns the occurrence of new diseases and/or worsening of previous diseases within three to six months after starting antiretroviral therapy. The biological profile shows that patients experience a rapid and high improvement in CD4 count, with decreasing HIV RNA viral load. No clear risk factor has been identified to date. Several diseases involving the skin are well identified in IRS, such as shingles, eosinophilic folliculitis, kaposi sarcoma, HPV warts and condylomata, molluscum contagiosum, but also some auto-immune diseases as lupus, vitiligo.
- Diagnose and treat malignant skin tumors.
Non melanoma skin tumors: An increased risk of developing several types of skin cancer has been comparatively shown in HIV and solid-organ transplant recipients. The role of immunosuppression could be strongly suggested. ART does not influence this increased incidence of non melanoma skin tumor, and this has also been shown for cancers of the cervix, liver, lip, mouth, pharynx, lung and bronchus in recent studies [11,12].
Melanoma and HIV: The risk of melanoma is higher in this population (HIV and solid-organ transplant recipients) too, and the risk remains under ART [13]. Sudden onset of atypical nevi has been reported in old, small case series. A more aggressive tumor behavior is reported.
Continuous and systematic dermatological follow-up is required to detect early lesions. Physicians following HIV patients should encourage prevention and specialized dermatological control.
- Prevent and treat other sexually transmittel infections.
Conclusion: prevention and treatment
Skin disorders in HIV infection need to be treated by specialized physicians who know the different development stages of this infection. The pattern of the opportunistic infections associated to lymphocytes CD4 level is particularly of interest for diagnosis and prognosis during treatment. For the dermatologist, the modern approach is to think and test for HIV in any individual presenting with a risk of viral acquisition or with any dermatosis, to prevent and treat skin cancers in HIV+ persons, and to rehabilitate a body image that might be modified by the disease: esthetic medicine tools are becoming crucial in the long term psychological and social follow-up of those patients. New therapies offer the opportunity getting old with HIV.
Bibliography:
- Wiwanitkit V: Prevalence of dermatological disorders in Thai HIV-infected patients correlated with different CD4 lymphocyte count statuses: a note on 120 cases. Int J Dermatol 2004; 43 (4): 265–268.
- Cedeno-Laurent F, Gomez-Flores M, et al. : New insights into HIV-1-primary skin disorders. J Int AIDS Soc 2011; 14: 5.
- Uthayakumar S, Nandwani R, et al.: The prevalence of skin disease in HIV infection and its relationship to the degree of immunosuppression. Br J Dermatol 1997; 137 (4): 595–598.
- Lacour JP, Saiag P, et al.: HIV infection. Cutaneous-mucous manifestations of HIV primoinfection. Ann Dermatol Venereol 2002; 129 (10): 44–46.
- Toutous-Trellu L, Abraham S, et al.: Topical tacrolimus for effective treatment of eosinophilic folliculitis associated with human immunodeficiency virus infection. Arch Dermatol 2005; 141 (10): 1203–1208.
- Pechere M, Krischer J, Trellu L, et al.: Persistent periungual erythema with telangiectasia: red fingers syndrome. Arch Dermatol 1999; 135 (6): 715–716.
- Barde C, Piguet V, et al.: Management of resistant mucocutaneous herpes simplex infections in AIDS patients: a clinical and virological challenge. HIV Med 2011; 12 (6): 367–373.
- Faust H, Toft L, Sehr P, et al.: Human Papillomavirus neutralizing and cross-reactive antibodies induced in HIV-positive subjects after vaccination with quadrivalent and bivalent HPV vaccines. Vaccine 2016; 34 (13): 1559-1565.
- Chang Y, Cesarman E, et al.: Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science. 1994; 266 (5192): 1865–1869.
- Mallal S, Phillips E, et al.: HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med 2008; 358 (6): 568–579.
- Clifford GM, Polesel J, et al.: Cancer risk in the Swiss HIV Cohort Study: associations with immunodeficiency, smoking, and highly active antiretroviral therapy. J Natl Cancer Inst 2005; 97 (6): 425–432.
- Silverberg MJ, Leyden W, et al.: HIV infection status, immunodeficiency and the risk of non-melanoma skin cancer. J Natl Cancer Instit 2013 ;105: 350–360.
- Olsen CM, Knight LL, Green AC: Risk of melanoma in people with HIV/AIDS in the pre and post-HAART era: a systematic review and metaanalysis of cohort studies. Plos one 2015; 9: e95096.
- Damjan S, Toutous-Trellu, L et al.: Alopecia Universalis Associated with Vitiligo in an 18-year-old HIV-positive Patient: Highly Active Anti-retroviral Therapy as First Choice Therapy? Acta Derm Venereol 2014; 94: 116–117.
DERMATOLOGIE PRAXIS 2017; 27(6): 9–14