Andreas Studer, MD, from the University Center for Geriatric Medicine at the Felix Platter Hospital in Basel, spoke at the Update Refresher in Zurich on the two topics of dementia and depression. What does current dementia drug therapy offer? How often are older people depressed and what are the symptoms to look out for?
The first topic was the drug therapy of dementia (Fig. 1), which according to Dr. med. Andreas Studer from the University Center for Geriatric Medicine at the Felix Platter Hospital Basel is still purely symptomatic. The deterioration of the condition can be delayed, but a modification, a stop or even a cure are currently not in sight. “Moreover, it turns out that the patient with dementia pays back later that which he gains from the medication. That is to say: Towards the end, the condition then suddenly deteriorates very rapidly and he lives about the same length of time as the untreated patient. The only thing we can expect at all from the current therapy is, in the best case, a temporary improvement,” the speaker continued.
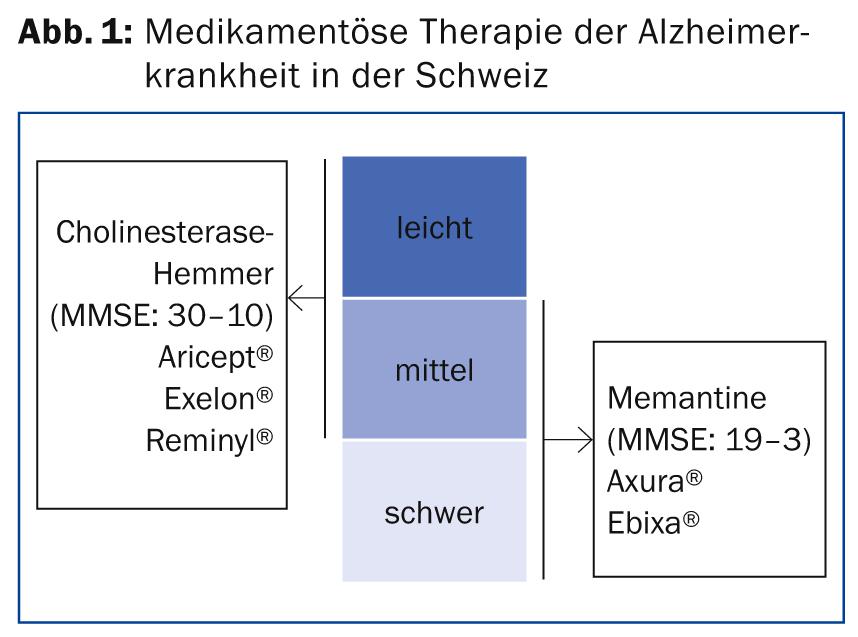
One drug approach to Alzheimer’s dementia is to increase the availability of acetylcholine in the synapses. The cholinesterase (ChE) inhibitors available in Switzerland are donepezil (Aricept®), rivastigmine (Exelon®) and galantamine (Reminyl®). Rivastigmine has a short half-life, but the effect is much longer than the half-life would suggest. The new transdermal application by patch is particularly useful. According to Dr. Studer, this is easy to use and much better tolerated than the other dosage forms (capsule, solution). Galantamine is now only available in the so-called “prolonged release” form. The titration is not quite simple, but not too complicated either. In principle, all three are roughly equivalent in terms of efficacy, so the decision is usually made on the basis of galenics.
Effect of ChE inhibitors and memantine.
ChE inhibitors may, over a period of time, delay dysfunction of cognition, Activities of Daily Living (ADL) (instrumental), clinical global impression, and, to some extent, neuropsychiatric symptoms. They are indicated for mild to moderate dementia of the Alzheimer’s type (“Mini Mental State Examination” MMSE: 30-10). In addition to Alzheimer’s disease, the indication for rivastigmine (Exelon®) also includes Parkinson’s disease and Lewy body dementia (S3 guideline). According to the same guideline, ChE inhibitors are likely to work in mixed dementias (the most common form of dementia in people >80 years). These include, for example, mixed forms of Alzheimer’s and vascular dementia. They are probably also effective in pure vascular dementia, but less so than in Alzheimer’s type. However, they show no effect against frontotemporal or alcohol dementias or against Korsakow’s syndrome.
“According to the Federal Social Insurance Office (BSV), an MMSE is indicated at the beginning of therapy and again after three months in the course of an interim evaluation. Thereafter, such a cognitive inventory must be performed every six months. If the MMSE value falls below ten, the costs for ChE inhibitors are no longer covered by health insurance,” Dr. Studer explained. There is also evidence that donezepil is effective in Alzheimer’s dementia even in the severe stage of the disease, and continuation or new treatment at this time can be recommended according to the S3 guideline. However, health insurance does not cover such therapy, which leads to a preference in Switzerland for an overlapping switch to memantine for severe dementia. “In my opinion, the decisive factor is whether a ChE inhibitor can improve hard facts such as walking, eating, speaking, assisting with care and urine control. In this case, continued non-pay therapy is often justified,” the expert said.
The mechanism of action of memantine differs from that of ChE inhibitors. This is a selective antagonist of the NMDA-type L-glutamate receptor with a long half-life, available in Switzerland as Axura® and Ebixa®. It is indicated in moderate to severe AD (MMSE: 19-3) and also delays dysfunction of cognition, ADL, clinical general impression, and partial neuropsychiatric symptoms. It is also likely to be effective in mixed forms of dementia as well as in pure vascular dementia (S3). Like the ChE inhibitors, it shows no effect in frontotemporal and alcohol dementias and in Korsakow syndrome. In principle, memantine is well tolerated and has few side effects, according to Dr. Studer. Costs are no longer covered below an MMSE score of three. In principle, the active ingredient is not cheap, but the price must be set against the high costs incurred by severely demented patients in nursing homes. So delaying full care for a year may very well make sense and be cost-effective.
Also discussed was the efficacy of ginkgo biloba preparations. According to the S3 guidelines, they are currently not recommended for dementia due to insufficient evidence of their efficacy; however, they are recommended for mild cognitive impairment (MCI). According to Dr. Studer, they can certainly be used here, especially since there are no alternatives up to this point.
Depression in old age
According to Dr. Studer, there are studies that report the prevalence of depression in old age to be 14.1 in women and 8.6% in men. In nursing homes, the incidence of especially dysphoric minor depression is significantly higher at 30-45%. “Not to be forgotten are the depressions associated with chronic physical illnesses, which add up in old age. Depression can clearly worsen the outcome of diabetes mellitus,” the expert said. Some important symptoms of depression in the elderly that should also receive attention in family practice are listed in Table 1 .
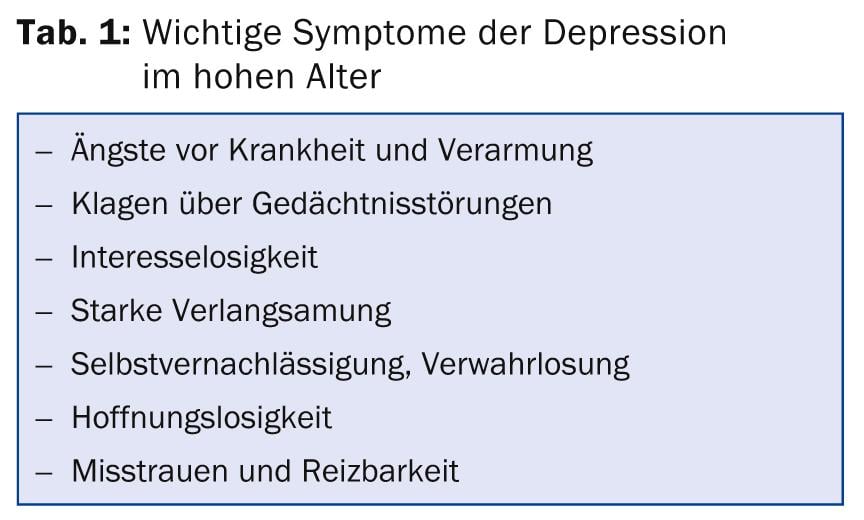
Typical somatic signs are found in sleep disturbances, hypochondriacal fears, concentration disorders, psychomotor slowdown, fatigue, loss of energy and, last but not least, pain that cannot be explained organically or not adequately.
“A frequent trigger and risk factor for depression in old age is, among other things, the loss of independence as a result of physical illness, i.e. the anxious question: How long will I manage to look after myself alone? In addition, old age is often accompanied by a certain loneliness and a lack of social support. This can also have to do with a change of location, e.g. a move to Ticino. Here, there is a threat of being uprooted. In addition, financial worries, conflicts with relatives, a negative life balance and a depressive personality structure are risk factors for depression in old age,” Dr. Studer explained. As a result, men often turn to alcohol, while women are more likely to abuse medications. Vulnerability to somatic illness increases with depression, as does hospitalization duration and financial burden. Mortality is also on the rise. Again and again, Dr. Studer encounters so-called “passive” suicides: Elderly patients with chronic conditions who require regular medication deliberately do not take it and die.
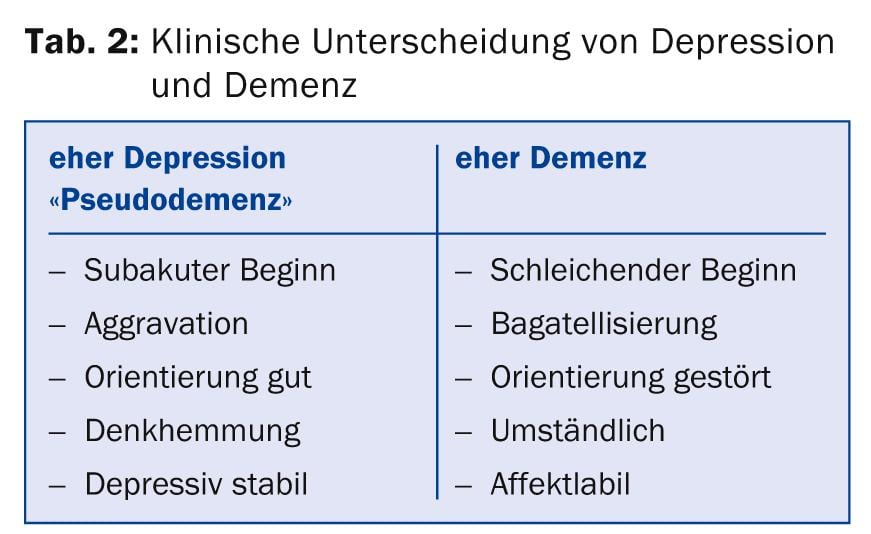
Moreover, the symptoms of depression in old age and dementia overlap strongly (Fig. 2).
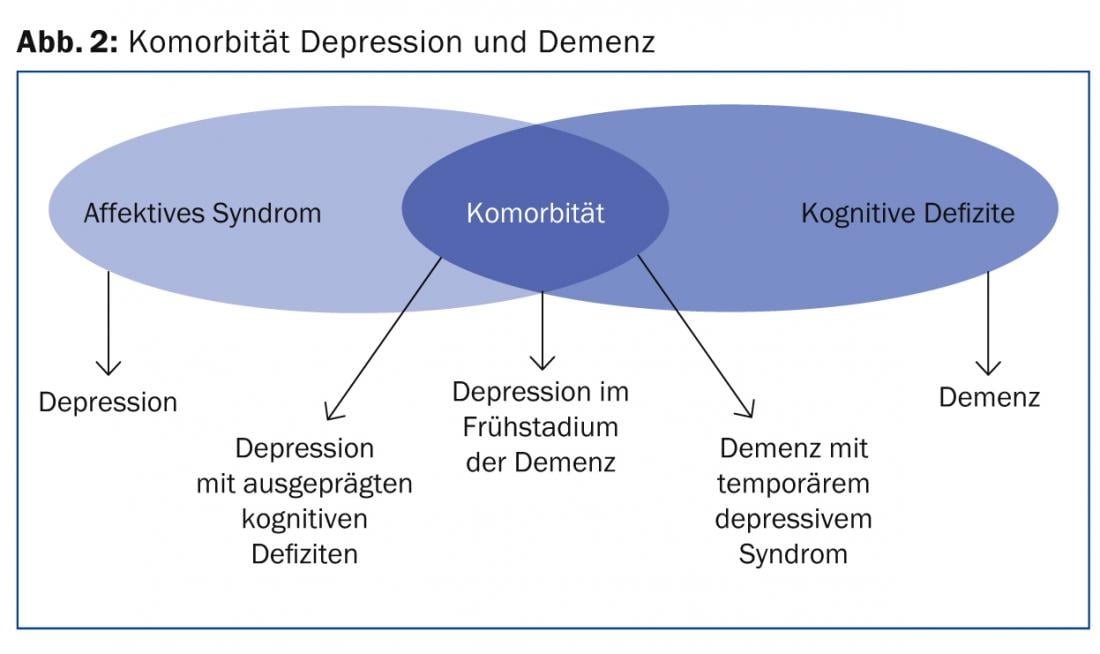
These two disorders are the most common psychiatric disorders in the elderly, and statistically they often occur together, especially in individuals >80 years of age. Thus, an accurate diagnosis is important because prognosis, treatment, and care vary. Clinically, the two clinical pictures can certainly be differentiated, which is shown in simplified form in table 2.
Suicides in old age
According to Dr. Studer, 80% of elderly people who commit suicide suffer from depression. Suicidal thoughts are more life-threatening in older people (related to this the mnemonic: “Young women attempt suicide, old men kill themselves”). There is a high risk of recurrence even if the suicide fails.
Crucially, however, the chances of cure and improvement with therapy are the same as for boys. A combination of medication, psychotherapy and sociotherapy is useful. The various antidepressants are summarized in Table 3.
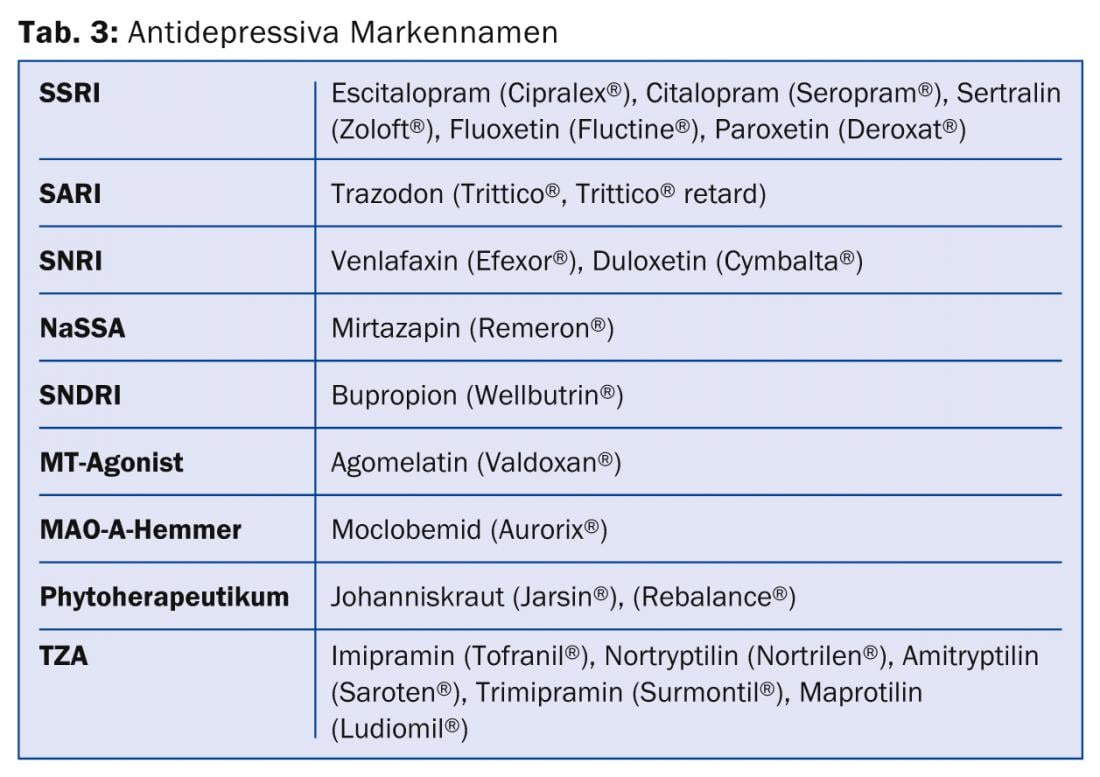
Basically, according to Dr. Studer, pharmacotherapy for depression in the elderly:
- The best antidepressants are those with the fewest side effects.
- Gradual dosing
- I.d.R. lower target dose (>80-year-olds one-third to one-half), but if necessary increase to maximum recommended dose
- No abrupt dose changes, taper off (SSRI!).
- No tricyclic antidepressants (TCAs, first-generation AD) in multimorbid and demented patients.
- No psychotropic combination drugs (e.g., Deanxit).
- No St. John’s wort if polymedicated (has an impact on anticoagulation, which can cause problems if polymedicated)
- Choose a sedative-anxiolytic antidepressant for sleep disturbances and anxiety
- If there is no or insufficient response within six to eight weeks, referral to geriatric psychiatrist.
Source: FOMF General Internal Medicine Update Refresher, May 7, 2014, Zurich.
HAUSARZT PRAXIS 2014; 9(7): 50-52