Poorly controlled diabetes is a risk factor for severe COVID-19 progression. Therefore, especially during the corona pandemic, the best possible blood glucose control is crucial. However, it has been shown that many patients avoid visits to the practice and clinic for fear of infection – this should change. There is an interesting study finding on DPP-4 inhibitors: in hospitalized COVID-19 patients, sitagliptin as an additive treatment was associated with milder courses.
Good glycemic control of diabetics is very important, especially in the pandemic, emphasized Prof. Dr.med. Matthias Laudes, Head of Endocrinology, Diabetology and Clinical Nutrition Medicine at the University Hospital Schleswig-Holstein, Kiel (D), in the context of the congress Diabetologie grenzenlos [1]. Poorly controlled diabetes increases the risk for severe COVID-19 progression. Obesity is also a risk factor. The younger COVID patients in the intensive care unit at Kiel University Hospital are mostly overweight people, the speaker reported. The fact that obesity is associated with more severe COVID courses can be explained by an increased tendency to thrombosis due to the metabolic inflammatory state, Prof. Laudes said. Thrombotic clots in the smallest blood vessels can lead to organ failure in COVID-19 disease.
Optimal glucose control during corona pandemic particularly important
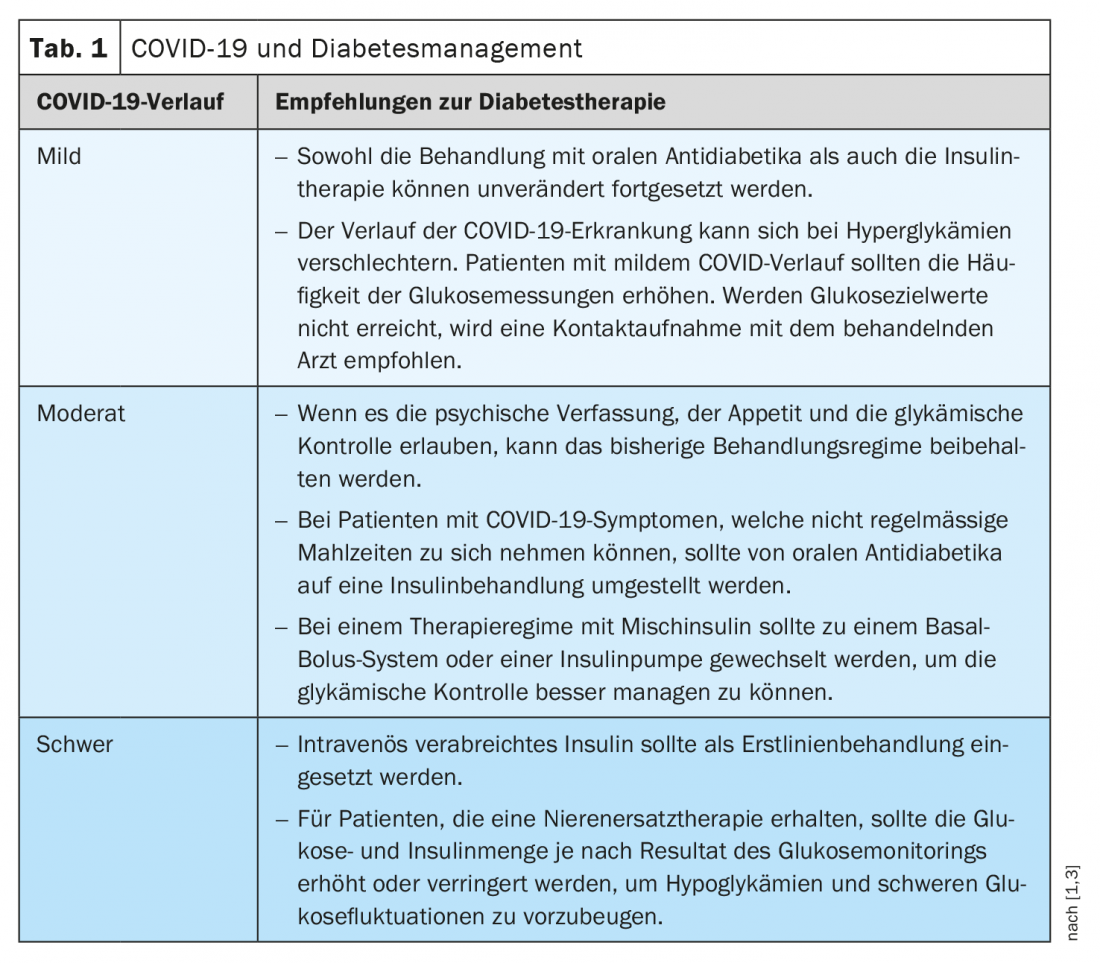
The immune system appears to rely on good insulin sensitivity, and elevated insulin levels increase the risk for prothrombotic events during infection. But there is also another reason. In diabetics, angiotensin converting enzyme 2 (ACE-2) activity is increased. It is known that SARS-CoV-2 uses the membrane-bound enzyme ACE-2 to enter somatic cells [2]. The amount of this enzyme on the cell surface correlates with blood glucose levels. If the glucose level is too high, there is more ACE-2 on the cell surface, making it easier for the virus to enter the body’s cells. “Therefore, the most important thing for us at this time is to control diabetes well so that the amount of this protein, which serves as a portal of entry, is as low as possible,” summarizes Prof. Laudes. “The better the diabetes is controlled, the less ACE is on the body’s cells and the lower the incidence of infection of individual cells,” the speaker added. Thus, optimal diabetes management is essential, especially during the corona pandemic (Table 1) [1,3]. However, many patients avoid clinic visits for fear of infection and this can have negative consequences. “We have to take away the fear of patients to go to the surgeries and clinics, all hygiene standards are maintained there,” Prof. Laudes elaborates. “Patients need to be aware that they should come to the doctor’s office especially frequently during this time in order to have perfect blood glucose control.”
What is the role of DPP-4?
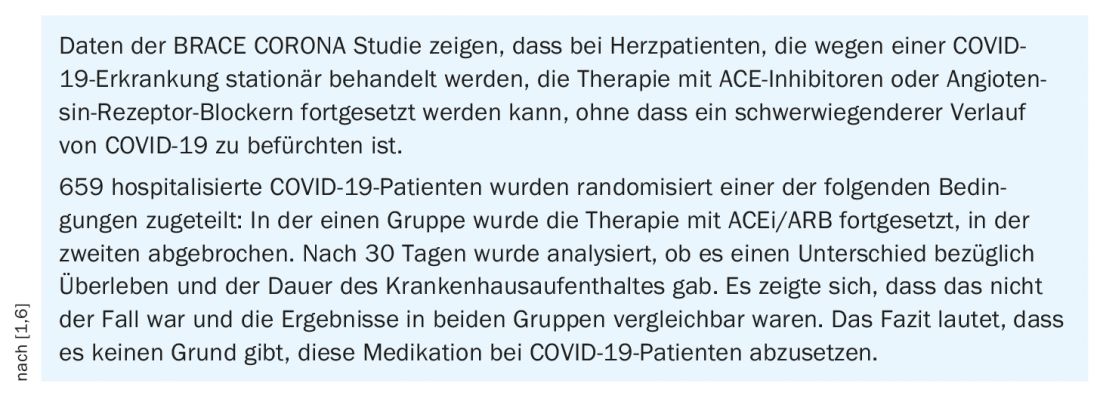
That ACE inhibitors have no adverse effect on the course of COVID disease, is known from studies (Box). Regarding DPP-4 inhibitors, which are known to be widely used in diabetics, there are also interesting findings and studies are underway to determine whether DPP-4 inhibitors can be used in the future as additive agents to improve COVID courses. It has been discussed for some time whether the SARS-CoV-2 virus binds not only to ACE-2 but also to DPP-4. So far, it has not been possible to clarify this question conclusively. An interesting observation, however, is that DPP-4 not only occurs on the cell surface, but also circulates in the bloodstream, which is known as ‘soluble DPP-4’. During an infection, the virus cannot distinguish whether the protein for docking is only on the cell surface or whether it is also floating around in the blood, the speaker said. “If less of the soluble protein is present, stronger binding takes place to the membrane-bound proteins, and thus stronger infection of cells. Conversely, if more of the soluble protein is present, viruses are scavenged and thus cell infection is less,” says Prof. Laudes, summarizing the hypothesis of how soluble enzymes influence the infectivity of the virus. A study published in December 2020 demonstrated that diabetes patients hospitalized for COVID-19 disease who received the DPP-4 inhibitor sitagliptin in addition to insulin (n=169) had a better outcome than those treated with insulin alone (n=169) [4]. For example, in the sitagliptin group, mortality was significantly lower and time to hospital discharge was shorter. The explanation: Patients who are in the ICU with a severe course of COVID have less of the soluble DPP-4. When you give DPP-4 inhibitors, the body makes more of the soluble DPP-4 in response, which allows more virus to be intercepted, Prof. Laudes explains. There are further studies on this, which also examine how the effects of DPP-4 inhibitors in non-diabetics affect the course of COVID-19 disease. So far, no conclusive results are available.
Type 1 diabetes: delayed diagnosis during lockdown
Diabetic ketoacidosis is a life-threatening emergency in the manifestation of type 1 diabetes mellitus in children and adolescents, often associated with delayed diagnosis or previous misdiagnosis. An analysis of data from 532 patients from 216 diabetes centers in Germany showed that significantly more cases of diabetic ketoacidosis occurred in the setting of type 1 diabetes mellitus in children and adolescents during the period of COVID-19 lockdown [5]. The main risk factors included age <6 years, migrant background, and delayed presentation to the clinic or practice. One explanation is that people visit the emergency room late for fear of infection, by which time ketoacidoses have already developed.
Source: Diabetology without borders 2021
Literature:
- Laudes M: SARS-CoV-2, COVID-19, obesity and diabetes. Prof. Dr.med. Matthias Laudes, Diabetology without borders, press conference, Feb. 26, 2021.
- Hoffmann M, et al: SARS-CoV-2 Cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020; 181: 271-280.
- International Diabetes Federation 2020, https://idf.org (last accessed Mar. 04, 2021).
- Solerte SB, et al. Sitagliptin Treatment at the Time of Hospitalization Was Associated With Reduced Mortality in Patients With Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study. Diabetes Care 2020 Sep; dc201521. https://doi.org/10.2337/dc20-1521
- Mönkemöller K, et al: Can ketoacidosis be avoided in pediatric patients with manifestation of type 1 diabetes mellitus? Lessons from the COVID-19 pandemic. Monatsschr Kinderheilkd 2021, https://doi.org/10.1007/s00112-020-01108-2
- Lopes RD, et al. Continuing versus suspending angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: Impact on adverse outcomes in hospitalized patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-The BRACE CORONA Trial. Am Heart J 2020; 226: 49-59.
HAUSARZT PRAXIS 2021; 16(3): 4-5 (published 10.3.21, ahead of print).