Anxiety disorders are among the most common psychiatric disorders. The reaction to danger, which is actually essential for survival, becomes clinically relevant at the moment when the fear experience is groundless, exaggerated or unrealistic. The frequency of this clinical picture has increased significantly in recent years. With proper diagnosis, effective treatment is possible.
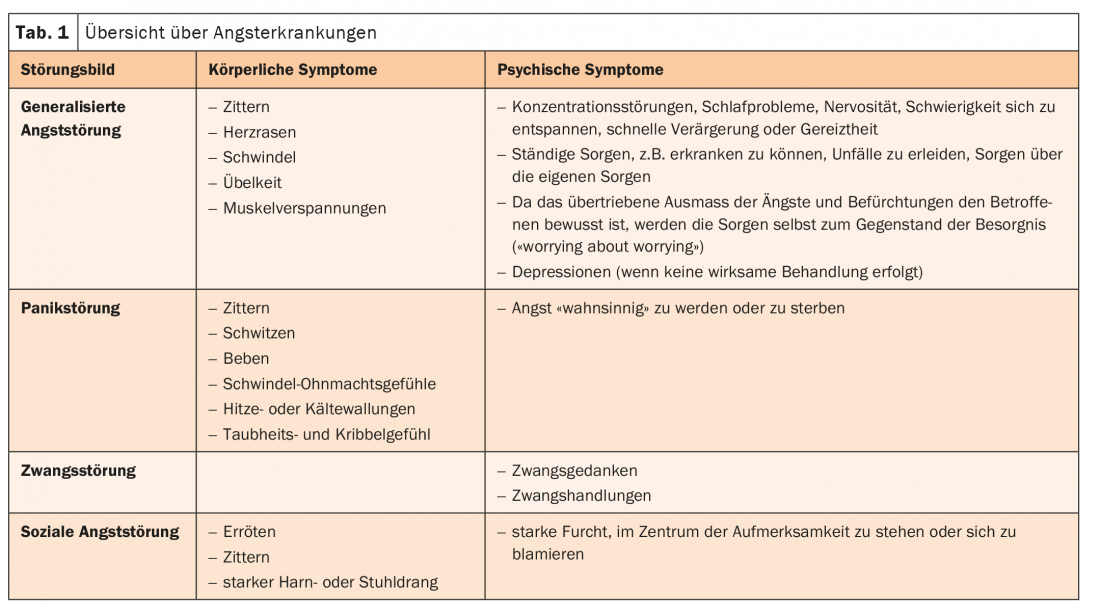
Every person knows fears, insecurities, doubts. These are usually temporary and linked to a specific situation. However, approximately 20% of the population suffers from very severe and/or persistent anxiety [1]. Anxiety can therefore occur as part of a normal stress reaction, as an accompanying symptom of another mental disorder, as an expression or consequence of a physical illness, or be caused by medication or addictive substances. Anxiety can occur as a leading symptom of various disorders. These include generalized anxiety disorder, panic disorder, obsessive-compulsive disorder, and social anxiety disorder (Table 1) [2].
Common disease, often overlooked
Anxiety disorders often go unrecognized because patients complain of pain, sleep disturbances, or other somatic complaints rather than anxiety. The diagnosis is based on the differentiation between symptom, syndrome and diagnosis level. At the symptom level, the focus is primarily on physical complaints. In addition, avoidance behavior and worry or social behavior strategies are recorded. At the syndrome level, the severity is assessed. Self-assessment and third-party assessment scales are used for this purpose. Initial indications of the diagnosis are usually already apparent in spontaneous descriptions of the complaints in the free clinical interview. However, since this is often not reliable enough, standardized interviews should be used in the further course. In addition, the possibility of comorbid conditions such as depression, psychotropic substance disorders, somatoform disorders, or additional anxiety disorders to be closely examined.
In the anamnesis, in addition to a self-history, family history and external anamnesis, a differentiation of anxiety should also be made. Is the fear situation or object related? What triggers it. What is the course of the disease and what is the degree of impairment? The somatic diagnosis clarifies whether it may be a secondary anxiety symptom. If anxiety symptoms occur after the age of 45, a somatic cause is more likely [2]. However, repeated somatic workup should be avoided because of the risk of iatrogenic fixation and chronicity.
Multimodal treatment management
An effective way to counter stressful situations can be the use of phytopharmaceuticals. Products based on valerian can bring calm back into life in case of stress and nervousness.
An indication for therapy of anxiety disorders exists when patients have moderate to severe distress with impairments in the social and/or occupational domains, psychosocial limitations, and comorbid conditions such as addiction. The goal is to reduce anxiety symptoms and avoidance behaviors, improve quality of life, and reduce the likelihood of relapse. Included are improvements in limited mobility, social integration and occupational performance.
The gold standard for the treatment of anxiety disorders is a combination of cognitive behavioral therapy (CBT) and pharmacologic interventions. However, psychotherapy is often not available in a timely manner. Suggestions for self-help should be given here to bridge the waiting time. Pharmacological therapy is divided into three phases: acute therapy, maintenance therapy and prophylactic therapy. A number of substances from different substance classes are available for drug treatment. These include SSRIs and SSNRIs as the drugs of choice, then tricyclics, benzodiazepines, and other preparations such as anticonvulsants.
Literature:
- www.sgad.ch/de/hilfe/angststoerung (last accessed 10.08.2021)
- www.medix.ch/wissen/guidelines/psychische-krankheiten/angststoerungen (last accessed 10.08.2021)
- https://zellerag.ch/de/gesundheit-wissen/pruefungsangst (last accessed on 10.08.2021)
InFo NEUROLOGY & PSYCHIATRY 2021; 19(4): 24-25.











