The basis of diagnosis in urothelial carcinoma is urethrocystoscopy, bladder irrigation cytology, and computed tomography with excretion phase. Image-enhancing techniques increase the diagnostic accuracy of urethrocystoscopy and thus may improve recurrence-free survival in superficial urothelial carcinoma of the urinary bladder and upper urinary tract. FDG-PET/CT offers no relevant advantage in the primary diagnosis of lymph node metastases in invasive urothelial carcinoma. Despite state-of-the-art imaging, lymph node metastases (pN+) are found in 25% of patients undergoing cystectomy for invasive urothelial carcinoma who were preoperatively classified as lymph node negative (cN0). Extensive pelvic lymphadenectomy is therefore mandatory as part of cystectomy, even in the cN0 stage.
Urothelial carcinoma is the sixth most common cancer in the Western world [1] and one of the most costly from an economic point of view [2]. In addition to the costs of surgical interventions, which are not insignificant especially due to the high recurrence rate of bladder cancer, diagnostic investigations are also a major cause of the high costs. In light of this, it is important to view the ever-evolving diagnostics with a critical eye. The various diagnostic options in urothelial carcinoma are discussed below.
Urinalysis
Apart from anamnesis (macrohematuria?), the first step in diagnosis is urine examination. The strip test has a very high sensitivity for microhematuria (up to 97%), but may be falsely positive in alkaline urine, hemolysis, myoglobinuria, after ejaculation, or due to oxidants (including bethadine). Therefore, in case of a positive strip test, the finding should always be confirmed by microscopic urine examination. It is also important to minimize false positive urine tests by proper urine collection (midstream urine, single catheter urine in women if necessary).
Urine cytology should be obtained if a bladder tumor is suspected. Urine cytology is most sensitive by obtaining a so-called bladder lavage cytology, in which cells of the bladder wall are exfoliated by means of a disposable catheter and subsequent lavage of the urinary bladder with physiological solution. Urine cytology shows high sensitivity especially in the diagnosis of bladder tumors with poor differentiation (high grade: G3/4). In carcinoma in situ (CIS), the sensitivity of bladder lavage cytology is as high as 97% and is considered sufficient to initiate immunotherapy with intravesical BCG in the absence of solid tumor. However, urine cytology cannot be used to determine the origin of the tumor cells (bladder or upper urinary tract).
Although a variety of bladder tumor marker systems are on the market (including UroVysion FISH, Immunocyt/uCyt +, Bladder Tumor Antigen, Nuclear Matrix Protein 22), none has yet become established in clinical practice, either for primary diagnosis or as a marker in follow-up [3]. For well-differentiated tumors (low grade: G1/2), there is a higher sensitivity (50-80%) than cytology, but also a much lower specificity. In particular, benign changes in the bladder mucosa can result in false positive findings.
Blood tests
Although bleeding anemia is a common finding in patients with invasive urothelial carcinoma, blood testing cannot diagnose urothelial carcinoma because specific tumor markers for urothelial carcinoma are lacking.
Urinary bladder endoscopy (urethrocystoscopy)
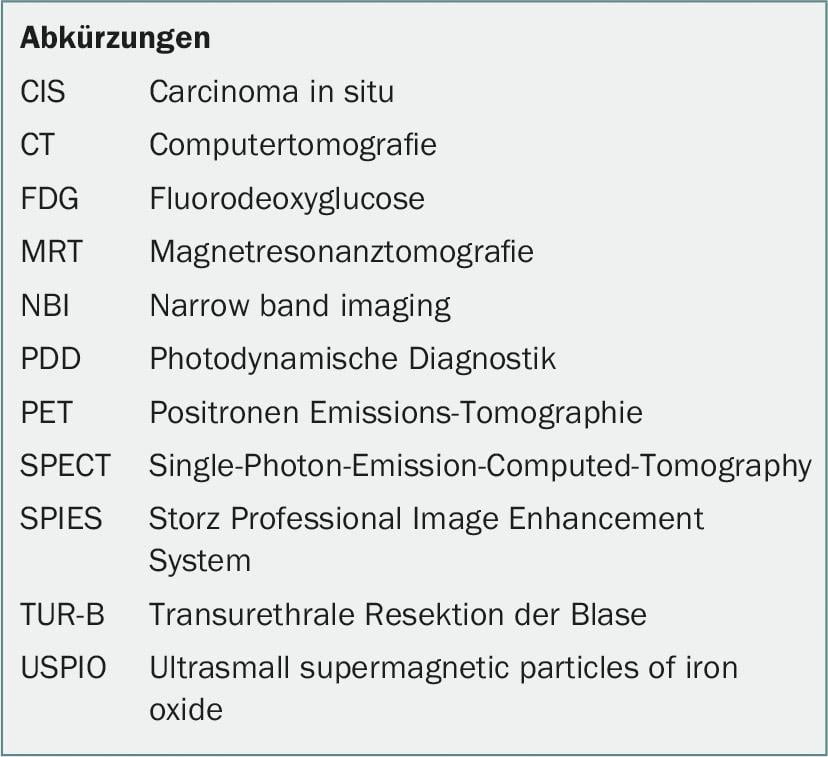
The cornerstone of any urothelial carcinoma diagnosis is urethrocystoscopy (Fig.1). In case of positive findings, histological confirmation is performed by transurethral resection (TUR-B) under spinal or intubation anesthesia (Fig. 1b). In this procedure, the exophytic portions and the base of the tumor, which should necessarily contain muscle of the bladder wall, are removed and usually sent separately for histologic evaluation. During TUR-B, a bimanual examination is also performed to assess for the presence of organ-spanning tumor growth (≥cT3). Fixation of the bladder to adjacent structures or the pelvic wall suggests trans-organ growth. It has been shown that bimanual palpation provides an additional improvement for the detection of organ overgrowth despite massively evolving radiologic diagnostics [4].
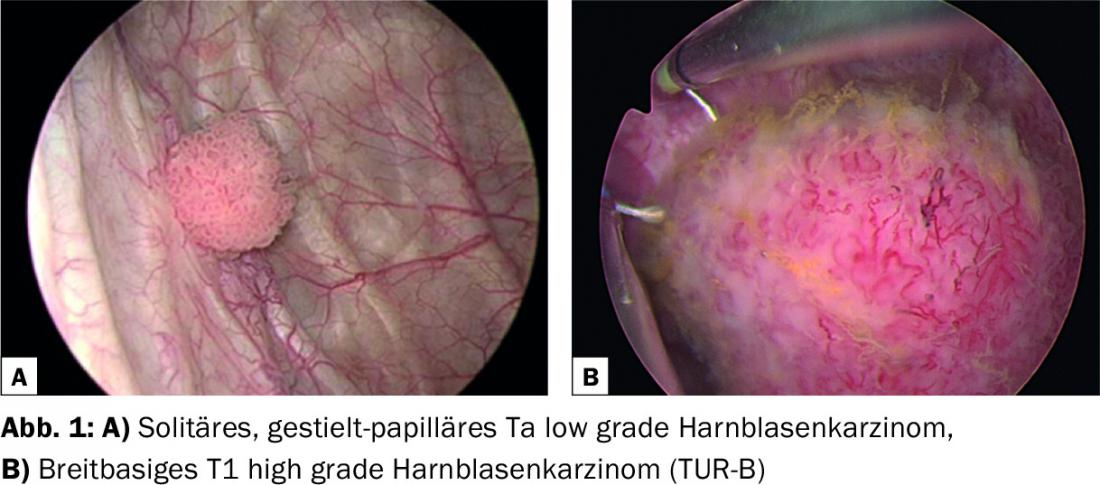
Image enhancing cystoscopic procedures
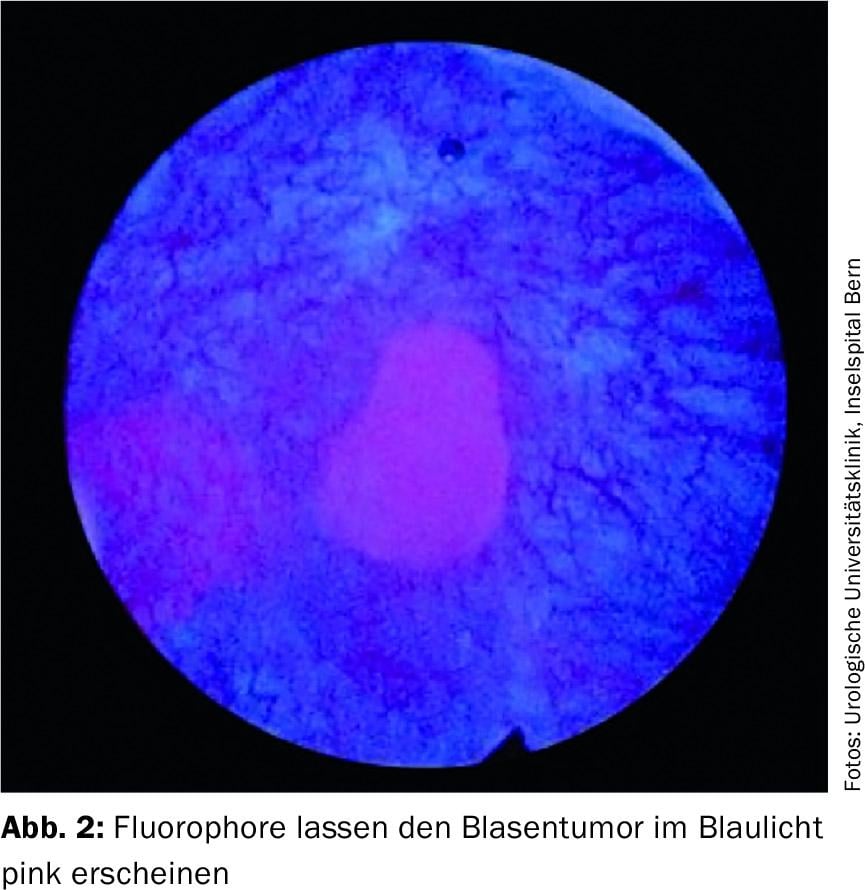
Photodynamic diagnosis (PDD) is used to improve the detection of urothelial carcinoma during urethrocystoscopy. In this procedure, a fluorescent dye is instilled into the bladder via a bladder catheter 1-2 hours before the scheduled procedure. The accumulation of fluorophores in the malignant cells causes them to glow pink under blue light (Fig. 2) . PDD shows an improved detection rate especially in the presence of CIS. Thus, a reduced recurrence rate at 12 months was demonstrated using PDD [5]. However, long-term results regarding survival and progression rates are lacking. In addition, a possible disadvantage of PDD is the high rate of so-called false positive findings.
Other methods to improve endoscopic diagnosis include narrow band imaging (NBI) and the Storz Professional Image Enhancement System (SPIES), both of which use filters (blue/green) and optical enhancement to achieve better contrast between hyperperfused tumor area and normal bladder mucosa during urethrocystoscopy ( Fig. 3) [6]. Thereby, there seems to be a possible advantage in terms of recurrence-free survival in non-invasive urothelial carcinoma of the urinary bladder compared to standard white light cystoscopy, but not in terms of progression-free survival [7]. NBI and SPIES show similar results [8]. Since these are purely imaging-based procedures, the additional costs are very moderate, which is why this diagnostic method is likely to become established in the future.

A new approach exists by combining tumor-specific antibodies (including CD47) with fluorophores. These conjugated antibodies are instilled into the bladder and then washed out. Subsequently, blue light urethrocystoscopy can be used to detect the tumor areas. Initial results show very high sensitivity (83%) and specificity (>90%) [9].
General imaging
Ultrasound examination may provide initial evidence of a bladder tumor. However, since both the specificity and, above all, the sensitivity are low, sonography, in contrast to computed tomography (CT; including the excretory phase) or magnetic resonance imaging (MRI), is not part of standard diagnostics in urothelial carcinoma. CT examination is usually preferred to MRI, because the upper urinary tract (extravesical second urothelial carcinoma?) can be better clarified in the excretory phase on CT.
Imaging of the primary tumor
For assessing whether it is superficial or invasive urothelial carcinoma, diagnostic TUR-B is superior to any previously available noninvasive imaging. However, TUR-B and bimanual palpation alone underestimates extravesical extension (≥T3) in approximately 40% [1]. With regard to the assessment of extravesical extension, dynamic contrast-enhanced MRI appears to offer a diagnostic advantage of 10-33% over CT examination [10], with an accuracy of 40-67% in the assessment of depth of invasion by MRI [10,11]. Multiparametric MR imaging did not significantly improve accuracy in tumor staging (52-85%) [11]. The best prediction for definitive histologic tumor stage can be achieved by combining imaging and bimanual palpation (sensitivity, 66%; specificity, 89%) [4].
Lymph node imaging
25% of patients who are classified as lymph node negative (cN0) preoperatively by CT or MRI turn out to be lymph node positive (pN+) histologically after extended pelvic lymphadenectomy. Considering that molecular examinations of the lymph nodes additionally show tumor cells in the lymph nodes in up to 30% of pN0 patients, it must be assumed that with CT examination alone approximately 30-40% of lymph node metastases are missed [12]. Especially small metastases (<6 mm) often remain undetected, whereas reactively enlarged lymph nodes are often misinterpreted as positive. Thus, it is obvious that new imaging techniques are needed.
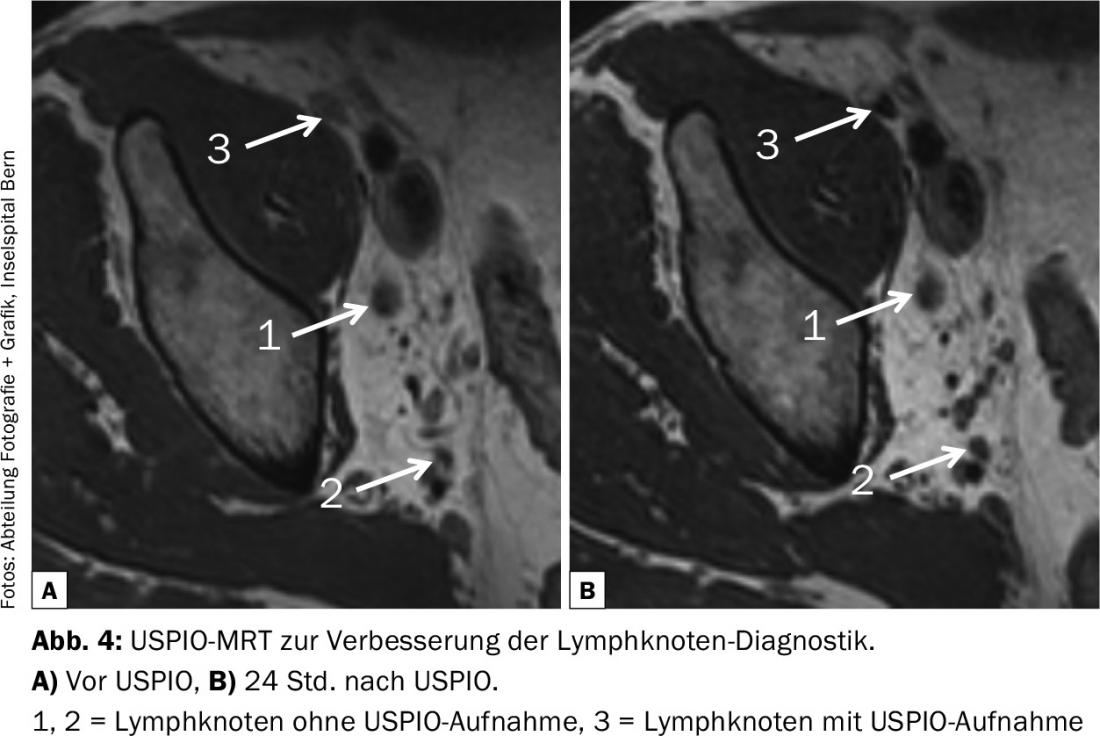
Improvement can be achieved using diffusion-weighted MRI (sensitivity: 64-79%, specificity 79-85%), especially when combined with ultrasmall supermagnetic particles of iron oxide (USPIO) MRI, using these “supermagnetic” iron particles as contrast agents (Fig. 4) [13]. This elaborate examination may improve the detection rate of metastases in non-enlarged lymph nodes, but still 25-35% of positive lymph nodes remain undetected preoperatively. Therefore, accurate extensive pelvic lymphadenectomy must always be performed as part of the cystectomy despite negative imaging. Even more so because lymphatic drainage in urothelial carcinoma of the urinary bladder varies from patient to patient, as demonstrated by SPECT-CT studies [14]. This is one of the reasons why the sentinel lymph node concept does not work in urothelial carcinoma – together with the fact that metastatic tissue in lymph nodes or lymphatic vessels prevents the uptake of radioactive tracer and leads to secondary lymphatic bypass pathways.
PET-CT
Since in urothelial carcinoma both primary tumor and metastases show increased glucose consumption, fluorodeoxyglucose (FDG)-PET/CT seems promising for diagnosis. While the initial results in 2010 showed promising results for the diagnosis of lymph node metastases (sensitivity 46%, specificity 97%), the recently published data of Aljabery et al. sobering: FDG-PET/CT showed no advantage over ordinary CT examination in either sensitivity (41% vs. 41%) or specificity (86% vs. 89%) [15,16].
Further diagnostics
Both chest CT and skeletal scintigraphy are recommended to complete staging because the predilection sites for hematogenous metastasis in urothelial carcinoma are the lungs and bones [3].
Conclusion
Despite major technical advances, urethrocystoscopy combined with bladder lavage cytology remains the cornerstone of diagnosis in bladder cancer. The variety of tumor marker systems for urine testing cannot mask the fact that both sensitivity and specificity of these systems are too low for meaningful diagnosis. Newer imaging techniques may improve staging diagnosis but are far from predicting even extravesical spread (≥ T3) with high probability. In addition, although modern imaging techniques may slightly improve the detection of lymph node metastases, 25% of lymph node-positive patients are still misclassified as lymph node-negative preoperatively. Therefore, extended pelvic lymphadenectomy should always be performed as part of cystectomy, regardless of preoperative lymph node status.
Literature:
- Rais-Bahrami S, et al: Contemporary role of advanced imaging for bladder cancer staging. Urol Oncol 2016; 34(3): 124-33.
- Svatek RS, et al: The economics of bladder cancer: costs and considerations of caring for this disease. Eur Urol 2014; 66(2): 253-62.
- EAU Guidelines on bladder cancer, 2015.
- Rozanski AT, et al: Is examination under anesthesia still necessary for the staging of bladder cancer in the era of modern imaging? Bladder Cancer 2015; 1(1): 91-96.
- O’Brian T, et al: Prospective randomized trial of hexylaminolevulinate photodynamic-assisted transurethral resection of bladder tumor (TURBT) plus single-shot intravesical mitomycin C vs conventional white-light TURBT plus mitomycin C in newly presenting non-muscle-invasive bladder cancer. BJU Int 2013; 112(8): 1096-1104.
- Cauberg EC, et al: Narrow band imaging cystoscopy improves the detection of non-muscle-invasive bladder cancer. Urology 2010; 76(3): 658-663.
- Herr H: Randomized trial of narrow-band versus white-light cystoscopy for restaging (second-look) transurethral resection of bladder tumors. Eur Urol 2015; 67(4): 605-608.
- Lee JY, et al: A network meta-analysis of therapeutic outcomes after new image technology-assisted transurethral resection for non-muscle invasive bladder cancer: 5-aminolaevulinic acid fluorescence vs hexylaminolevulinate fluorescence vs narrow band imaging. BMC Cancer 2015; 15: 566.
- Pan Y, et al: Endoscopic molecular imaging of human bladder cancer using a CD47 antibody. Sci Transl Med 2014; 6(260): 260.
- Barentsz JO, et al: Primary staging of urinary bladder carcinoma: the role of MRI and a comparison with CT. Eur Radiol 1996; 6: 129-133.
- De Leon AD: Role of multiparametric MR imaging in malignancies of the urogenital tract. Magn Reson Imaging Clin N Am 2016; 24(1): 187-204.
- Paik ML, et al: Limitations of computerized tomography in staging invasive bladder cancer before radical cystectomy. J Urol 2000; 163: 1693-1696.
- Birkhäuser FD, et al: Combined ultrasmall superparamagnetic particles of iron oxide-enhanced and diffusion-weighted magnetic resonance imaging facilitates detection of metastases in normal-sized pelvic lymph nodes of patients with bladder and prostate cancer. Eur Urol 2013; 64(6): 953-960.
- Roth B, et al: A new multimodality technique accurately maps the primary lymphatic landing sites of the bladder. Eur Urol 2010; 57(2): 205-211.
- Swinnen G, et al: FDG-PET/CT for the preoperative lymph node staging of invasive bladder cancer. Eur Urol 2010; 57(4): 641-647.
- Aljabery F, et al: PET/CT versus conventional CT for detection of lymph node metastases in patients with locally advanced bladder cancer. BMC Urol 2015; 15: 87.
InFo ONCOLOGY & HEMATOLOGY 2016; 4(5): 14-17.