Basal cell carcinoma (BCC) is the most common cancer in the world. Various factors and tumor characteristics influence the risk of recurrence, which is why BCC is divided into high- and low-risk BCC. In treatment, the goal is complete removal of the tumor with a cosmetically satisfactory result. The therapeutic gold standard remains surgical excision. However, topical therapies (e.g., imiquimod), photodynamic therapy, and radiotherapy have also become popular for low-risk BCC. For very large, invasive and metastatic BCC, there is now also a systemic therapy with vismodegib, which has been approved in Switzerland since 2013.
In the United States, the lifetime risk of a Caucasian male developing basal cell carcinoma (BCC) is approximately 30% [1]. In Switzerland, the cantons of Neuchatel and Vaud showed an incidence of 200/100 000 inhabitants in the age group 70-79 years in 2003 [2]. In fact, the number is probably higher, because the BCC is not reportable and the coverage is therefore patchy. In addition, in practice, BCC are often removed with procedures that do not allow histologic confirmation.
Definition of basal cell carcinoma
BCC is a mostly very slow growing tumor of the skin. Growth is often three-dimensional and in almost all cases causes only local tissue destruction. Because of the extremely low metastasis rate (<0.003-0.1%), it is also referred to as a semimalignant tumor [3]. It probably originates from precursor cells from different levels of the hair follicle, the most common of which is the hair root sheath. It is thought to be monoclonal in origin, as evidenced by the fact that different types of BCC can grow despite the same localization. One almost always finds BCC in sun-exposed areas of the body. In about 80% of patients, BCC occurs between the corner of the mouth and the lower base of the ear (the so-called “mask area”), of which the nose is the most common with 30% (Figs. 1 and 2). The order of most frequent localizations is nose > trunk > lower third of face > capillitium and remaining skin.


Risk and causes
The typical patient with BCC is Caucasian, over 60 years of age, and male. Light skin types are predominantly affected (I and II according to Fitzpatrick) [4]. The incidence of BCC is increasing, faster in women than in men; lifestyle factors are thought to be the reason.
UV light, especially sun exposure over years, is considered the main cause of BCC development. For BCC, intense, short UVB exposures in the 290-320 nm range appear to have the greatest impact. Therefore, artificial sources of irradiation (solariums, phototherapy, etc.) can also be stressful. Immunosuppression is estimated to increase the risk of developing BCC by a factor of 10 [5]. Ionizing radiation, for example radiotherapy and especially frequent irradiation, also promotes the development of BCC. Arsenic exposure can also lead to BCC in the long term.
In addition, there are very rare hereditary disorders that are associated with increased BCC. One of these is Gorlin-Goltz syndrome (“Nevoid Basal Cell Carcinoma Syndrome”, NBCCS). This is an autosomal dominant inherited disease in which the patched receptor is mutated. Patched is part of the Hedgehog(Hh) pathway and suppresses Smoothened (SMO). If inhibition of SMO falls away, overexpression of the Hh pathway occurs. Such overexpression is also found in BCC from patients who do not have NBCCS and is therefore almost always considered a prerequisite for BCC development [6].
Subtypes of basal cell carcinoma
Over 26 different types of BCC have been described. Common are the following:
- Nodular BCC (solid BCC, nBCC): This most common subtype accounts for approximately 50% of all BCC. Characteristic of the clinically sharply circumscribed, dome-shaped tumor is a beaded, raised rim interspersed with telangiectasia. A central depression is often visible; if this is ulcerated, the diagnosis is basalioma exulcerans (Fig. 3) . Differential diagnoses include sebaceous gland hyperplasia, adnexal tumors, dermal nevi or keratoacanthomas. Deep foci can extend to the cartilage or bone and lead to increased morbidity due to sometimes considerable damage (e.g. destruction of the eye).

- Pigmented BCC: This subtype of nodular BCC can be confused with ulcerative melanoma on the one hand, and hemangiomas, melanocytic nevi or seborrheic keratoses on the other (if small) due to its dark appearance. The telangiectasias are often masked by the pigment, making clinical diagnosis difficult.
- Sclerodermiform BCC (sBCC): superficially, sBCC presents as an atrophic, slightly retracted plaque, so it can be mistaken for morphea. Subcutaneously, sBCC spreads areally in branched tumor clusters, and the borders are clinically indistinguishable. Surgically, a higher resection distance must be chosen, and ideally either a “Mohs Micrographic Surgery” or a two-stage surgery (“Slow-Mohs”) is required.
- Superficial BCC (suBCC): SuBCC is characterized by a very superficial and multicentric spread. Frequently, areas of healthy skin lie between tumor nests. Typically, there is no ulceration. The clinic may be reminiscent of nummular eczema. Because of the shallow depth of penetration, suBCC are often readily treatable with topical therapy (e.g., imiquimod).
- Metatypical BCC: Metatypical BCC is a mixed form of BCC and squamous cell carcinoma, but can only be identified histologically. Clinically, metatypical BCC resembles nBCC. Significantly, however, growth has been more aggressive.
- Metastatic BCC: Metastasis is extremely rare in BCC. It occurs particularly in large, deeply ulcerative BCC and is both lymphogenic and hematogenic, preferentially in lung and bone.
Diagnosis, degrees of risk and treatment options
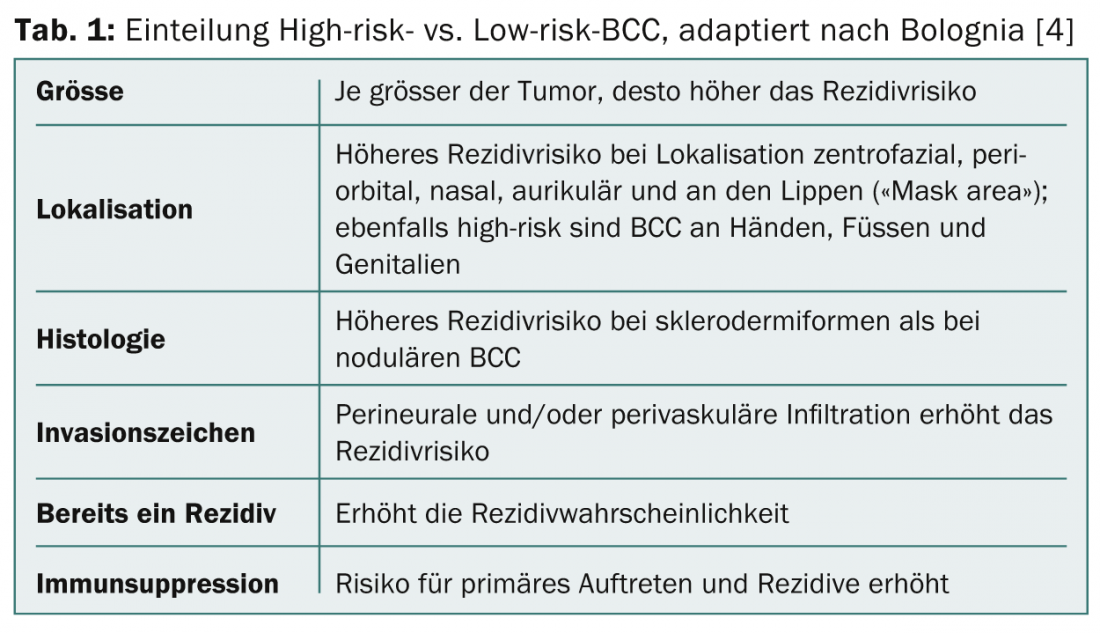
If BCC is suspected (history, location, progression), a specimen biopsy should be obtained, as this is the only way to confirm diagnoses, identify the type of BCC, and assess tumor depth. Various factors and tumor characteristics influence the risk of recurrence (Table 1) . By assessing these factors, tumors are classified into high-risk BCC and low-risk BCC.
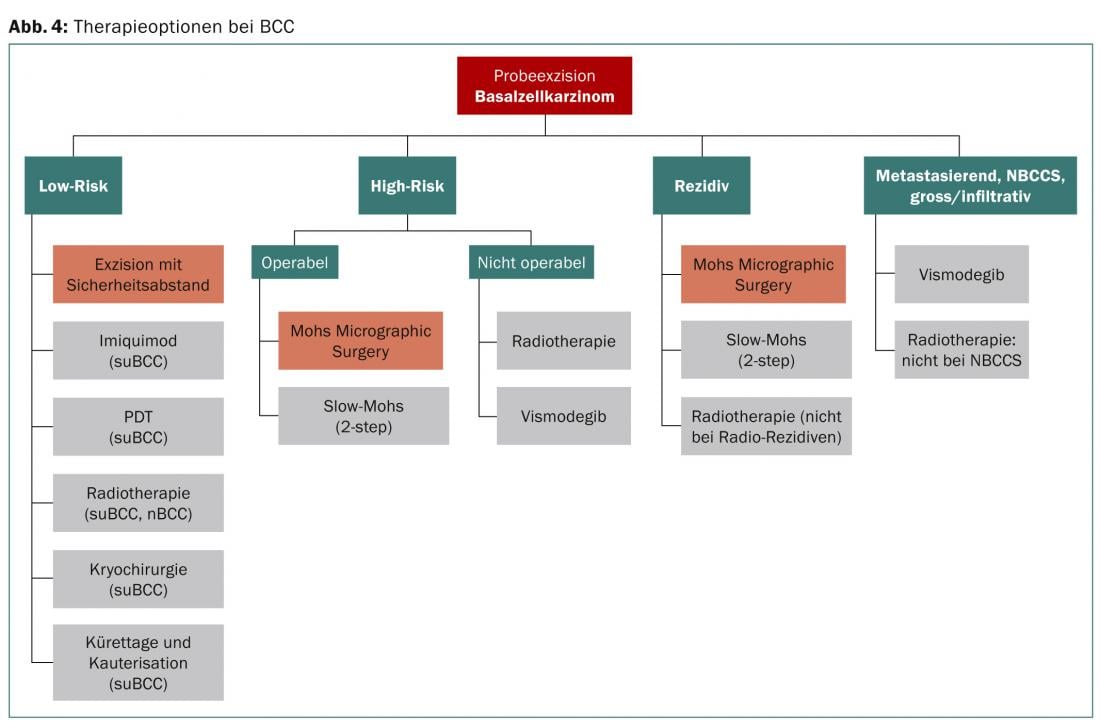
There are currently several surgical and non-surgical treatment options (Fig. 4). There are two main goals for treatment: complete removal of the tumor and a cosmetically acceptable result. For both low- and high-risk BCC, surgical excision with histologic incision margin control is the treatment of choice. For low-risk BCC, there are good alternatives, but the best long-term outcome is again achieved with surgical excision.
Surgical therapy methods
Surgical excision with safety margin: the gold standard for therapy of low-risk BCC is excision with safety margin. How large this should be depends on the tumor type and the localization (Tab. 2). In the case of a well-circumscribed BCC <20 mm, it is assumed that the probability of residual tumor is 15% at a distance of 3 mm and 5% at a distance of 4-5 mm [7,8].
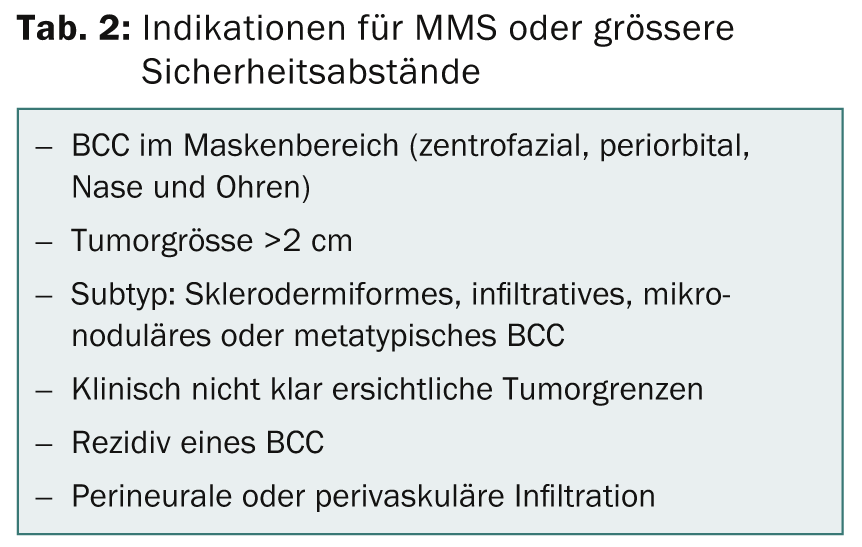
Mohs Micrographic Surgery (MMS): This procedure, developed by Dr. Mohs developed technique allows intraoperative preparation and evaluation of frozen sections. This allows residual tumor cells at incision margins to be detected and promptly ablated. The surgeon can ablate in any dimension until no tumor cells are detected. The 5-year remission rates of 99% for primary BCC and 95% for recurrence after excision make this method the gold standard for high-risk BCC [8]. The method requires specialized training of the surgeon as well as a high level of experience. Alternatively, the frozen section can be evaluated by a pathologist.
Two-stage surgery (Slow-Mohs): In two-stage surgery, a primary excision is first made with a safety margin without closure, after which the specimen is evaluated by pathologists. If the tumor has been completely removed, definitive wound care is performed in the follow-up operation, for example by means of direct closure or flapplasty. If the excision was not in toto, a new resection with histological control is performed. MMS is generally preferable because the incision margins remain close to the end of the tumor and larger safety margins are eliminated, which means a nicer cosmetic result. In the case of two-stage surgery, the intervals should be more generous. For high-risk BCC, up to 1 cm is recommended, but this is often impractical, especially in the mask zone on the face (e.g., on the lower eyelid). Here, the surgeon must weigh up the benefits and risks on an individual basis.
BCC not excised in toto: In two studies with histologically confirmed BCC not excised in toto, the post-resectate showed that residual BCC tumor cells were still detectable in only about half. The reasons are still unclear; it is possible that a cell-destructive milieu develops postoperatively, which destroys the remaining tumor cells. The best treatment method for recurrences is MMS; alternatively, a two-stage excision with a generous safety margin (5-10 mm is suggested) is performed. In some cases, adjuvant therapy with imiquimod or photodynamic therapy may be used for tumors in situ or superficial residual cells, but long-term data are not yet available.
Ablative and destructive therapy methods without histology
Curettage and cauterization: these procedures have a place in the treatment of peripheral low-risk lesions. However, combination procedures with imiquimod and photodynamic therapy (PDT) led to better results. Curettage and cauterization do not appear to be suitable for the treatment of recurrences, with a 5-year tumor-free rate of only 60% in one study [9].
Cryotherapy/cryosurgery: a quick and easy therapeutic option for low-risk BCC. Remission rates of 85-95% have been observed in randomized controlled trials [10]. Side effects include pain, erythema, and blistering and crusting; scarring and atrophy are also possible. For high-risk lesions, cryotherapy may have some value. In one study, 158 periorbital BCC were treated with cryosurgery, and the recurrence rate at 5-year follow-up was 7.6% [11].
Topical therapy with imiquimod (Aldara®) and ingenol mebutate (Picato®): Imiquimod therapy is currently approved for superficial-type BCC. A more severe skin reaction (erosions, ulcerations) leads to better results but has a negative impact on compliance, which is why a regimen of 5×/week for six weeks is recommended by the British Association of Dermatologists (BAD) for suBCC [8]. Occlusion of the therapy area does not seem to provide any benefit. There is no approval for the treatment of nBCC in Switzerland.
Ingenol mebutate has been approved in Switzerland for the treatment of actinic keratoses since 2013. Successful treatment of suBCC has been described [12], but approval for this indication is not available in Switzerland.
Photodynamic therapy (PDT) with 5-aminolevulinic acid (ALA) or methyl aminolevulinate (MAL): PDT is an option for patients suffering from large-area, difficult-to-operate suBCC or nBCC. For suBCC, the 3-year remission rate is reported to be 69-85%; for nBCC, the remission rate at 5-year follow-up is 70-82%. For nBCC, debulking should occur first at tumor thickness >2 mm. In suBCC, both ALA and MAL can be used. For nBCC, MAL is preferable because it penetrates deeper into the skin [13].
Radiotherapy: Radiotherapy still has a place in elderly patients who are inoperable or difficult to operate on. Here, radiotherapy can be used well in low-risk and conditionally in high-risk BCC and recurrences. Radiotherapy is also suitable as neoadjuvant and adjuvant therapy. The 4-year remission rate is 80% in numerous studies >.
The main side effect is radionecrosis, for which some areas such as the bridge of the nose are predestined. Other side effects include pigmentary abnormalities, telangiectasia, and radiodermatitis. Surgical excisions have a better cosmetic outcome. In NBCCS as well as xeroderma pigmentosum, radiotherapy is contraindicated because radiation damage can cause the formation of new BCC [10,14]. Also, one should not re-irradiate the recurrence of a radiotherapied BCC [8].
Vismodegib (Erivedge®): In NBCCS, a mutation causes a permanent upregulation of the Hh pathway. Vismodegib is an SMO-1 inhibitor and in this way inhibits the Hh pathway. Since 2013, vismodegib has been approved in Switzerland for the treatment of advanced, locally invasive and metastatic BCC in which other treatment options (excision, radiotherapy, etc.) would mean significant disadvantages for the patient. Side effects include muscle spasms, dysgeusia, hair loss, fatigue, nausea, and hyponatremia. Unfortunately, resistance is already apparent [15]; in the corresponding patients, SMO was altered differently depending on the site of the biopsy. Future therapeutic options targeting the Hh pathway could include itraconazole and vitamin D3, which have inhibitory effects on SMO.
Aftercare
The risk of developing a second BCC is increased after primary BCC. As the number of BCCs and age increases, so does the risk for further BCCs. In the canton of Vaud, the cumulative risk of second BCC is reported to be 20% after ten years and 40% after 20 years [2]. The following recommendations are useful for follow-up:
- Close self-monitoring of the patient. This requires a detailed explanation and instruction by the physician.
- Consistent sun protection with at least factor SPF 30.
- In the first three years after diagnosis, the risk of second BCC is highest [16]. The current guidelines in Germany (03/2012) recommend annual controls for the first three years [8].
Conclusion for practice
- BCC is the most common cancer of all. Prior to therapy, a classification is made into high-risk and low-risk BCC.
- If suspected, a trial excision is made to confirm the diagnosis.
- In both high- and low-risk BCC, surgical excision is the best therapeutic method. Noninvasive therapies may be considered for low-risk BCC when circumstances are unfavorable for surgery.
- When BCC occurs in a very young patient, NBCCS should be excluded.
- Because of the increased risk for second BCC, patients should be followed up annually for at least three years.
Dr. Omar Hasan Ali
Josef Aschwanden, MD
Lukas Flatz, MD
Literature:
- Wong CS, et al: Basal cell carcinoma. BMJ 2003; 327(7418): 794-798.
- Levi F, et al: High incidence of second basal cell skin cancers. International journal of cancer 2006; 119(6): 1505-1507.
- Reifenberger J: Basal cell carcinoma. In: Plewig G, editor. Brown-Falco’s Dermatology, Venereology and Allergology. Berlin: Springer; 2012.
- Soyer HP, et al: Actinic Keratosis, Basal Cell Carcinoma and Squamous Cell Carcinoma. In: Bolognia J, Jorizzo JL, Schaffer JV, editors. Dermatology. [Philadelphia]: Elsevier Saunders; 2012.
- Hartevelt MM, et al: Incidence of skin cancer after renal transplantation in The Netherlands. Transplantation 1990; 49(3): 506-509.
- Kasper M, et al: Basal cell carcinoma – molecular biology and potential new therapies. The Journal of clinical investigation 2012; 122(2): 455-463.
- Hauschild A, et al: Brief S2k guidelines–Basal cell carcinoma of the skin. Journal of the German Society of Dermatology 2013; 11 Suppl 3: 10-15, 1-6.
- Telfer NR, et al: Guidelines for the management of basal cell carcinoma. The British journal of dermatology 2008; 159(1): 35-48.
- Rowe DE, et al: Mohs surgery is the treatment of choice for recurrent (previously treated) basal cell carcinoma. The Journal of dermatologic surgery and oncology 1989; 15(4): 424-431.
- Berking C, et al: Basal cell carcinoma-treatments for the most common skin cancer. Deutsches Ärzteblatt international 2014; 111(22): 389-395.
- Tuppurainen K: Cryotherapy for eyelid and periocular basal cell carcinomas: outcome in 166 cases over an 8-year period. Graefe’s archive for clinical and experimental ophthalmology 1995; 233(4): 205-208.
- Siller G, et al: PEP005 (ingenol mebutate) gel for the topical treatment of superficial basal cell carcinoma: results of a randomized phase IIa trial. The Australasian journal of dermatology 2010; 51(2): 99-105.
- Braathen LR, et al: Guidelines on the use of photodynamic therapy for nonmelanoma skin cancer: an international consensus. J of the American Academy of Dermatology 2007; 56(1): 125-143.
- Kimonis VE, et al: Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. American journal of medical genetics 1997; 69(3): 299-308.
- Brinkhuizen T, et al: Acquired resistance to the Hedgehog pathway inhibitor vismodegib due to smoothened mutations in treatment of locally advanced basal cell carcinoma. J Am Acad Dermatol 2014. pii: S0190-9622(14): 1792-1797.
- Marcil I, et al: Risk of developing a subsequent nonmelanoma skin cancer in patients with a history of nonmelanoma skin cancer: a critical review of the literature and meta-analysis. Archives of dermatology 2000; 136(12): 1524-1530.
InFo ONCOLOGY & HEMATOLOGY 2014; 2(9): 8-13.











