Depression wants to be accurately diagnosed and specifically treated. In Switzerland, up to 20% of the population is affected – in varying degrees. However, because depression is a clinical diagnosis, it is not always easy to know which path to take. But prolonged dithering is not advisable. It is preferable to treat according to guidelines and to select the drug on the basis of symptoms.
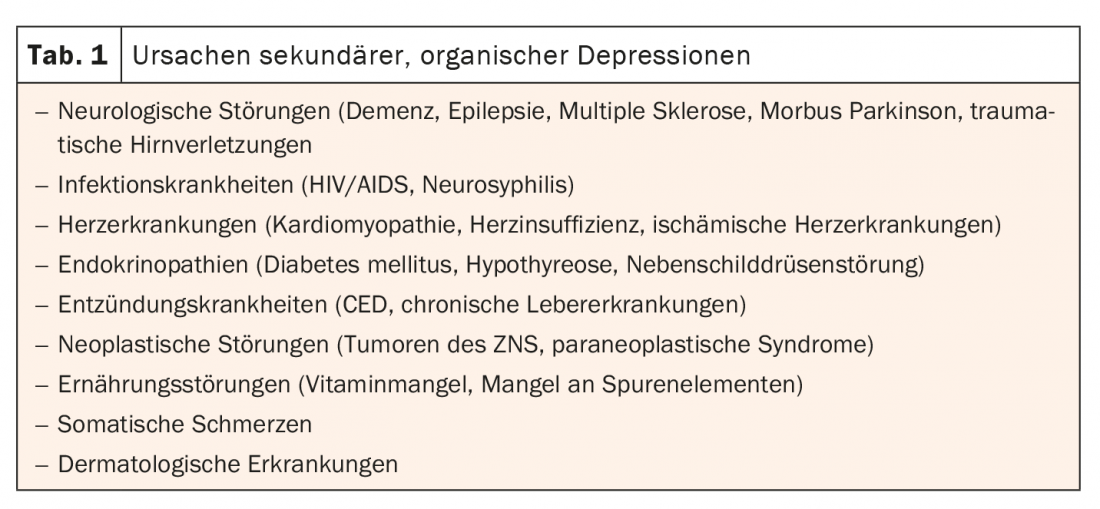
Not all depression is the same. In addition, the symptoms of depression can hide a variety of other diseases. In addition to the main symptoms of depressed mood, loss of interest, joylessness, lack of drive and increased fatigue, there may be other additional symptoms. These include decreased concentration and attention, decreased self-esteem and self-confidence, feelings of guilt and worthlessness, negative and pessimistic outlook on the future, sleep disturbances, decreased appetite, and/or suicidal ideation. Therefore, a comprehensive medical history, physical-neurological findings, and technical examinations including thyroid parameters, iron metabolism, EEG, and MRI are important for differentiated diagnosis. This approach serves to differentiate symptomatic depression from organic depression. Symptomatic depression usually occurs postoperatively, postinfectiously, endocrine, or pharmacogenically. In organic depression, the cause is more likely to be, for example, the presence of dementia or a brain tumor (Table 1) .
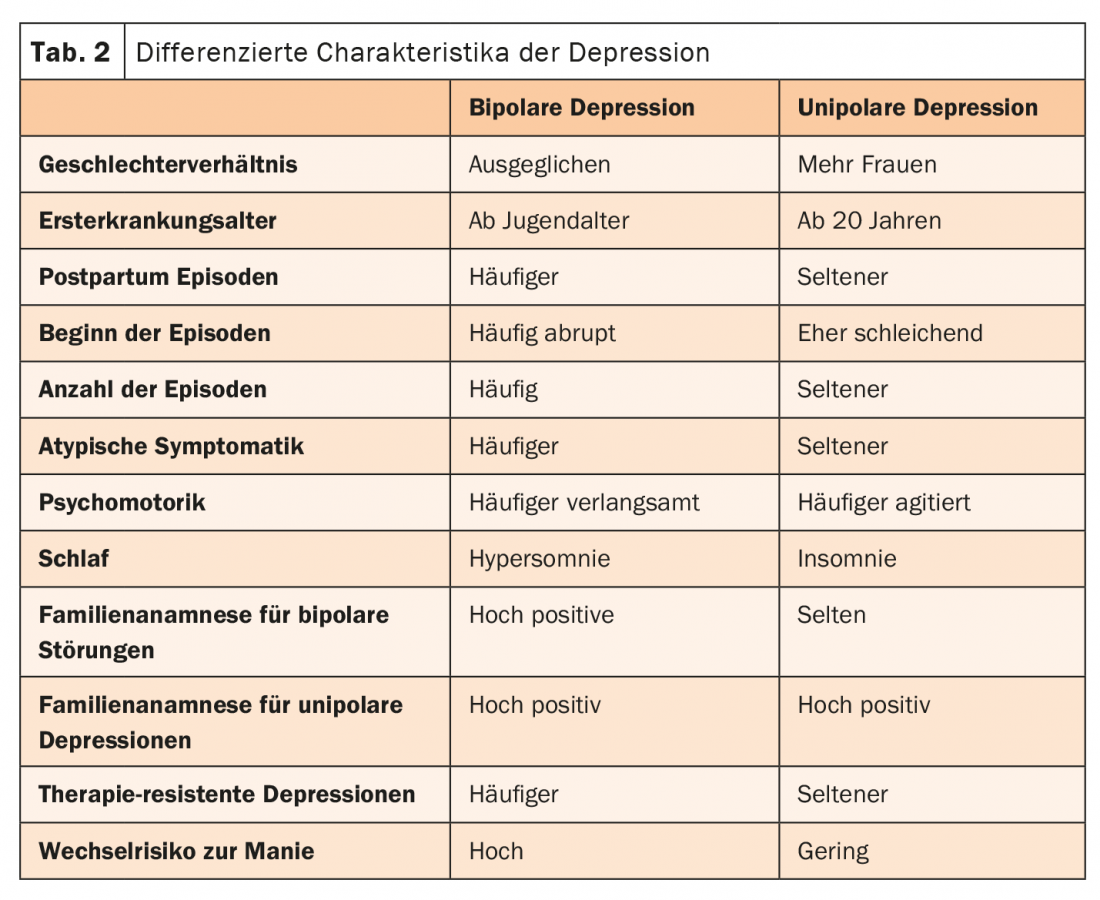
Screening forms can be used for further clarification. The Suicide status form, WHO-5 well-being questionnaire, or patient health questionnaire (PHQ-D) can provide further insight into patients’ mental lives. Third-party assessment questionnaires such as the HAM-D or the Montgomery-Åsberg Depression Rating Scale (MADRS) complete the picture. Neurobiological markers of depression include immune, electrophysiological, endocrine, as well as CNS-associated markers, in addition to genetic and environmental factors and the cognitive symptoms already described. For example, cortisol, IL-6, IFN-gamma and triglycerides are increased, cholesterol, iron, B12 or also BDNF are reduced, as Prof. Dr. med. Thomas J. Müller, Meiringen/Bern, pointed out. The question is whether there are predictors that can predict diagnosis or even response to a drug. In fact, there are certain characteristics that can be differentiated, at least in terms of bipolar or unipolar depression (Table 2) .
Individual approach relies on participatory decision making
After education and psychoeducation, the treatment algorithm relies on participatory decision making to elicit the individually appropriate course of action. While an active wait-and-see approach for 14 days may be considered for a mild form of depression, psychotherapy and/or pharmacotherapy should be started immediately for moderate or severe depression. With the help of close monitoring, therapy can be adjusted or supplemented as needed. For acute treatment of bipolar depression, the 2019 update recommends combination treatment of quetiapine/quetiapine XR or lithium in combination with an antidepressant. SSRIs (with the exception of paroxetine) and bupropion are most likely to be recommended for this purpose.
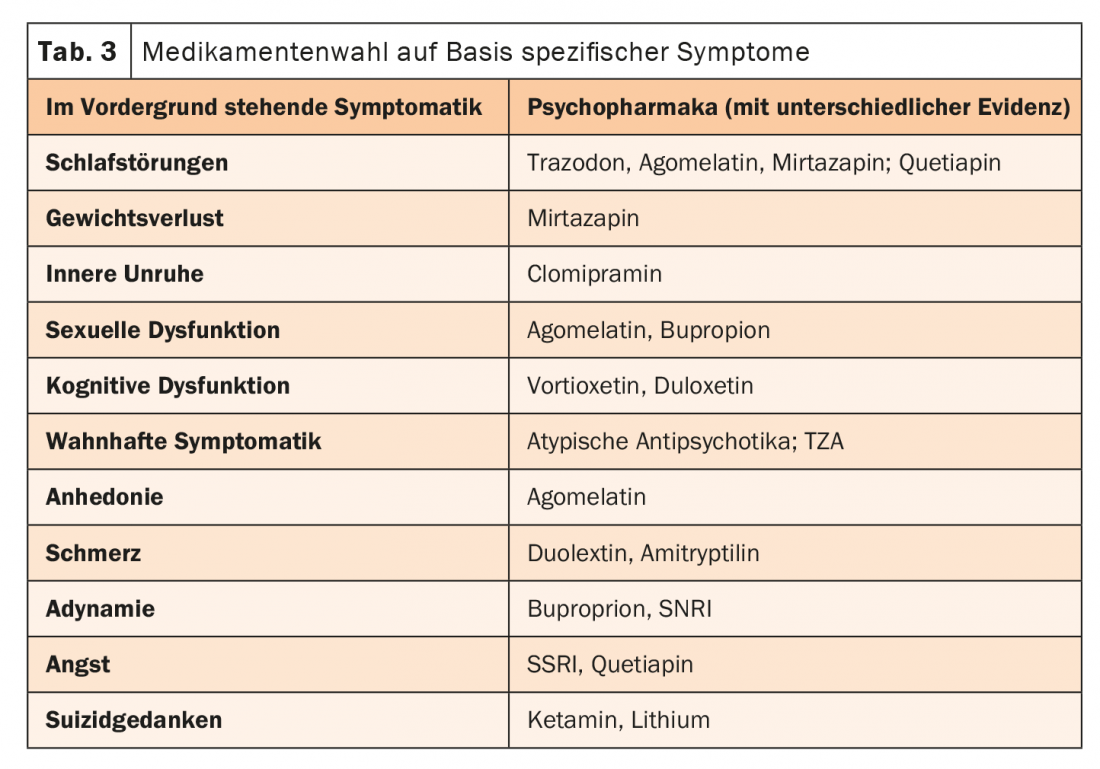
Which antidepressant is ultimately used can be decided, for example, on the basis of the psychomotor effect. Amitriptyline, doxepin, and trimipramine have more sedative-anxiolytic effects. SSRIs, MAO inhibitors, venlafaxine, desipramine, and nortriptyline, on the other hand, are less sedating. Imipramine and clomipramine are mildly sedating and activating, respectively, for this purpose, as the expert pointed out to the Kielholz scheme. Ultimately, selection should be based on the specific symptoms, with classification based on experience (tab. 3) . The study situation is not clear in this respect.
Congress: FomF Update Refresher
InFo NEUROLOGY & PSYCHIATRY 2021; 19(4): 26-27 (published 8/21, ahead of print).











