Dear colleagues, can you imagine that in an emergency department, when a heart attack is suspected, a registration to the cath lab is made without an ECG being derived beforehand? Of course, this question is purely rhetorical; all the more reason to occasionally wonder how often bronchodilator and also anti-inflammatory inhalative therapy is started in patients with dyspnea without prior diagnosis and the effect is awaited. Uncritically equating dyspnea for prolonged periods with bronchial obstruction and an indication for combination therapy with a beta stimulator and a corticosteroid may lead to incorrect, unnecessary, or even harmful therapies. In a study of a group practice outpatient clinic, for example, a purely clinical diagnosis of asthma could not be confirmed in almost one third of the patients. Vocal cord dysfunction, hyperventilation, tracheal stenosis, and functional causes can present in confusingly similar ways.
In this issue of HAUSARZT PRAXIS with an article on dyspnea in general and COPD as one of the common diseases with this leading symptom, it is shown how far you can already get in practice with history, clinic and a simple technical examination.
Also, basing a COPD diagnosis solely on a tobacco history associated with dyspnea does not do justice to many patients. A simple spirometrically proven obstruction in practice and its severity as well as the lack of response of bronchial obstruction to betamimetics together with the medical history are sufficient to determine the stage of COPD including the new GOLD risk classification (A,B,C,D) and thus also to initiate a stage-appropriate therapy.
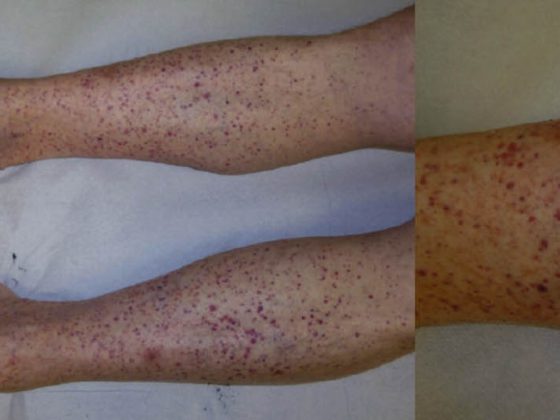
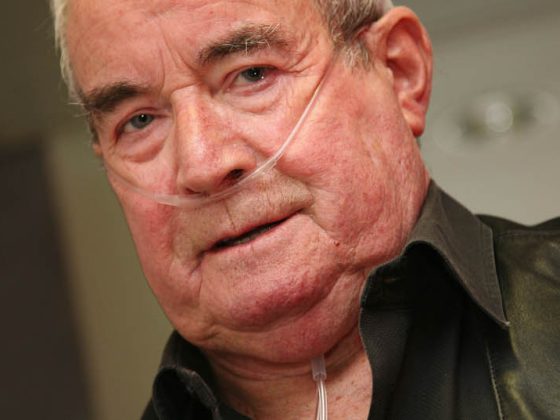
In 1964, i.e. 50 years ago, the two extreme phenotypes of COPD, the “blue bloater” and “pink puffer”, were described in the “Blue Journal”, the most renowned pneumological journal. This memorable engram is still with most of us. Today, refined phenotyping of diseases, including COPD, is becoming increasingly important to provide individualized therapies. Patients differ in their inflammatory pattern, exacerbation frequency, comorbidities, or emphysema type, to name a few. This has made the disease COPD, previously considered almost hopeless and chronic-progressive, interesting again and much more grateful in treatment. What will probably endure for all time is the recurring call to stop tobacco if one wants to prevent the 4000 COPD deaths per year in Switzerland.
Prof. Dr. med. Robert Thurnheer
HAUSARZT PRAXIS 2014; 9(8): 13