Exogenous allergic alveolitis (EAA) is in itself a very rare disease. So when we talk about common and rare triggers of EAA, we are dealing with very small numbers of cases. In addition, there are strong regional and occupational differences. An expert explained how best to track down the triggers of the disease.
Whereas in German-speaking countries the term exogenous allergic alveolitis is still preferred, the term hypersensitivity pneumonitis (HP) has now become established in English and has largely replaced extrinsic allergic alveolitis, explained Dr. Marcus Joest, Allergology and Immunology Laboratory, Bonn Lung and Allergy Center, by way of introduction. In the U.S., the annual incidence (2004-2013) is 1.28-1.94/100 000 population, and the prevalence is 1.67-2.71/100 000. “This almost meets the requirements for an orphan disease definition.” However, the risk is significantly increased in certain collectives, including bird owners and farmers, for example.
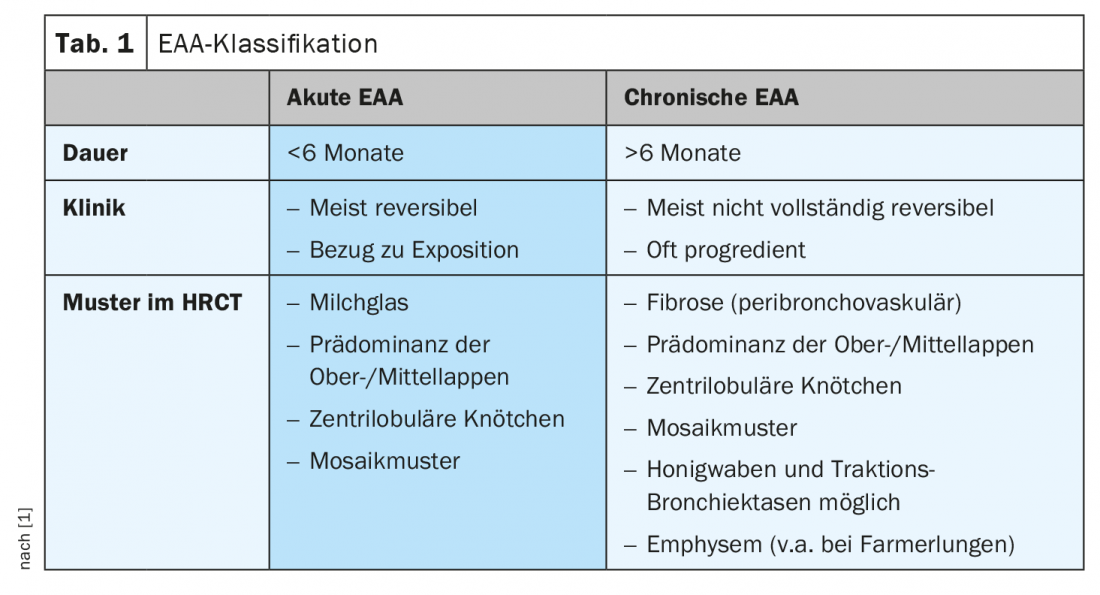
With regard to immunology, it used to be referred to as an immune complex reaction (type 3), but today it is more commonly referred to as a complex immune reaction. It is classified as acute (<6 months) and chronic (>6 months) EAA. Acute EAA is usually reversible, and often a link to exposure can be found anamnestically (Tab. 1). However, not every chronic course must end in fibrosis; there are also chronic non-fibrosing EAAs.
Division into 5 classes
Diagnostic criteria for acute EAA include primarily exposure, recurrent symptoms 4-8 hours after exposure, elevated IgG antibodies to candidate allergens, esp. Crackle and matching HRCT findings. For chronic EAA, in addition to exposure, it is elevated IgG antibodies or BAL lymphocytosis, decreased DLCO or hypoxemia, matching HRCT, matching lung biopsy, positive inhaled provocation, or improvement after abstinence.
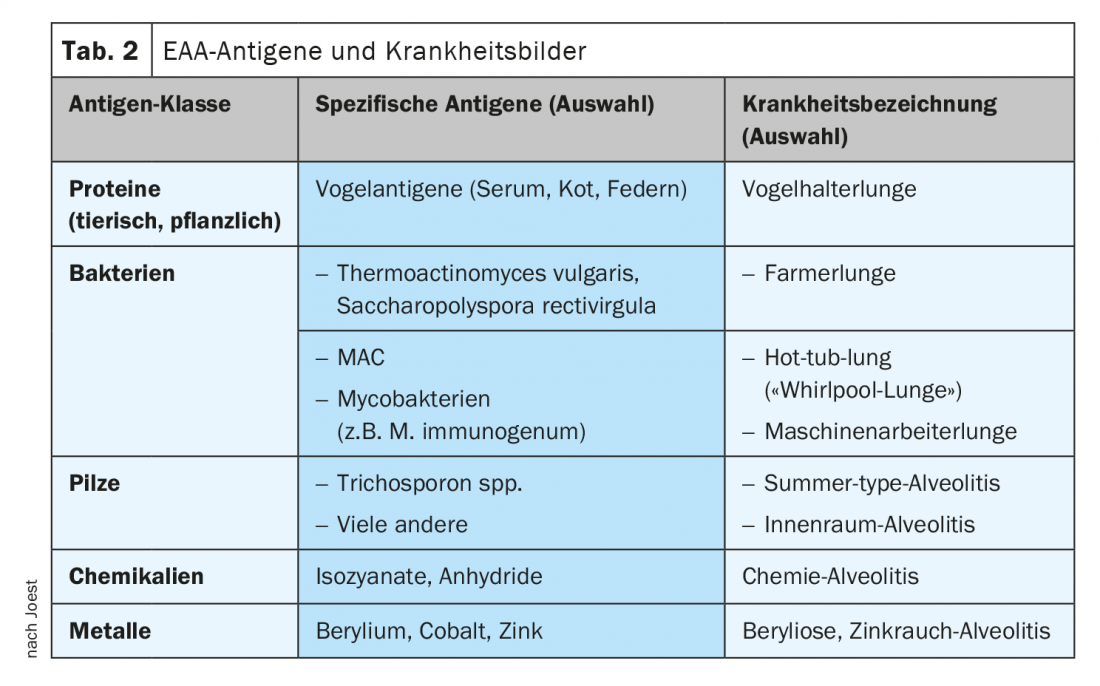
EAA antigens can be broadly divided into 5 classes, with proteins, bacteria, and fungi being the most common (Tab. 2). With regard to the triggers of EAA, according to Dr. Joest, it is important to distinguish between antigens and antigen sources. “For us as clinicians, the antigen sources are the information we can find out anamnestically. We usually can’t find out from the patient which bacterium or mold triggered the EAA, but rather a source.” The allergist cited a bagpipe as an example of a reservoir of various bacteria and fungi. Another source of antigen is the Jacuzzi, also called a whirlpool or hot tub in English. Here, as in metalworking with cooling lubricants (MWF), non-tuberculous mycobacteria (NTM) can be the trigger of EAA. In the case of KSS, a working group had also highlighted a number of other pathogens (including Pseudomonas, Fusarium, Aspergillus). Different germ spectra (Sphingobacterium spitivorum, Bacillus, Pseudomonas app. Stenotrophomonas) can also be found in sources such as room fountains or steam irons, which can lead to so-called “humidifier lung”.
Large regional differences
There are large regional differences in the differentiation between frequent and rare triggers: In India, for example, so-called “air coolers”, which are not found at all in Central Europe, are a frequent source of antigens. In Japan, summer type alveolitis caused by Trichosporon spp. is endemic; in Europe, it is practically absent. And in France, Absidia (Lichtheimia) corymbifera is a common proven farmer’s lung antigen, but for which there are few and indirect (serological) data outside France. A recent review [2] was based on a literature search spanning 30 years (1990-2020) that included 967 studies. Analysis of the frequency of various exposures in EAA patients revealed that bird lung was the most common in all forms at nearly 29%, with farm lung following at 16% and mold (general) at 13%. In 17% of patients in this analysis, the source remained unknown.
Is it even worth the effort to find the trigger of the EAA? Dr. Joest answered this question unequivocally in the affirmative: the survival rate after diagnosis of EAA in patients with identification of the allergen is 8.75 years, while that of those without identification is only 4.88 years. As long as EAA has not yet progressed to a chronic progressive form, allergen avoidance is the most important form of therapy. The other therapies – both a systemic steroid administration as an acute therapy or alternatively immunosuppressants or in the advanced fibrotic forms also an antifibrotic therapy – are always only slowing down the progression, while the allergen abstinence can actually bring a cure.
Source: Lecture “Common and rare triggers of EAA” in the session “Rare Allergies in Pneumology”. 61st Congress of the German Society for Pneumology and Respiratory Medicine e.V., 5.06.2021.
Congress: DGP 2021 digital
Literature:
- Vasakova M, et al: Hypersensitivity pneumonitis: perspectives in diagnosis and management. American Journal of Respiratory and Critical Care Medicine 2017; 196 (6): 680-689; doi: 10.1164/rccm.201611-2201PP.
- Barnes H, et al: Exposures and associations with clinical phenotypes in hypersensitivity pneumonitis: A scoping review. Respir Med 2021; 184: 106444; doi: 10.1016/j.rmed.2021.106444.
InFo PNEUMOLOGY & ALLERGOLOGY 2021; 3(3): 31-32 (published 9/17-21, ahead of print).