Supraventricular tachycardia (SVT) occurs in the general population with a prevalence of approximately 2-3/1000 population. Many people can be helped by adequate diagnosis and treatment of arrhythmias, and the correct finding of an ECG in SVT is important for every medical professional.
Supraventricular tachycardia (SVT) occurs in the general population with a prevalence of approximately 2-3/1000 population. By definition, supraventricular tachycardia is based on atrial frequencies of >100 beats per minute under resting conditions and the excitation propagation of SVT is via the His bundle or higher structures [1].
The European Society of Cardiology (ESC) recently published a comprehensive guideline that focused on the diagnosis and clinical management of SVTs and summarized the progress of the last 10 years of a rapidly evolving field [2]. In addition to general aspects of the clinical approach, a correct ECG diagnosis is necessary, but often difficult for physicians with little experience in the treatment of cardiac arrhythmias. Therefore, the aim of this article is to present the important aspects of ECG diagnostics in a simplified way [1,2]. Regarding the clinical procedure, we recommend the reader to read another publication of our research group: [3].
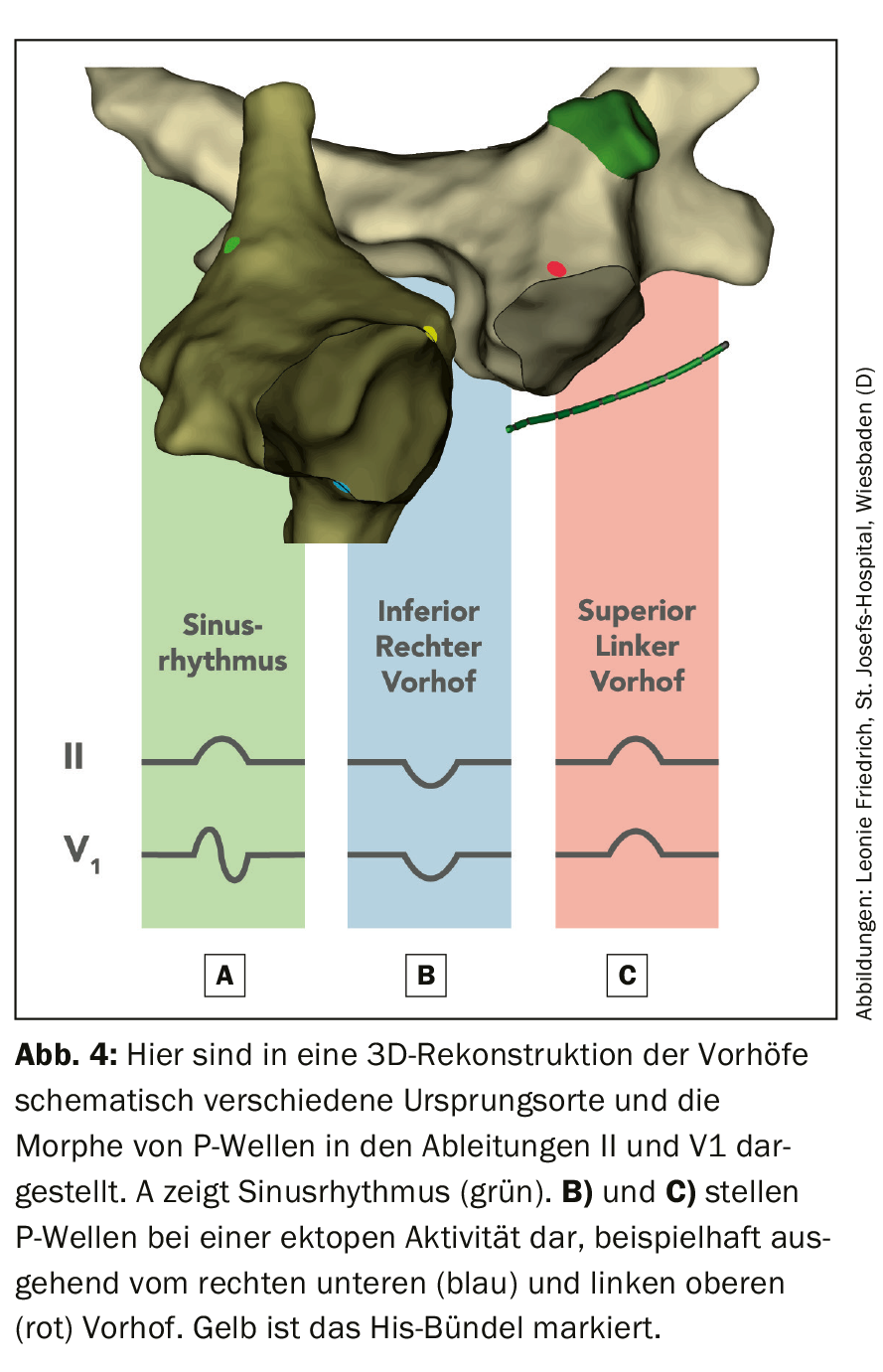
In general, an attempt should be made to document SVT on a 12-lead ECG to diagnose the arrhythmia. A comparison with the resting ECG may also be helpful (e.g., presence of preexcitation, Fig. 1) . If the ECG documentation is unsuccessful, an electrophysiological examination with possible catheter ablation can be indicated in patients with a directional history (overview 1).
Narrow complex tachycardia
SVTs that activate the heart via the His-Purkinje system typically present as narrow complex tachycardia (QRS <120 ms). In rare cases, early His bundle activation may also occur in highly septal ventricular tachycardia (VT), resulting in narrow complex tachycardia.
Individual arrhythmias often underlie specific ECG changes, and comparison of the tachycardia ECG with the resting ECG is recommended (Fig. 1).
Atrial tachycardias (AT) often show QRS complexes unchanged from the resting ECG (Fig. 1A), often starting with successive acceleration and ending with deceleration of the heart rate. Irregular tachycardias may be focal or multifocal ATs as well as atrial fibrillation and atrial flutter with alternating AV conduction. Atrial fibrillation is the most common cause. Atrial flutter often shows regular AV conduction (Fig. 1B), although 2:1 conduction with masked flutter waves occasionally presents a diagnostic challenge. In the presence of very rapid AV conduction, “pseudo”-regularized atrial fibrillation must also be considered for differential diagnosis. In contrast, SVTs with reentry mechanisms are never irregular [4].
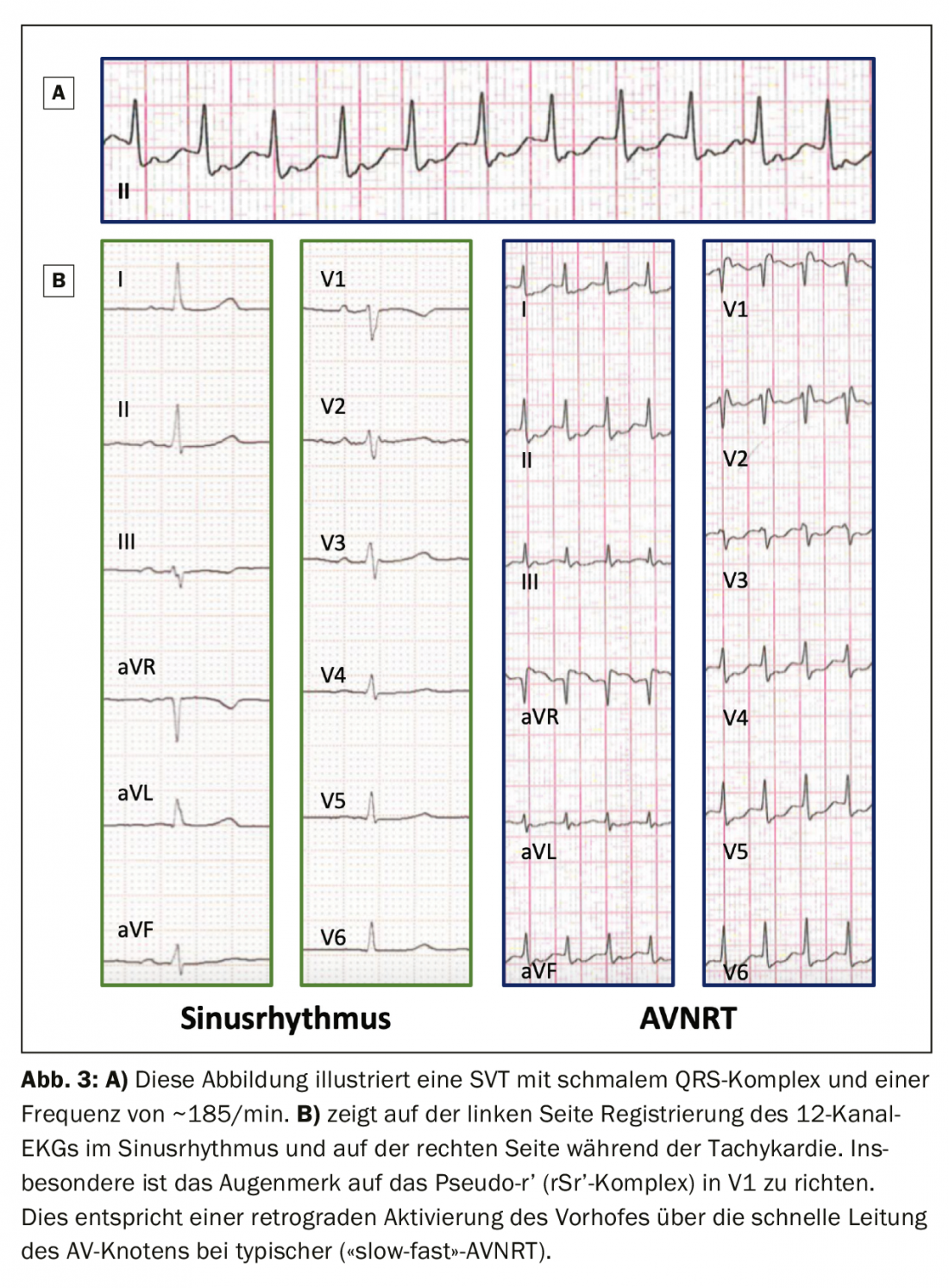
A typical (so-called “slow-fast” AV nodal reentry tachycardia = AVNRT) leads to a “pseudo-R'” due to the fast (“fast”) retrograde conduction (in V1) or “pseudo-S” (in inferior leads, box in Figure 1C). Typical for this rhythm disturbance are an abrupt onset – mostly triggered by a supraventricular extrasystole – and a similar termination. Premature ventricular beats are more likely to trigger atypical AVNRT (the reentry circuit runs in the opposite direction of a typical AV nodal reentry tachycardia) or AV reentry tachycardia (AVRT).
Preexcitation (premature excitation of the ventricle) on resting ECG (Fig. 1D) may be diagnostically suggestive even in the absence of tachycardia documentation. However, lack of preexcitation does not exclude AVRT, because orthodromic tachycardia (tachycardia with ventricular excitation along the physiological conduction system) can occur via a so-called “hidden” conduction pathway with only retrograde (ventriculo-atrial) conduction properties.
R/P ratio and P-wave morphology
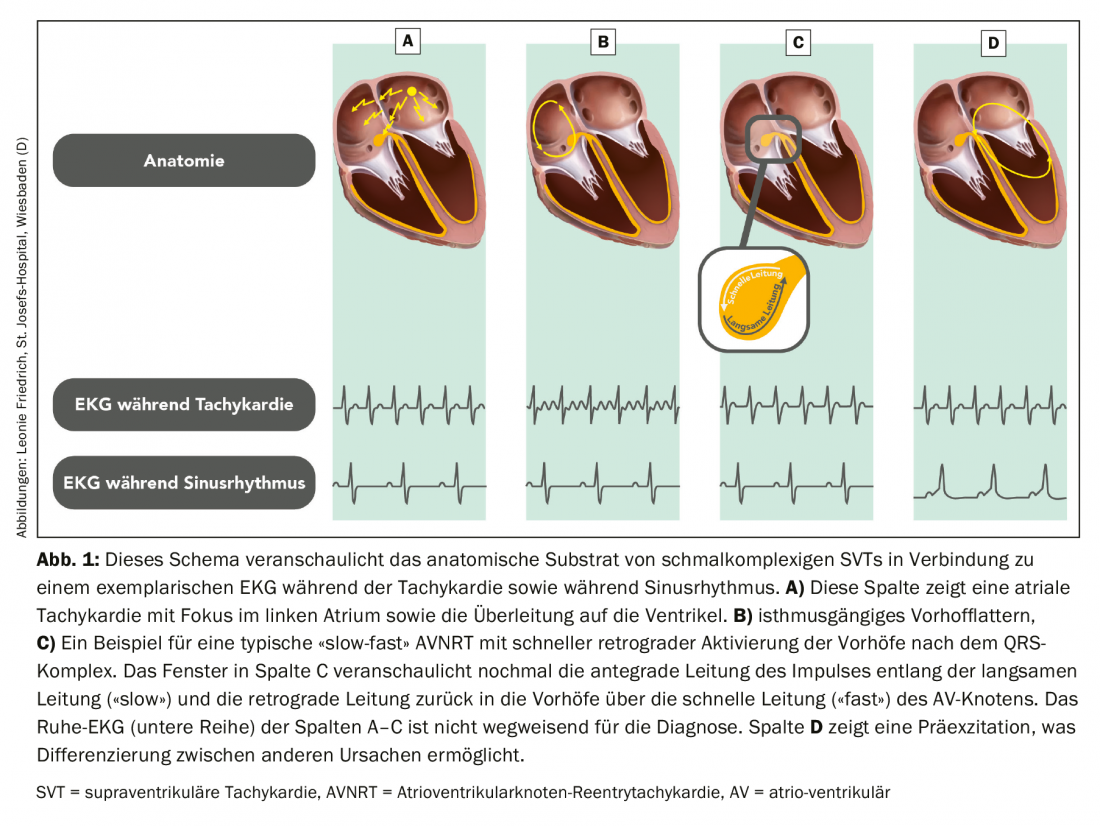
Narrow complex tachycardias can be divided into long and short RP interval tachycardias. Tachycardias with short RP interval are characterized by RP interval <50% than RR interval of tachycardia, whereas SVTs with long RP are characterized by RP > PR (Fig. 2).
A very short RP interval indicates rapid retrograde atrial excitation as in the case of typical (“slow-fast”) AVNRT or AT, but less frequent here. Precise measurement of the RP interval on surface ECG is difficult, but a cut-off of 90 ms can be adopted for differentiation between typical AVNRT from atypical or AVRT [5]. Rapidly retrogradely conducted P waves may appear in the form of a “pseudo-R” in V1 and/or “pseudo-S” in the inferior leads, which are not present in the resting ECG (Fig. 1C). These features are more usually seen in a typical AVNRT (Fig. 3) than in AVRT due to an accessory pathway or AT [1].
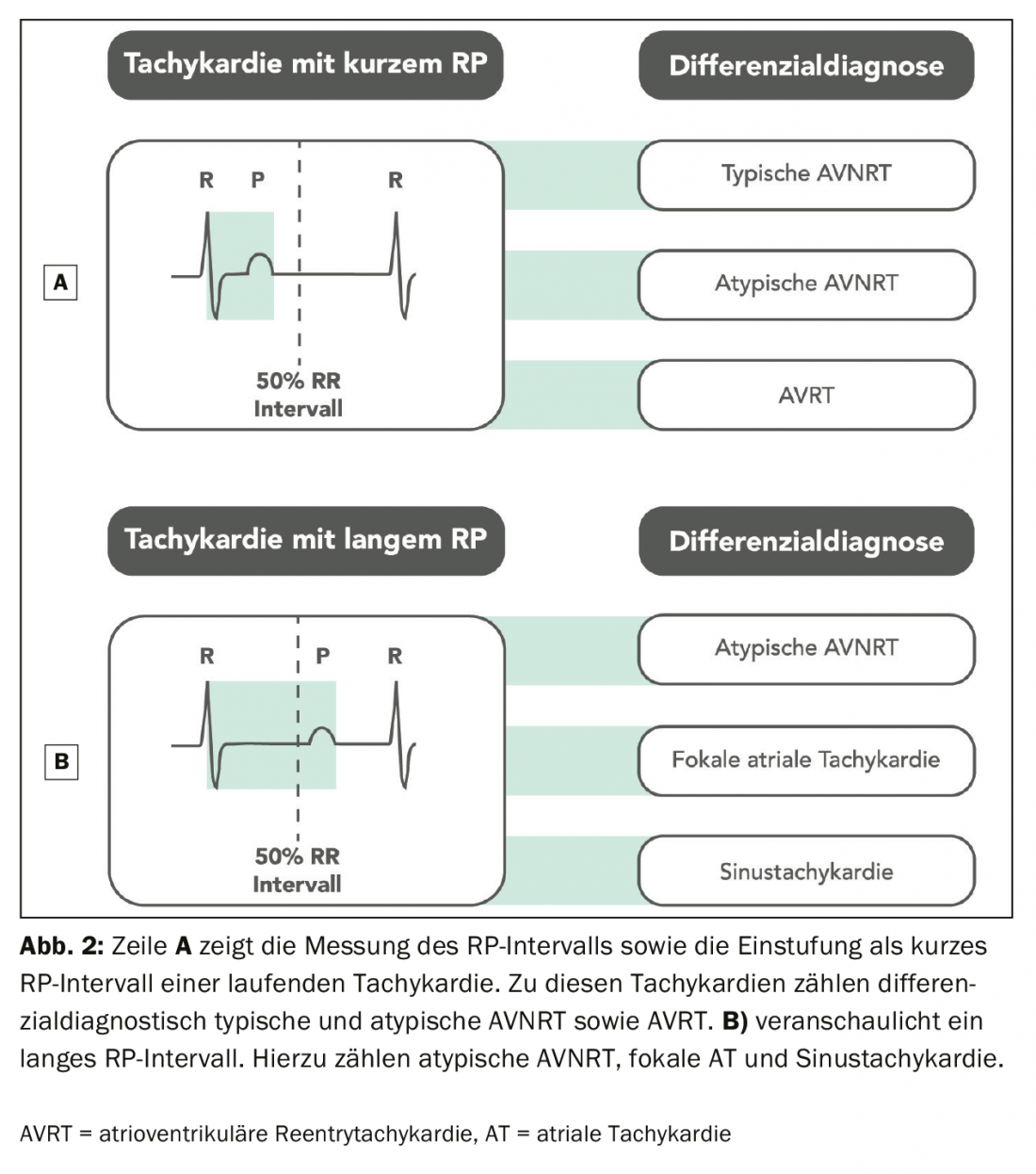
In addition to the P/R ratio, the morphology of the P-wave is important. P waves with morphology similar to normal sinus rhythm indicate adequate or inadequate sinus tachycardia, sinus node reentry tachycardia, or AT with a focus near the sinus node. P waves different from sinus rhythm with different AV conduction are typically found in ATs. In this case, the P-wave morphology may indicate the locality of the AT focus. For example, positive P waves in V1 and negative P waves in derivative I indicate a left atrial origin (Fig. 4).
Broad complex tachycardia
Analysis of wide-complex tachycardia (QRS >120 ms) is often more difficult. SVTs may manifest as wide-complex tachycardia in the presence of preexisting or functional bundle branch block, drug-induced conduction slowing, antegrade conduction accessory pathway, or an atrial sensed ventricular paced rhythm in patients with pacemakers. SVTs with wide ventricular complexes may further be caused by electrolyte disturbances or drugs. Antiarrhythmic drugs are typical drugs that can cause QRS widening [6,7]. Functional tachycardia-related right bundle branch block (RSB) is more common than functional left bundle branch block (LSB) because of the longer refractory period of the right bundle branch. Thigh blocks can occur with any SVT or sinus tachycardia. The goal of ECG interpretation of broad complex tachycardia is to distinguish SVT from VT.
Atrioventricular dissociation
AV dissociation is an evidential ECG criterion of VT and is characterized by atrial activity independent of ventricular activation. The ratio of atrial to ventricular activity is usually 1:1 or higher (more P waves than QRS complexes) in SVTs. Although ventriculo-atrial conduction is also present in up to 50% of patients with VT and a 1:1 ratio is possible, the ratio in VT is often less than 1:1 (more QRS complexes than P waves). Detection of AV dissociation is often difficult because the P waves are usually hidden in the QRS complexes or T waves. P waves are generally best identified in the inferior and chest wall leads [8].
Fusion and capture strokes
Particularly in VTs with a rate of ~100-120 beats per minute, occasional isolated sinus beats transmitted to the ventricles can be identified on the basis of altered QRS morphology. During recurrent ventricular activity, short excitable gaps exist that can be captured by or fused with isolated sinus beats (hence the name “capture” and “fusion” beats). The morphology of these beats is a combination of the VT morphology and the corresponding sinus rhythm (Fig. 5).
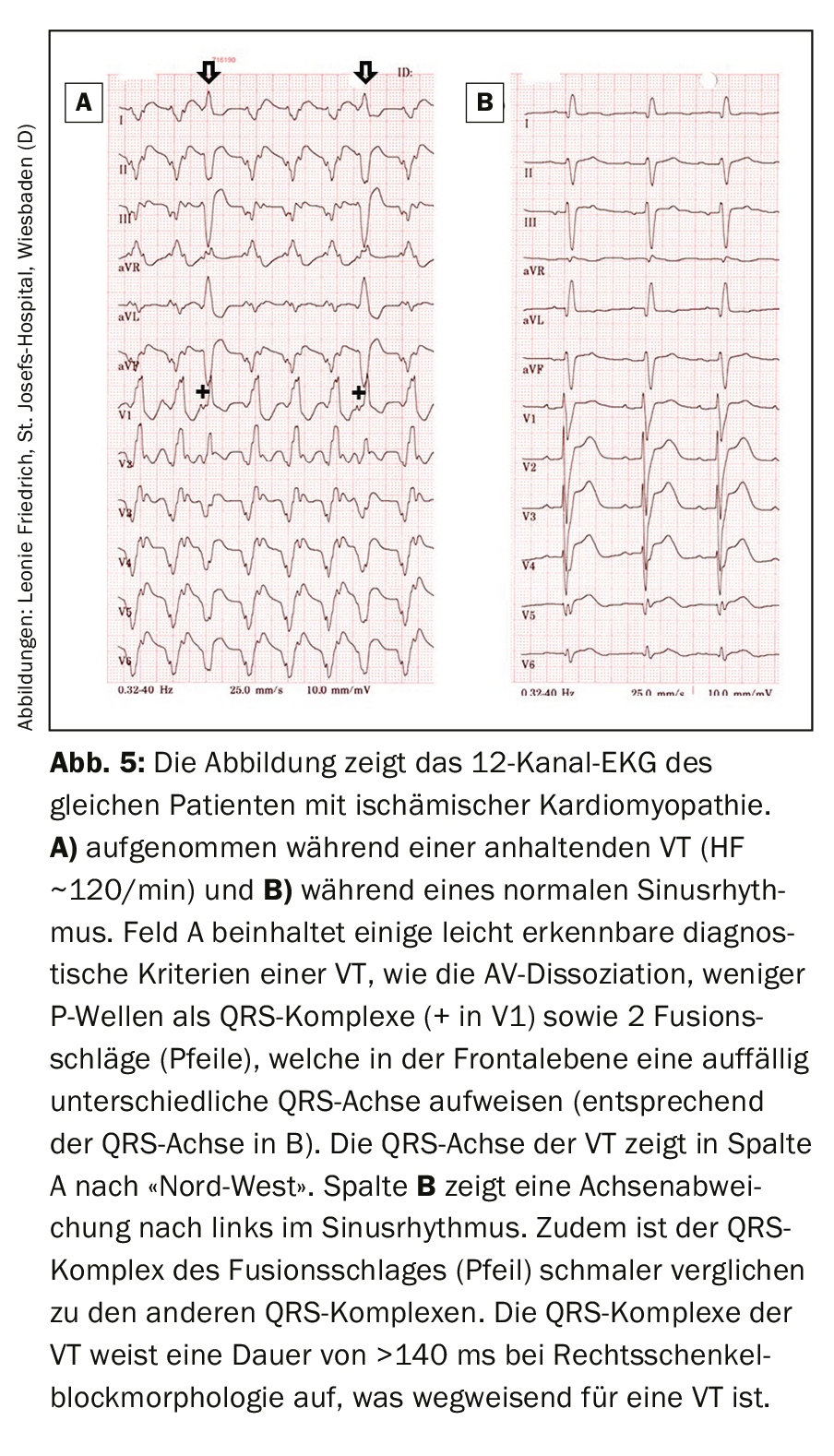
QRS duration and QRS axis
The probability of VT increases with RSB with QRS >140 ms and LSB with QRS >160 ms. In addition, the QRS axis can be helpful in the interpretation. The QRS axis of an SVT with aberrancy is usually limited to -60° to +120°. Therefore, a QRS axis of a broad complex tachycardia outside this range suggests the presence of a VT (Fig. 6) . In particular, an extreme axis deviation of -90° to +180° (“north-west” axis in the Cabrera circle) indicates a VT. Therefore, predominantly negative QRS complexes in leads I, II, and III (which depict this extreme axis deviation) are useful criteria for detecting VT.

The differential diagnosis of broad complex tachycardia on 12-lead ECG is often challenging even for experts. The discussion of detailed morphological criteria as well as the application of different algorithms is beyond the scope of this paper. In this regard, we refer the reader to the corresponding excellent works [1,2].
In summary, many people can be helped by adequate diagnosis and treatment of cardiac arrhythmias and the correct finding of an ECG in SVT is important for every medical professional.
Take-Home Messages
- Recording a 12-lead ECG is important in ongoing tachycardia in stable patients.
- In broad-complex tachycardia, the presence of AV dissociation and fusion and capture beats is probative of ventricular tachycardia.
- In wide-complex tachycardia, the “north-west” axis of QRS is indicative of ventricular tachycardia.
Literature:
- Katritsis DG, Boriani G, Cosio FG, et al: European Heart Rhythm Association (EHRA) consensus document on the management of supraventricular arrhythmias, endorsed by Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiologia (SOLAECE). Europace 2017; 19(3): 465-511.
- Brugada J, Katritsis DG, Arbelo E, et al: 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J 2020; 41(5): 655-720.
- Boehmer AA, Rothe M, Soether CM, et al: Procedure and treatment options for supraventricular tachycardia. Dtsch Med Wochenschr 2020, in press.
- Jais P, Matsuo S, Knecht S et al: A deductive mapping strategy for atrial tachycardia following atrial fibrillation ablation: importance of localized reentry. J Cardiovasc Electrophysiol 2009; 20(5): 480-491.
- Letsas KP, Weber R, Siklody CH, et al: Electrocardiographic differentiation of common type atrioventricular nodal reentrant tachycardia from atrioventricular reciprocating tachycardia via a concealed accessory pathway. Acta Cardiol 2010; 65(2): 171-176.
- Crijns HJ, Kingma JH, Gosselink AT, et al: Sequential bilateral bundle branch block during dofetilide, a new class III antiarrhythmic agent, in a patient with atrial fibrillation. J Cardiovasc Electrophysiol 1993; 4(4): 459-466.
- Crijns HJ, van Gelder IC, Lie KI: Supraventricular tachycardia mimicking ventricular tachycardia during flecainide treatment. Am J Cardiol 1988; 62(17): 1303-1306.
- Alzand BS, Crijns HJ: Diagnostic criteria of broad QRS complex tachycardia: decades of evolution. Europace 2011; 13(4): 465-472.
FAMILY PRACTICE 2020: 15(8): 12-16