Fixed combinations can simplify the therapy management of hypertension and improve adherence – these are statements that are now generally accepted. Accordingly, the administration of fixed combinations is also recommended in the European guidelines. This is because effective blood pressure reduction is indicated from the outset, particularly in view of possible cardiovascular consequences.
Ischemic heart disease and stroke occupy the top two positions worldwide in terms of leading causes of mortality. Nearly 18 million people die annually due to cardiovascular heart disease, pointed out PD Emrush Rexhaj, MD, Bern. Thus, this cause accounts for 31% of all deaths worldwide [1]. The risk factors for developing cardiovascular disease are broad and range from smoking to obesity to diabetes. The greatest danger, however, comes from arterial hypertension. For every 1 mmHg increase in systolic blood pressure, the risk of a lethal stroke also increases by 1%, the expert said. If blood pressure increases at a ratio of 20/10 mmHg, cardiovascular risk increases by 50% [2].
Given that the proportion of patients with hypertension has doubled from 648 million sufferers to 1278 million patients within the last 30 years, effective treatment management appears essential [3]. In fact, individuals aged 55 years with normal blood pressure have a greater than 90% risk of developing hypertension within the next 25 years [4].
Reduce cardiovascular risk
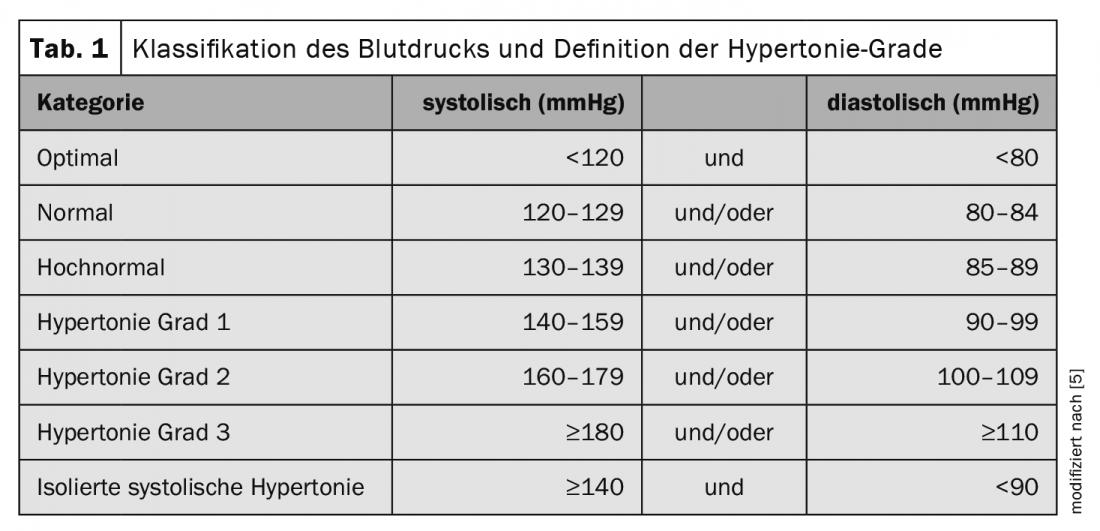
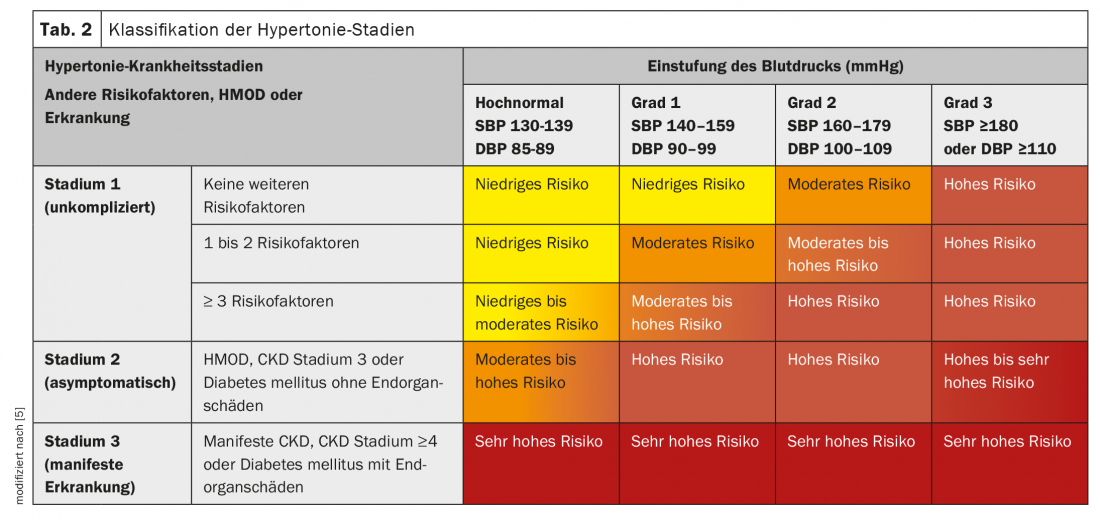
The 2018 blood pressure guideline of the European Societies of Hypertension and Cardiology (ESC/ESH) has defined the new threshold values (tab. 1) . However, attention should also be paid to the type of blood pressure measurement to be able to exclude white coat hypertension. Depending on the risk factors, hypertension is also divided into different stages (Tab. 2). Since the risk of cardiovascular disease increases with every increase in blood pressure, early and effective intervention is required. Just a 5 mmHg reduction in systolic blood pressure reduces the risk of cardiovascular events by 10%, stroke by 13%, and myocardial infarction by 14% [6].
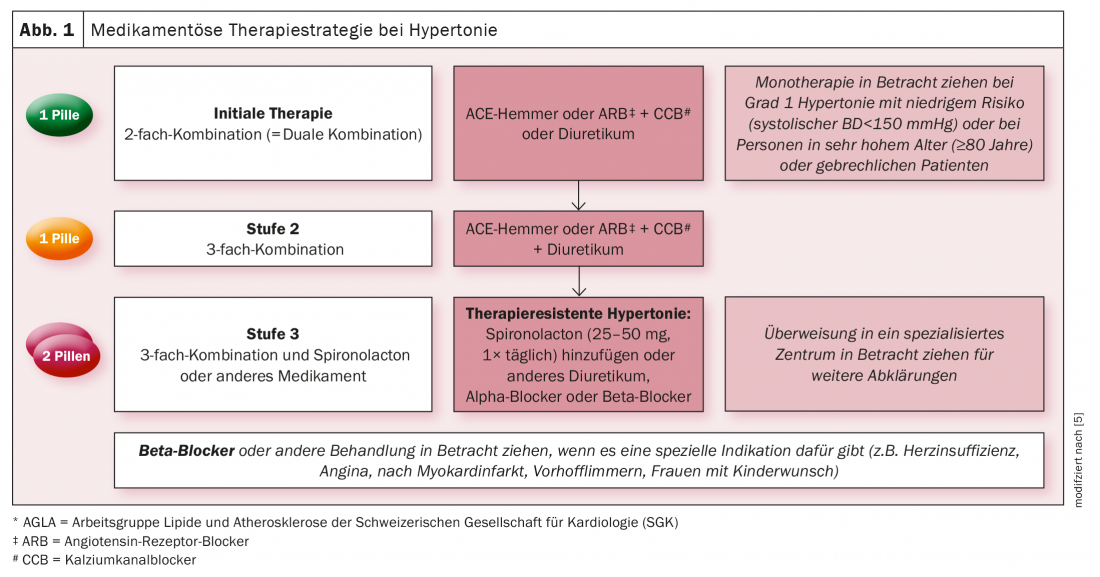
The guidelines therefore recommend starting therapy at values ≥140/90 mmHg. The primary goal is then a blood pressure <140/90 mmHg. In the long term, target values of 130/80 mmHg or lower should be aimed for. The basis should always be lifestyle changes such as stopping smoking, weight reduction and exercise. In addition, initial therapy is then given with a dual combination of ACEi or ARB in combination with CCB or a diuretic (Fig. 1). This should be administered as a fixed combination in one tablet. Likewise, escalation should be to a triple combination with a fixed combination, Rexhaj emphasized.
Uncontrolled hypertension in focus
However, despite the clear treatment algorithm, approximately 70% of affected individuals in Europe do not reach the target values [7]. The figures in Switzerland look similar: Of the 1.7 million hypertensive patients, only half are diagnosed and receiving treatment. Of these, however, only 40% are considered controlled. Conversely, 60% of hypertension patients in Switzerland are not controlled [8]. The reasons are mainly the lack of patient adherence, but also the limited use of combination therapies. However, monotherapy rarely achieves the goal. More than 75% of those affected require at least dual therapy. However, adherence decreases rapidly the more tablets have to be taken. Therefore, fixed combinations should always be used, the expert also affirmed.
Studies were able to demonstrate that patient adherence could be increased by approximately 44% by reducing the number of tablets with fixed combinations [9–12]. In addition, fixed combinations lower blood pressure faster and better than monotherapy [13]. Cardiovascular risk can also be reduced by 11%, Rexhaj reported.
Start early, reduce effectively
In summary, it has been shown that early initiation of treatment is indicated – even in elderly patients. To avoid falsely high values, blood pressure should ideally be measured outside the practice. Poor adherence must be considered the main reason for poor control. Therefore, fixed combinations should be used. These have been shown to lead to improved adherence, faster and better blood pressure control, a reduction in cardiovascular risk, and a reduction in side effects.
Congress: FomF Update Cardiology
Literature:
- www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (last accessed on 04.02.2022)
- Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903-1913.
- NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021; 398: 957-980.
- Vasan RS, Beiser A, Seshadri S et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA 2002; 287: 1003-1010.
- Williams B, Mancia G, Spiering W, et al: 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018; 36: 1953-2041.
- Blood Pressure Lowering Treatment Trialists Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 2021; 397: 1625-1636.
- Beaney T, Burrell LM, Castillo RR, et al: May Measurement Month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J 2019; 40: 2006-2017.
- Chow CK, Teo KK, Rangarajan S, et al: Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013; 310: 959-968.
- Castellano JM, Sanz G, Ortiz AF, et al: A polypill strategy to improve global secondary cardiovascular prevention: from concept to reality. J Am Coll Cadriol 2014; 64: 613-621.
- Selak V, Elley CR, Bullen C, et al: Effect of fixed dose combination treatment on adherence and risk factor control among patients at high risk of cardiovascular disease: randomised controlled trial in primary care. BMJ 2014; 348: g3318.
- Thom S, Poulter N, Field J, et al: Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD: the UMPIRE randomized clinical trial. JAMA 2013; 310: 918-929.
- Huffman MD: The Polypill: From Promise to Pragmatism. PLOS Med 2015; 12: e1001862.
- MacDonald TM, Williams B, Webb DJ, et al: Combination Therapy Is Superior to Sequential Monotherapy for the Initial Treatment of Hypertension: A Double-Blind Randomized Controlled Trial. J Am Heart Assoc 2017; 6:e006986.
CARDIOVASC 2022; 21(1): 26-27