A major factor in the development of atherosclerotic-related cardiovascular disease is the retention and accumulation of cholesterol-rich lipoproteins in the vessels. Therefore, in addition to adequate blood pressure control, the focus of effective prevention is primarily on LDL cholesterol lowering to reduce cardiovascular morbidity and mortality.
The most common cardiovascular diseases include chronic CHD and acute myocardial infarction, which are usually caused by coronary atherosclerosis. The risk of CHD is nearly 50% in healthy 40-year-old men and about 36% in women. In Switzerland, nearly 10 000 men were hospitalized due to acute myocardial infarction in 2018. In the meantime, acute treatment has improved significantly; however, many patients are still at increased risk of morbidity and mortality as a result. Therefore, the most important risk factors that can be influenced – hypertension and hypercholesterolemia – should be controlled at an early stage.
Fixed combination for fast blood pressure adjustment
Since it is known that treatment adherence decreases with each additional tablet taken, guidelines now recommend initial use of a two-drug fixed combination in hypertensive treatment when multiple antihypertensives are required. This allows target blood pressure to be reached more quickly in the more than two-thirds of patients for whom this is necessary.
Effective blood pressure reduction is of high prognostic value, as highlighted by a meta-analysis. Reduction of systolic blood pressure by 20 mmHg correlated with a twofold lower mortality rate. Lowering diastolic blood pressure by 10 mmHg is associated with a similar risk reduction. The primary therapeutic target should be <140/90 mmHg in all patients. Depending on age, risk and tolerability of the treatment, further reductions should be made thereafter on an individual basis.
If a hypertensive patient also has elevated LDL cholesterol, a fixed combination therapy is also recommended, this time of an antihypertensive with a lipid-lowering agent. Corresponding combination preparations are now available and can contribute to better vascular protection.
LDL cholesterol reduction in focus
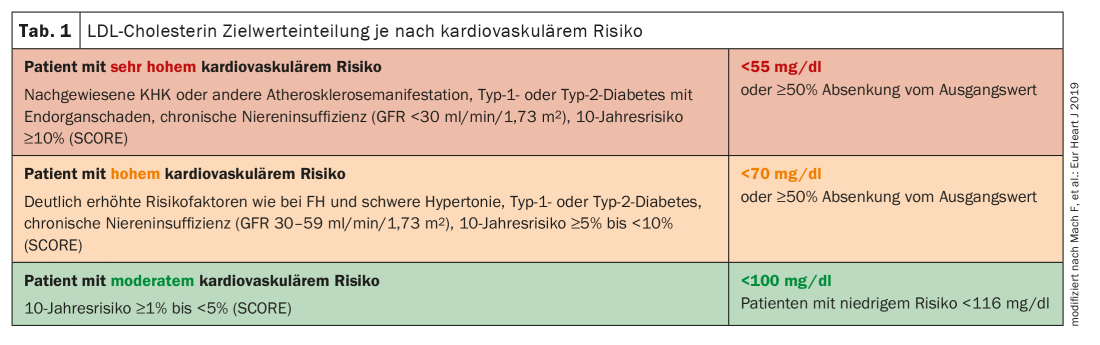
The first choice for reducing LDL cholesterol are statins, whose efficacy and safety have been demonstrated in numerous clinical trials. For example, a meta-analysis showed that for every 1 mmol/l (39 mg/dl) reduction in LDL cholesterol over one year, cardiovascular mortality was reduced by 20%, the rate of major cardiovascular events was reduced by 24%, and the rate of stroke was reduced by 16%. The LDL-C target values have been increasingly lowered in recent years and are based on the patients’ baseline cardiovascular risk (Fig. 1). However, the target values are only achieved in just under a quarter of those affected. This seems to have several causes. First, high-dose statin therapy is very rarely resorted to, and second, there is a non-linear dose-response relationship. Each doubling of the dose leads on average only to an additional reduction in LDL-C of about 6%. Therefore, care should be taken to choose a potent statin and, if in doubt, a switch should be made. This is because the side effects of statins are dose-dependent.
Combined treatment for significant LDL cholesterol reduction
If the LDL cholesterol target is not reached despite the highest statin dose that can still be tolerated, escalation to combination therapy should be made. The ESC guidelines recommend ezetimibe as the first combination partner, and PCSK9 inhibitors are available as another combination option. This can reduce LDL cholesterol by an additional 25%. This further, highly effective reduction is accompanied by a significant reduction in cardiovascular events. The goal of effective management in terms of blood pressure and cholesterol reduction is comprehensive vascular protection – ideally with just one tablet daily.
Further reading:
- www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/krankheiten/herz-kreislauf-erkrankungen.html (last call on 22.01.2021)
- www.obsan.admin.ch/de/indikatoren/myokardinfarkt (last call on 22.01.2021)
- Williams B, et al: Eur Heart J 2018; 39(33): 3021-3104.
- Lewington S, et al: Lancet 2002; 360(9349): 1903-1913.
- Cholesterol Treatment Trialists’ (CTT) Collaboration. Lancet 2010; 376: 1670-1681.
- Fox KM, et al: Clin Res Cardiol 2018; 107(5): 380-388.
- Knopp RH, et al: N Engl J Med 1999; 341(7): 498-511.
CARDIOVASC 2021; 20(1): 22











