The therapy of alcoholics is quite a difficult task. Psychosocial support measures are often initiated, which may not always be the only correct course given the advances in medication. Recently, it is new treatment goals such as reduction, rather than abstinence, from alcohol that have proven effective and stable over the longer term.
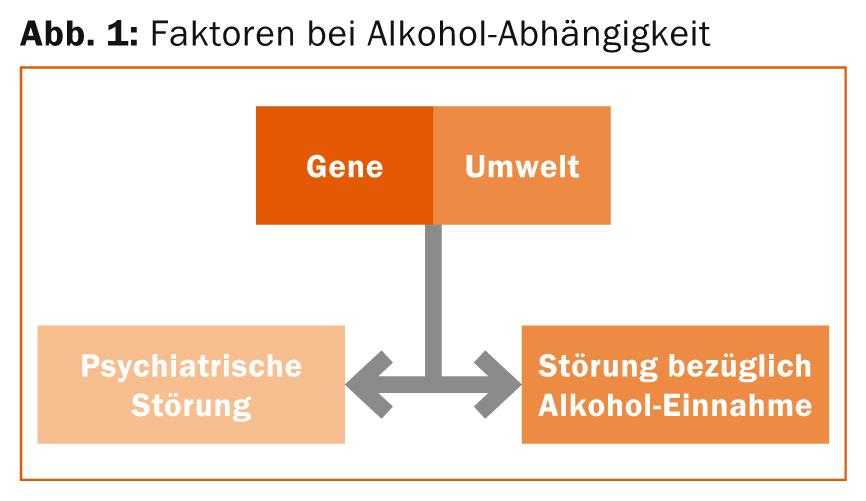
(ag) According to Prof. Henri-Jean Aubin, MD, Paris, psychiatric comorbidities and disorders are common in alcohol dependence. Such significant comorbidities are mainly mood and anxiety disorders. One can summarize the various factors involved in alcohol dependence in a graph, as shown in Figure 1 . It is critical to note that the arrows go both ways, so an alcoholic can be influenced by a psychiatric disorder, and vice versa. Alcohol dependence in women seems to be more often influenced by psychological comorbidity than in men, and anxiety disorders are often associated with alcohol dependence.
“New, as yet unpublished data from us show that in a small collective of alcohol abusers, some with alcohol-induced mood disorder and major depressive episodes, depression scores on the Hamilton scale already declined significantly after 8-15 days in withdrawal. It is crucial to note that the last antidepressant therapy was more than two weeks ago. So it seems that short-term changes in mood and anxiety are indeed possible when you stop alcohol,” Prof. Aubin explained.
Conversely, is the use of antidepressants useful in alcohol abusers with comorbid depression? A double-blind, placebo-controlled study from 2010 [1] concluded regarding the use of naltrexone, placebo, and sertraline individually and in combination in depressed alcohol-dependent patients that sertraline plus naltrexone resulted in a higher abstinence rate, later relapse, and fewer severe side effects compared to the other groups, and also prevented the depressive state at the end of treatment in many cases (83.3%).
In contrast, a previous meta-analysis or systematic review [2] summarized the current state of research to the effect that more studies on the use of antidepressants in alcohol dependence with comorbid depression are needed to draw a firm conclusion. In the case of alcoholics without comorbid depression, the use of antidepressants is not justified, according to the authors.
“The NICE guidelines are therefore as follows: they recommend that alcohol abusers with comorbid depression or anxiety disorder should first address the alcohol intake, because this may also significantly improve the depression or anxiety disorder. However, if these persist after three to four weeks of abstinence, the symptoms should be assessed and, if necessary, a referral or therapy for the specific disorder should be considered,” says Prof. Aubin. “In conclusion, although there is some evidence that antidepressants are effective in reducing depressive symptoms in depressed alcohol abusers, it is always more appropriate to treat the alcohol dependence first if there is comorbidity, as this may lead to improvement in the mood disorder as well.”
Clinical relevance of alcohol reduction
Prof. Jonathan Chick, MD, West Linton, addressed the question of how alcohol reduction, rather than complete abstinence, has clinical relevance. “The reason given for not providing treatment to individuals who should be receiving it is overwhelmingly an unwillingness to abstain from use,” Prof. Chick introduced. Thus, many sufferers prefer reduction rather than abstinence as a treatment goal [3,4]. There are also studies showing that non-abstinent remission was associated with better overall quality of life than abstinent remission after three years [5]. Mann et al. [6] investigated the question of what effects can be achieved with reduction as a therapeutic goal in more detail. In fact, nalmefene (opioid receptor modulator) was shown to reduce total alcohol consumption after six months compared to placebo (each taken as needed). In addition, the improvement in liver enzymes was greater than with placebo. Van den Brink et al. [7] measured the strongest effects precisely in the subgroup that had a confirmed high risk of drinking. In the combined six-month studies by Mann et al. [6], Gual et al. [8] and François et al. [9] also found that the Mental Component Summary (MCS) score was both significantly related to the reduction in alcohol consumption and greater with nalmefene (vs. placebo). That is, the mental component of quality of life was significantly improved with the drug after six months.
The most common side effects of the drug in each of the studies included nausea and dizziness, with the vast majority of side effects being mild to moderate, as well as transient and occurring after the first dose (not later).
“In summary, for some patients, the risk of harm starting from alcohol use can be reduced without having to stop use completely. The goal of reduction is preferred by many sufferers; it can be as effective as abstinence. It is quite possible here to keep the reduction stable over a long period of time [10]. Psychosocial support for the patient can also be incorporated into the therapy concept as an accompanying measure. Nalmefene (applied as needed) can be used to reduce heavy drinking days and total alcohol consumption. In terms of clinical relevance, the effect size of the compound was similar to that of therapies for other mental disorders,” concluded Prof. Chick.
Psychosocial accompanying measures
Psychosocial support measures were addressed by William D. Dundon, MD, Las Vegas: “In principle, this is one of the most common measures for alcohol addiction, forgetting that pharmacotherapy can complement this type of treatment very well. But, of course, it depends on compliance and the context in which the medication is taken. So you have to integrate psychosocial support into pharmacotherapy, for example in the form of an interview about the possible treatment goals, the benefits, but also the costs or disadvantages of the drug.”
In the course of the Phase III program on nalmefene, the so-called BRENDA was applied, according to Dundon. This is a brief, medication-focused, psychosocial interview that emphasizes, for example, the importance of adherence by using positive feedback. The measure guarantees that the support is constant and not too encircling. It can be learned by physicians with relatively little effort, according to Dundon, and produces good results.
Source: “Alcohol-Dependence – From Disease to Tretament,” Satellite Symposium at the 22nd European Congress of Psychiatry, March 1-4, 2014, Munich, Germany.
Literature:
- Pettinati HM, et al: Am J Psychiatry 2010 Jun; 167(6): 668-675. doi: 10.1176/appi.ajp.2009.08060852. epub 2010 Mar 15.
- Torrens M, et al: Drug Alcohol Depend 2005 Apr 4; 78(1): 1-22. epub 2004 Nov 11.
- Heather N, et al: Alcohol Alcohol 2010 Mar-Apr; 45(2): 128-135. doi: 10.1093/alcalc/agp096.
- Hodgins DC, et al: Addict Behav 1997 Mar-Apr; 22(2): 247-255.
- Dawson DA, et al: Alcohol Alcohol 2009 Jan-Feb; 44(1): 84-92. doi: 10.1093/alcalc/agn094. Epub 2008 Nov 28.
- Mann K, et al: Biol Psychiatry 2013 Apr 15; 73(8): 706-713. doi: 10.1016/j.biopsych.2012.10.020. Epub 2012 Dec 11.
- van den Brink W, et al: Alcohol Alcohol 2013 Sep-Oct; 48(5): 570-578. doi: 10.1093/alcalc/agt061. Epub 2013 Jul 19.
- Gual A, et al: Eur Neuropsychopharmacol 2013 Nov; 23(11): 1432-1442. doi: 10.1016/j.euroneuro.2013.02.006. Epub 2013 Apr 3.
- François, et al: Poster at ISPOR 2013.
- van den Brink W, et al: J Psychopharmacol 2014 Mar 26. [Epub ahead of print].
InFo NEUROLOGY & PSYCHIATRY 2014; 12(3): 39-41.











