Making medical care location-independent involves both opportunities and challenges in terms of implementation in the day-to-day running of clinics and practices. For this purpose, telemedicine offers a possibility to design diagnostics or therapy within the scope of technical application detached from place and time.
Making medical care location-independent involves both opportunities and challenges in terms of implementation in the day-to-day running of clinics and practices. For this purpose, telemedicine offers a possibility to design diagnostics or therapy within the scope of technical application detached from place and time.
The following overview mainly refers to the aspect of telemonitoring, the remote monitoring part of telemedicine. To this end, the first part of the paper first presents the prerequisites for a telemedicine program. In the second part, the workflows in the telemedical center (TMZ) are examined in more detail using the COPD disease as an example.
Goals of telemonitoring and care network
Telemonitoring is designed to support patients with a chronic condition. Especially in the accompaniment of the disease, the burden of disease can be reduced by targeted training as well as by improving self-management. This approach supports primary treatment. This requires a tightly integrated network of a telemedicine center and the respective primary care providers. The specific relationship between the TMZ and primary care provider must be agreed upon so that the division of roles is clear. The following questions may be relevant to this:
- Is telemedicine patient care provided exclusively by the TMZ or is there support from the primary care provider?
- Are critical cases escalated to the primary care provider?
- What data should be exchanged? For example, is there provision for regular reporting with key parameters, or can the primary care provider look at the electronic medical record when needed?
In general, no conclusive assessment can be made on the design of a telemedicine network because it depends on the available capacities. In individual critical cases, close coordination and exchange of information definitely make sense. This is the only way to ensure comprehensive care for patients with increased needs. A “care pilot” in the TMZ or a telemedical care management system can, of course, involve other professional groups and support the treatment of patients with primary responsibility. In addition, the type of telemonitoring and the extent of care management will be determined by the suspension of the TMZ and the care setting.
Requirements for a telemedicine program and the establishment of a telemedicine center.
In principle, the implementation of telemedicine approaches requires a sufficiently high-performance infrastructure for the transport of data (both in the company’s own network and via the Internet). In addition, standardized data exchange should be ensured from the outset in every process step so that the data can be recognized by all systems with as little effort as possible – provided they are networked units and there is no manual exchange process.
Telemedicine care and care management is provided through a common exchange platform that must contain all essential information. A more detailed description of a platform follows in the next section.
When setting up the platform, a decision must be made as to whether it is to be used on the company’s own systems (on-premise) or in the cloud. The decision has a significant impact on maintenance and support costs. In addition, different issues arise with regard to data protection and IT security. Notwithstanding this, IT expertise is required to operate a TMZ – depending on whether tasks such as providing the software and operating the platform are partially or fully outsourced to a technical service provider.
Access to the telemedicine platform is provided via application or also via web access. As a rule, mobile devices are used for this purpose by the patient. Many providers work with mobile devices or smart devices that are delivered locked (kiosk mode) and can only be used for the telemedicine program. However, modern telemedicine systems are increasingly trending toward bring-your-own-device. This development was triggered by the improved availability of mobile devices among patients. In addition, the connection to the telemedicine program can be made more quickly without time-consuming equipment shipping. This makes the program more cost-effective. Depending on the intensity of treatment and financial resources, mobile terminals and other measuring devices (such as pulse oximeter, scales, blood pressure monitor) can be provided. However, this requires a correspondingly well-established logistics process. Often, patients have necessary measuring devices such as a scale at home and then manually transmit the values to the telemedicine application. In principle, a coupling between app and measuring device and thus an automatic data transmission is possible.
In addition to the technical perspective, a number of other issues arise for the implementation of a telemedicine program. The processing of sensitive health data in particular places high demands on data protection and information security. In addition to the implementation of appropriate security concepts and the training of personnel, it is particularly important to provide participants in telemedicine programs with clear patient information and a comprehensive declaration of consent. If, for example, physicians are to participate in the program, a release from confidentiality obligations is also required. This legitimizes the exchange of information between TMZs and primary care providers.
Even though mobile devices are becoming increasingly widespread, it is still not a matter of course to assume that people are proficient in using apps and smart devices. The handling must be trained. In addition, care must be taken to ensure that the app is implemented in a way that is appropriate for the target group. The training effort, which should not be underestimated, is necessary to limit the use of the TMZ for problems and inquiries that arise. At the same time, the motivation of patients to participate in a telemedicine program increases.
Training of patients for the telemedical system, consultations, medical reporting of incoming vital signs and questionnaire results, contacting in case of deviating vital signs are carried out by medical staff at the TMZ. As a rule, these are nursing professionals. In addition, an interprofessional team orientation is useful. Administrative processes such as patient and practitioner recruitment (enrollment in the telemedicine program) can be considered separately.
Important characteristics for the specialist staff in the TMZ are, in addition to indication-specific or specialist knowledge, a professional, open-minded and empathetic way of conducting conversations (with a motivational approach), the ability to recognize problem situations in direct telephone contact in connection with the available data and to discuss them specifically with the patient with a view to improving the chronic illness. In order to be able to cope with the complex requirements, courses of study in e-health and digitization in medicine are becoming established for the further qualification of nursing staff.
Certainly, when viewed together, there are multiple challenges in building a TMZ. What is special in telemedicine is that any difficulties can only be solved remotely in direct telephone contact with patients. While location-based processes (in presence) offer the possibility to directly fix e.g. technical errors, remote support or management does not allow it. A high level of software and hardware reliability is therefore all the more important.
Description of the telemedicine platform
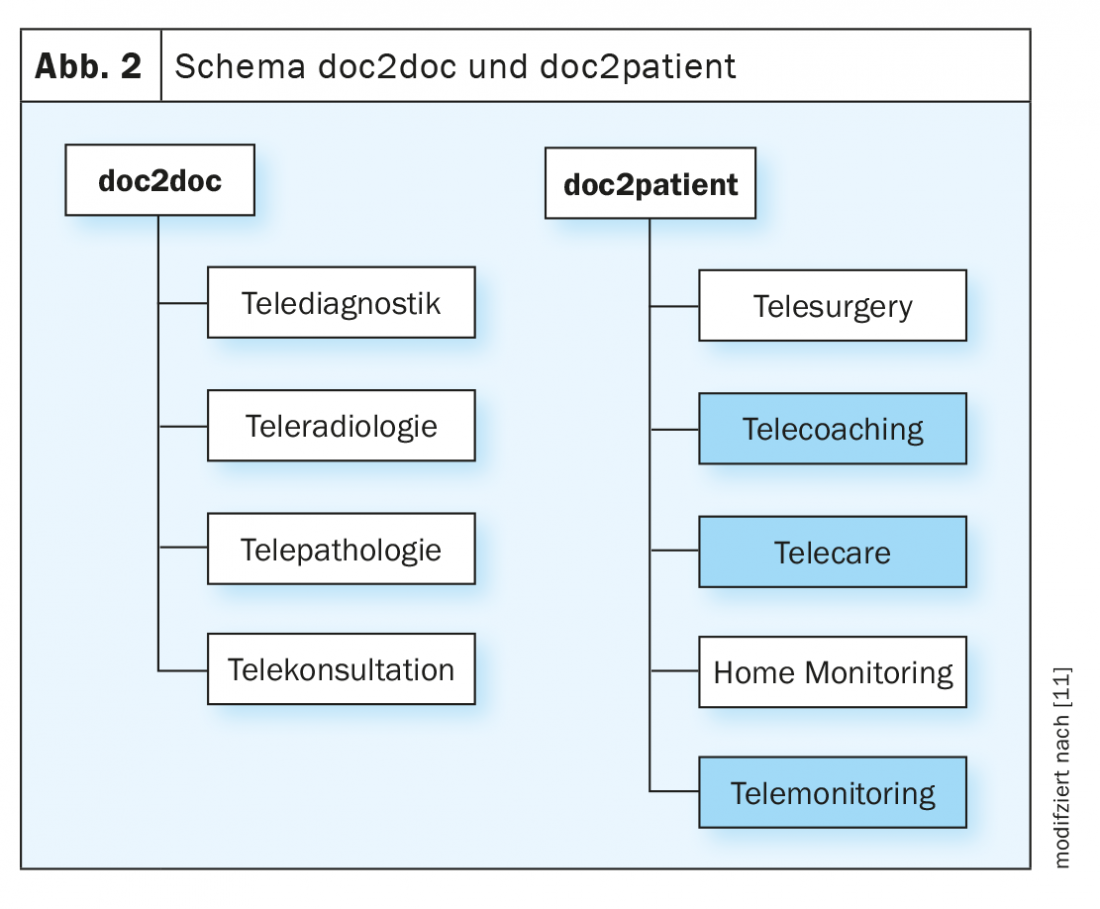
The typical components of a telemedicine platform are briefly described in general terms below (Fig. 1) . The exact division or location of the modules may vary. The platform applied specifically to the application for COPD is considered in the second part of the article. It should be noted at the outset that the platform should be a medical device according to the appropriate classification.
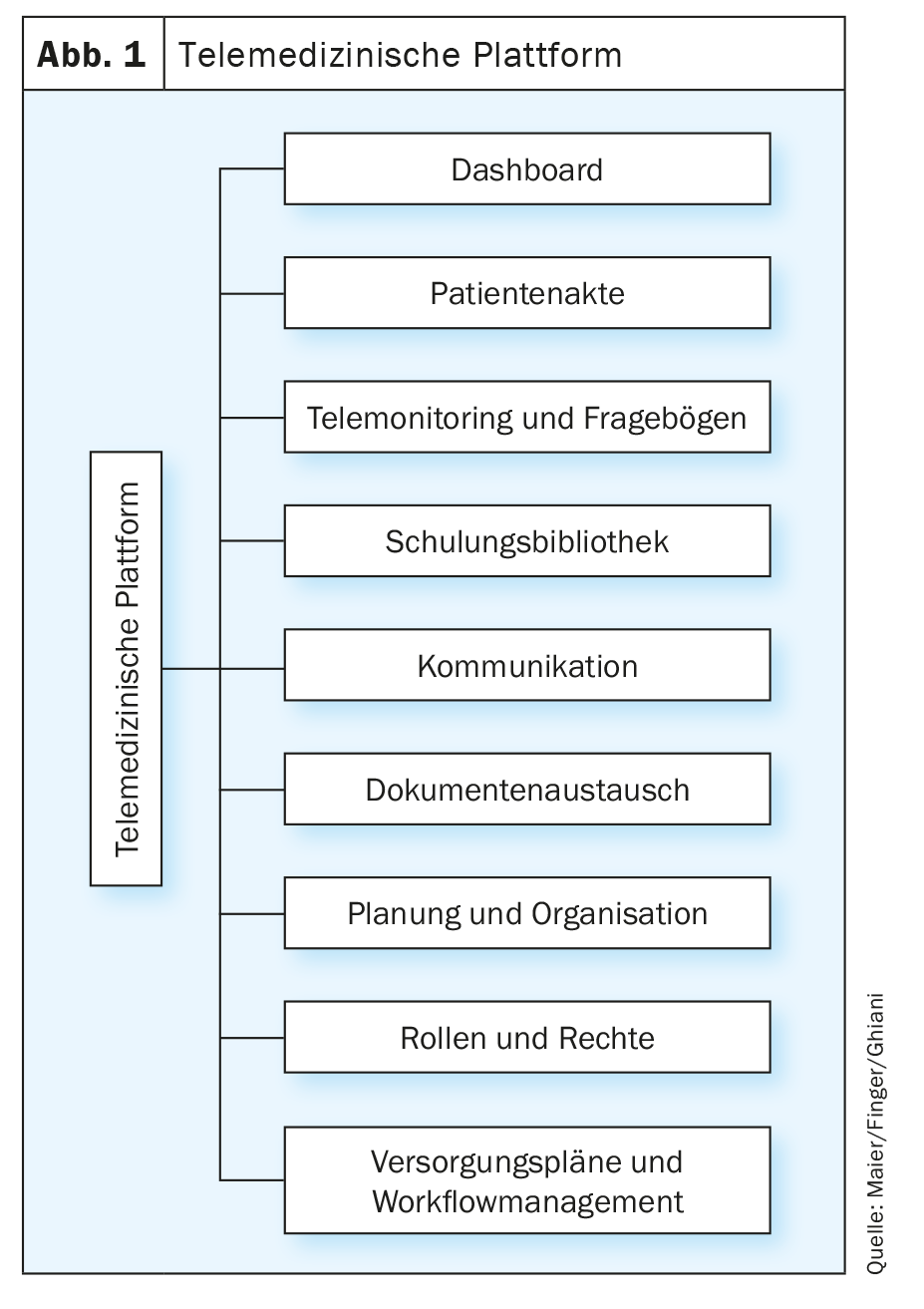
Dashboard
This is the summary representation of the patient population. At its core, a dashboard primarily serves the aspect of indicating the processing urgency for conspicuous vital signs and returns from the questionnaires according to different prioritization levels (e.g., low, medium, and high).
Patient file
The record presents essential patient information at a glance, such as master data, emergency contacts, diagnoses, co-morbidities and/or multimorbidities. Furthermore, the medication, laboratory values and progress documentation can be stored.
Telemonitoring and questionnaires
The module is used for real-time monitoring of vital signs and incoming questionnaires (e.g. from a symptom checker). For the vital parameters, limit values are stored, which trigger a corresponding alarm in case of deviation (e.g. a “flag” is generated, which must then be processed according to priority).
Training library
To support direct coaching, patients can access educational content within the platform in the form of videos and texts on understanding the disease and other topics to be integrated.
Communication
Patients can be contacted either classically by telephone or directly via the platform by chat and video call.
Document exchange
If no regular data exchange is planned, it should be possible to upload or download findings and other documents.
Planning and organization
An integrated calendar function is useful for organizing or keeping track of appointments (e.g. for an upcoming video consultation). In addition, a journal or diary can support patient “documentation.” Important events or individual goals in coping with the disease can be recorded there.
Role and rights
Central to building a platform is access and access control via a comprehensive roles and rights concept. This determines for patients and caregivers as well as for participating primary caregivers which modules can be viewed with which view/perspective. The fact that the concept defines data access is very significant for data protection.
Supply plans and workflow management
While roles and rights focus more on platform-administrative processes, supply plans and workflow management focus on the operational use of the platform. Indication-specific care plans define the times when caregiver activities are required, training modules are unlocked for patients, or certain regular or one-time questionnaires are provided to patients. The platform should be as simple and effortless to use as possible, so that the workflow for processing does not require lengthy steps. If necessary, defined escalation models can be used to assign responsibility to the other experts.
Telemedicine at the Robert Bosch Hospital
The Department of Telemedicine has been established at the Robert Bosch Hospital in Stuttgart since 2007. The telemedical work concentrates on the doc2patient and nurse2patient areas (Fig. 2) . The focus is on nursing telecoaching, telecare and telemonitoring. As an example, the telemedical care of COPD patients will be discussed in the course, which sees itself as a complementary accompaniment to the guideline-based therapy of the treatment providers.
Prevalence of COPD
Worldwide, chronic obstructive pulmonary disease (COPD) is one of the most common diseases [1]. Estimated to be 10.3% in 2019 between 30-79 years of age [2]. Across Europe, it is the third leading cause of death.
Together, WHO and the National Heart Lung and Blood Institute (NHLBI) launched the Global Initiative for Obstructive Lung Disease (GOLD) in 1997. It aims to accurately measure global COPD prevalence and associated morbidity, mortality, limitations in disease-related quality of life, and associated medical costs through a uniform disease definition and epidemiological methodology.
The spirometry-based definition of COPD in the GOLD guideline, first published in 2001, allowed an objective assessment of prevalence figures in subsequent epidemiological studies (e.g., PLATINO study 2005, BOLD study 2007), which turned out to be higher due to the methodology than diagnosis based on clinical symptoms alone [3].
Epidemiological studies suggest that the number of COPD sufferers in Germany alone will increase to approximately 8 million by 2050, due to increasing life expectancy and an aging population [4].
Telemedicine: Evidence in COPD
Due to the COPD-associated burden of disease, patients use outpatient and inpatient healthcare elements more frequently. The telemedicine approach, on the other hand, allows for close, in-home support. As a rule, it cannot be realized in such intensity even by outpatient general practitioner and specialist care, since control appointments in presence are less frequent. Any acute worsening of the chronic disease (exacerbations) are thus diagnosed later and then result more frequently in inpatient emergency admissions. In addition, patients do not always have comprehensive knowledge about the disease, so self-management in these situations is usually inadequate.
To demonstrate potential effects of telemedicine monitoring on direct medical costs, health system resource use, and mortality rates in patients with COPD, Achelrod et al. analyzed the effects of telemedicine monitoring on direct medical costs, health system resource use, and mortality rates in patients with COPD. Data from participants in Germany’s largest telemonitoring pilot project to date. They concluded that telemonitoring is a viable and cost-effective strategy to positively impact the above factors after 12 months. Thus, contrary to widespread fears, the reduction in outpatient medical presentations does not appear to have a detrimental effect on disease progression [5].
Also, the results of a three-year case-control study evaluating telemonitoring and its effects on health-related outcomes in patients with COPD primarily showed no relevant cost differences [6]. Nevertheless, a significantly higher number of outpatient physician contacts and drug prescriptions were found under telemonitoring. However, analyses of patient subgroups stratified by COPD severity revealed that total medical costs were heterogeneously distributed within each GOLD stage. They tended to be lower for patients in GOLD stage 1/2, whereas they were significantly higher in GOLD stage 3/4 compared with the control group without telemonitoring. Also striking was a significant survival benefit with telemonitoring in the subgroup of patients with stage GOLD 1/2 COPD.
Overall, the integration of telemedicine applications in therapy can enable continuous and valuable patient care in terms of patient empowerment and participation in therapy [7].
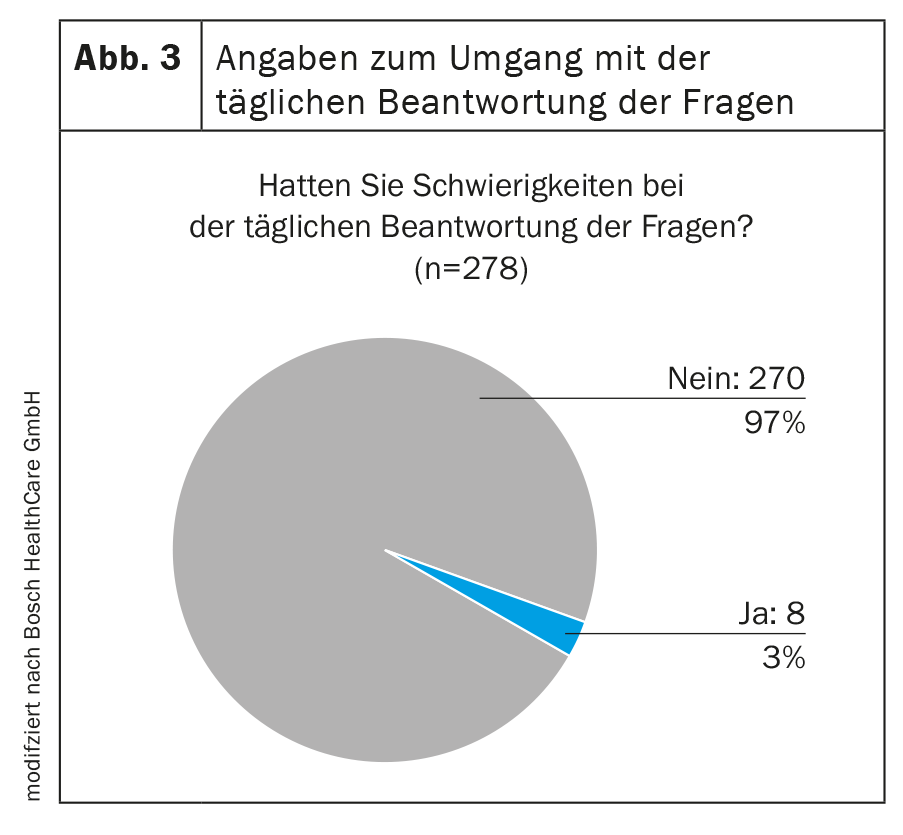
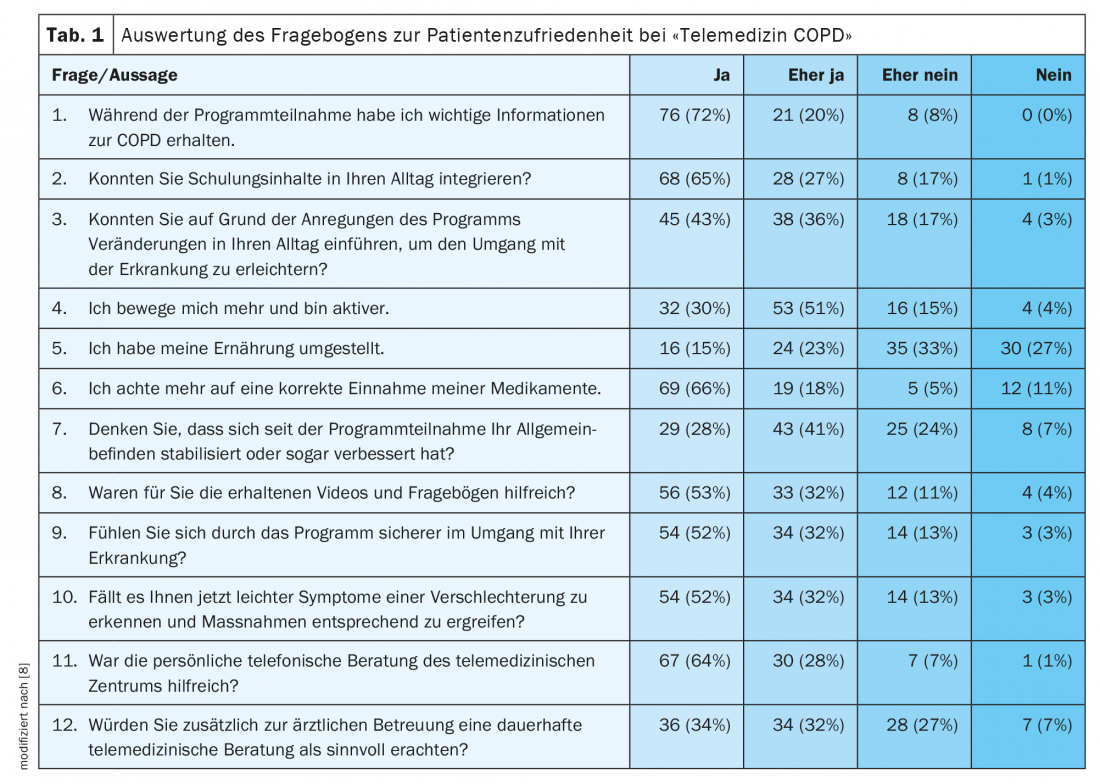
To know which factors are relevant to patients when receiving telemedicine care, survey data were analyzed at the Telemedicine Center at Robert Bosch Hospital over the period 2012-2017 [8]. An analysis of 278 participants (TN) was conducted over the period 2012-2014 to assess the personal benefits of the telemedicine program. The participants were asked about their satisfaction with the program content and the handling of the equipment used (Fig. 3, Fig. 4). In 2017, a qualitative survey of 105 participants was conducted using questionnaires on various aspects of patient satisfaction (tab. 1) .

As a result, it can be summarized that the patients largely reported greater confidence in managing the disease as a result of participating in the program. Furthermore, an improvement in everyday life was described due to more knowledge and the strengthened self-management. The training content and videos provided via the tablet have contributed to this. Supplementary telephone support is seen as a central building block to further deepen knowledge.
Workflows in the telemedicine center
Patients are selected for participation in a telemedicine program according to established criteria. In addition to the disease-specific diagnoses and the assessment of whether there has been a deterioration (e.g., due to a past hospitalization) or could be in the future, the motivation to participate in such a program is considered. Especially the frequent input of vital signs and answering of questionnaires may result in insufficient participation or early termination.
In the specific case, patients are approached by the health insurance company. The presented system also relies on a pulse oximeter with tablet. As outlined above, physician colleagues may be involved for supervision while participating in the program. They provide essential treatment information and enroll patients in the program. Likewise, they receive special progress reporting as needed during program participation.
During the defined program period of 10 months, the selected patients can record vital parameters such as blood oxygen concentration and heart rate, both of which are measured by pulse oximetry, as well as weight and optionally blood pressure data once a week.
Also on a daily basis, participants answer questions about COPD-related symptoms such as.
- Presence of dyspnea, its intensity and distribution over the day-night rhythm.
- Physical resilience
- Presence of cough
- Presence of bronchial secretions with extent/if any. color changes
- Presence of thoracic tightness
- Presence of breath sounds
This patient-collected data is entered through the tablet located in the home and transmitted in real time to the telemedicine center. As part of telecoaching, patients can access information on COPD-related topics on their tablet.
In addition, the participants have the possibility to contact the professional staff by phone within the defined office hours 5 days a week. Because it is not a telemedicine emergency program, the TMZ is not available 24/7.
In the following, the working principle of the reporting of recorded data will be further discussed.
The underlying (web) application consists of a health program for patients and an intake and clinical application for telemedicine staff. The system presented is Philips Motiva. This solution has already been on the market for some years and, despite design weaknesses, has extensive application potential. However, the software will no longer be available in the course of 2022. Nevertheless, the basic logic of a telemedicine platform can be easily recognized.
Via the admission application, the TN are first created in the electronic medical record. The clinical application can be used to analyze the vital signs and results of the various questionnaires sent by the TNs, as well as to provide educational materials in text form or training videos. Among other things, videos are provided on dietary behavior, goal setting in everyday life, inhalation techniques, dealing with emergencies, mobility and sports, and taking medications. This is done through the various settings of the application as well as through the predefined and stored workflow.
 .
.
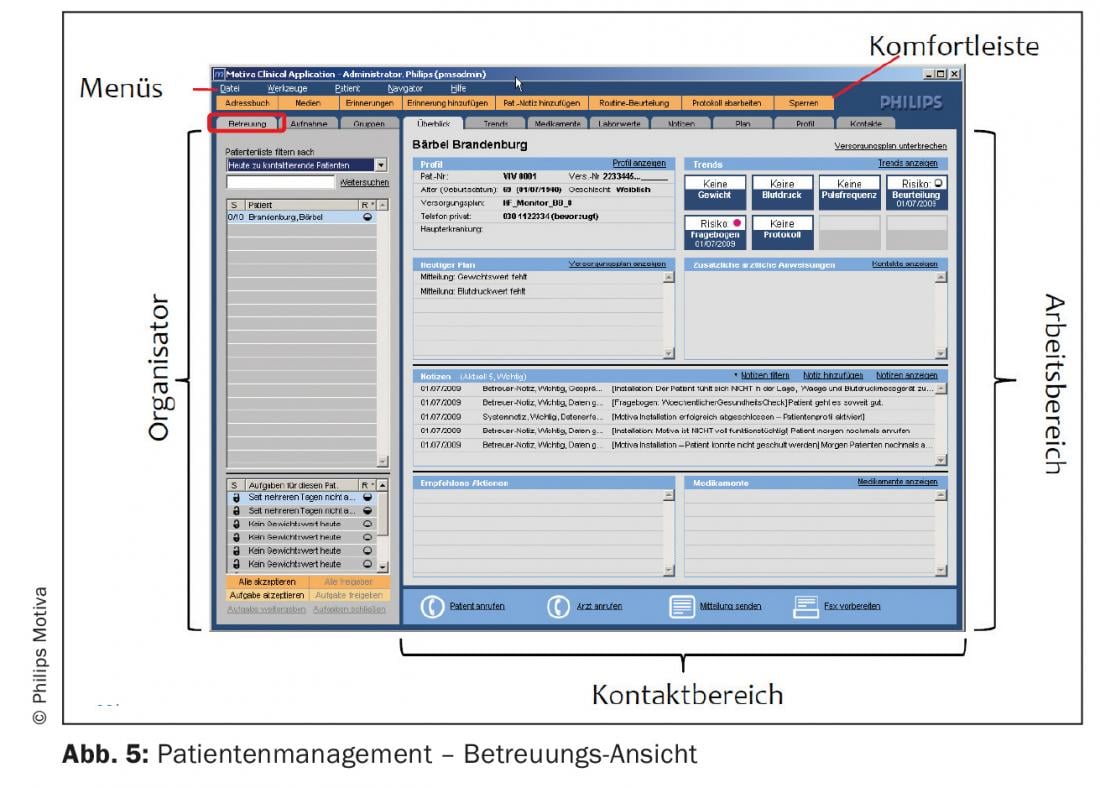
After logging into the telemedicine platform, the patient filter and search function, as well as the patient list with risk status and task list, are displayed to the TMZ-MA in the care view (Fig. 5) in the “Overview” tab. Hereby tasks generated at the respective patient due to:
- an intervention rule (e.g. change of a vital parameter compared to the baseline value).
- lack of data transmission
- of a completed questionnaire (e.g. change of symptoms)
- of a memory
be recorded. The “Trends” tab contains the measured vital signs, the assessment results of the sent questionnaires and visualizes graphical and tabular trends (Fig. 6).
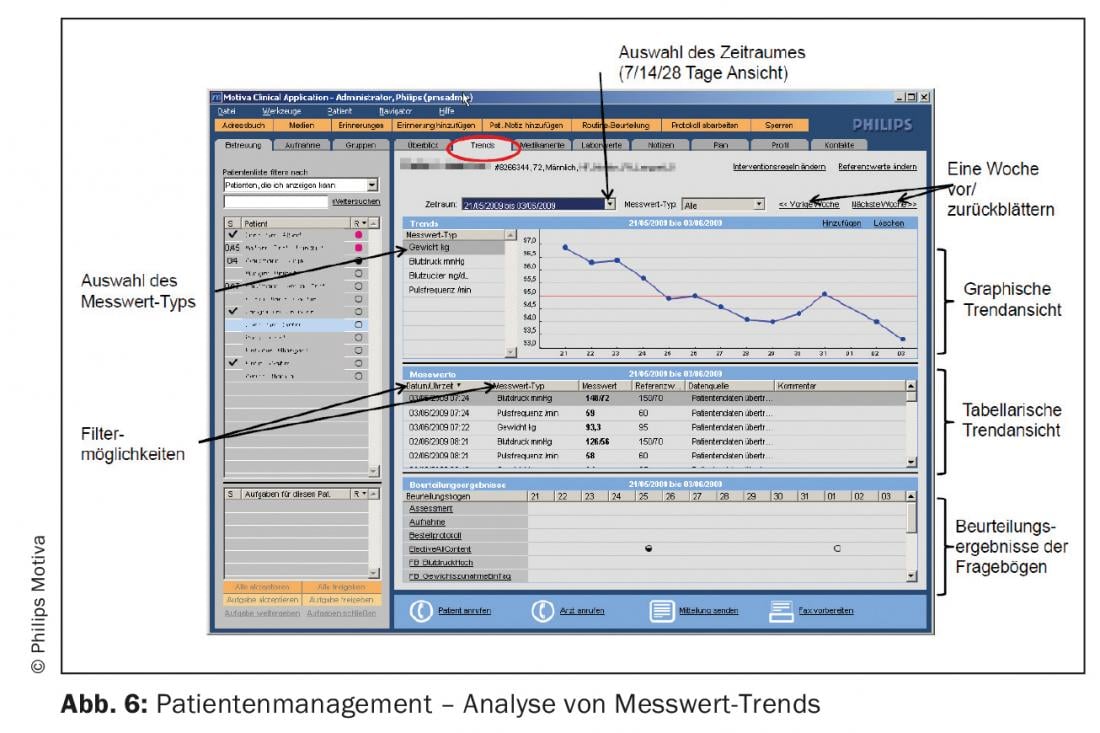
In summary, the tasks generated in the system at the above triggers are processed and completed by the TMZ MAs. The contents of consultations and conversations regarding patients, their relatives/contact persons, treatment providers if applicable, are documented as clinical notes and are accessible to all TMZ MAs with access rights.
The medical application also offers the possibility of assigning a defined group of patients to a TMZ-MA for care and also the possibility of finding the generated tasks without special assignment. High risk tasks are prioritized by the TMZ MAs.
In case of changes in both measured parameters and symptoms, a timely telephone contact is made by trained professionals with clinical experience as well as social and communication skills to evaluate the actual condition of the respective patients [9]. It is the responsibility of the TMZ-MA to provide individual advice on further procedures, such as accompanying measures and behavioral interventions, depending on the change. Patients turn to their (primary) care providers for escalation of treatment management.
Chronic diseases, which are characterized by a particular progression dynamic and which are characterized by co-morbidity and/or multimorbidity in the advanced stage of the disease, require numerous disease-related adaptation and coping strategies. The self-management that strengthens this is described by Lorig as learning and practicing skills necessary to continue living an active and emotionally satisfying life in the face of chronic illness [10].
It is advisable to structure the contents of the consultation within the framework of patient education also with regard to preparation for the discussion, clarification of the situation, problem analysis with development of solution strategies. As the analysis by the Robert Bosch Hospital also shows, it makes a lot of sense to sprinkle in recurring recommendations for patients with chronic illnesses. In addition to providing disease-specific guidance on medical issues such as medication or respiratory therapy, the goal in coaching is to break the spiral of deterioration. The program can be particularly successful for new diagnoses if there is a high level of willingness or motivation among patients to participate and collaboration with primary care providers.
Summary
When participating in a telemonitoring program, chronically ill patients with COPD can benefit from close monitoring. For this, a platform with device connection must be available and processes in the TMZ as well as responsibilities with external treatment providers must be clearly defined. Apart from the technical component, the core of telemedicine care is the personal or telephone contact between patients and caregivers. With targeted coaching, lifestyle adjustment can be achieved in patients and self-management can be strengthened. This improves the way the disease is dealt with in the long term.
Take-Home Messages
- The effort required to establish a program is estimated to be high (e.g., supply plans, building the platform).
- The success of the telemedicine program depends heavily on individual needs.
- The involvement of primary caregivers is very valuable, meaning and purpose must be clearly defined in advance.
- Follow-up of selected patients is very useful and leads to improvement of disease burden and self-management.
Literature:
- Aumann I, Prenzler A: Epidemiology and costs of COPD in Germany – A literature review on prevalence, incidence and costs of disease. The Clinician 2013; 42(4): 168-172; doi: 10.1055/s-0033-1347040.
- Adeloye D, Song P, Zhu Y, et al: Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med 2022; 10: 447-458.
- Karpinski NA, Petermann F: COPD: burden, risk factors, and prevalence. Health Care 2009; 71(12): 816-822; doi: 10.1055/s-0029-1231048.
- Peters E, Pritzkuleit R, Beske F, et al: Demographic change and incidence of disease. Bundesgesundheitsbl 2010; 53: 417-426; doi: 10.1007/s00103-010-1050-y.
- Achelrod D, Schreyögg J, Stargardt T: Health-economic evaluation of home telemonitoring for COPD in Germany: evidence from a large population-based cohort. Eur J Health Econ 2017; 18: 869-882; doi: 10.1007/s10198-016-0834-x.
- Hofer F, Schreyögg J, Stargardt T: Effectiveness of a home telemonitoring program for patients with chronic obstructive pulmonary disease in Germany: Evidence from the first three years. PLoS ONE 2022; 17 (5): e0267952; doi: 10.1371/journal.pone.0267952.
- Woehrle H, Schöbel C: The future of pneumology is digital. Pneumo News 2021; 01; doi: 10.1007/s15033-021-2676-1.
- Analysis of patient satisfaction of telemedical care within the project A.T.e.m./Telemedicine COPD at Robert-Bosch-Krankenhaus.
- Braga AV: The telemedicine consultation. Digital Transformation of Services In Healthcare I 2016; 93-108; doi: 10.1007/978-3-658-12258-4_6.
- Lorig K: Patient education: A practical approach, third edn. London: Sage Publications 2001.
- Pelleter J: Fundamentals of telemedicine. In: Schultz C, Helms T. (Eds.): Telemedicine – Paths to Success. Stuttgart: Kohlhammer 2013.
InFo PNEUMOLOGY & ALLERGOLOGY 2022; 4(3): 14-20.