Benign prostatic syndrome (BPS) is one of the most common reasons for physician consultation in older men. During diagnosis, the severity of symptoms and the patient’s level of distress should be clarified so that therapy can be planned accordingly. A large prostate alone is not a reason for treatment. Primarily, alpha-1 receptor blockers and 5α-reductase inhibitors are available for drug therapy. When prescribing, it is important to consider the therapeutic goal (symptom reduction or slowing of progression) and the potential side effects. The gold standard for surgical procedures is still transurethral electroresection (TURP).
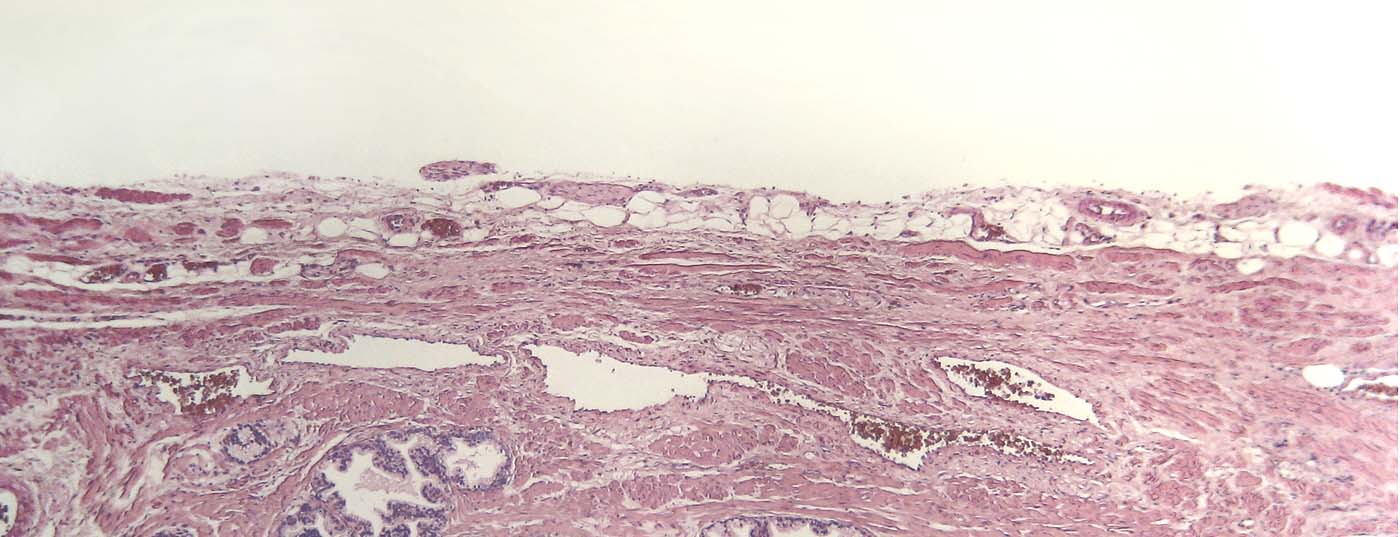
Benign prostatic hyperplasia (BPH) is a histological change and refers to a benign enlargement of the prostate due to an increase in cells in the area known as the transition zone. The symptoms caused by this enlargement are referred to in English as LUTS (“lower urinary tract symtoms”), and these in turn can be divided into storage and voiding disorders. In German-speaking countries, the term benign prostatic syndrome (BPS) is used, which is associated with irritative and/or obstructive micturition symptoms (Table 1).

BPH is one of the most common reasons men consult their primary care physician or urologist as they age. Due to the diversity of complaints as well as the severity, the assessment is not always easy. Since, on the other hand, referral to a urologist is not always mandatory, we would like to provide the necessary basic knowledge for primary assessment and, if necessary, initiation of therapy.
Epidemiology and definition of BPH
Prostate hyperplasia is a histological change that can be detected as early as 30 years of age. Almost 90% of all men from the eighth and ninth decade of life are affected. However, not every man with BPH has clinical symptoms, and few eventually need surgical intervention. BPH is often mistakenly used as a synonym for male lower urinary tract symptoms.
Medical history and physical examination
Diagnostics should answer the following questions:
- Can the patient’s complaints be attributed to BPH at all?
- Are the complaints so severe that they need to be treated?
- What is the appropriate form of therapy?
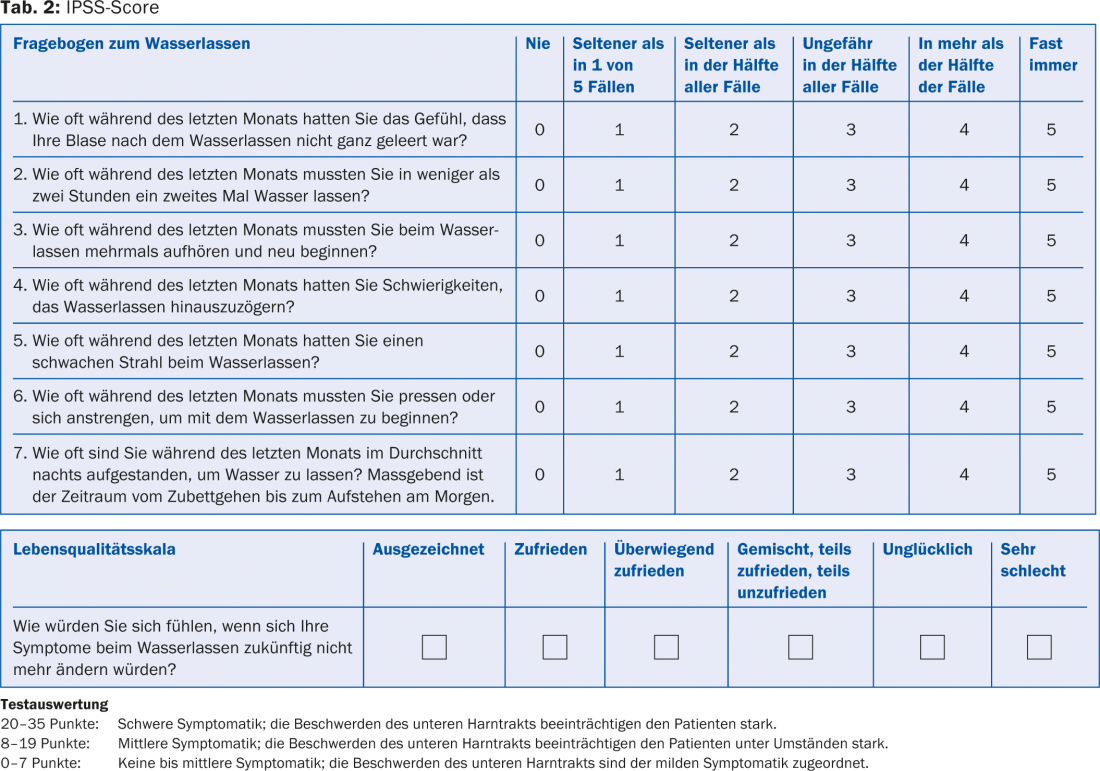
A thorough medical history is essential. International questionnaires such as the IPSS (International Prostate Symptoms Score) may be useful. It contains eight questions, seven on symptoms and one on quality of life (Table 2). The history should also include questions about hematuria, previous surgery, accidents, neurogenic diseases (e.g., Parkinson’s disease, multiple sclerosis), previous drug therapies, infections, and diabetes mellitus.
On examination of the abdomen, renal lobe tapping dolence is tested; suprasymphyseal palpation of a bulging bladder or abdominal mass may be possible. Inspection and palpation of the external genitalia is performed to detect any meatus stenosis, phimosis, or palpable urethral mass. The digital rectal examination is used to detect a rectal or prostatic malignant change and is performed in the lateral position. The method of four-footed stand is obsolete. The size, shape, consistency and dolence of the prostate, mucosal shift and any indurations are assessed. An enlarged prostate in itself is not a reason for treatment.
Laboratory and imaging
Urinalysis using urine sticks is performed to obtain a rough orientation regarding a possible infection or diabetes mellitus as the cause of the symptoms. In case of abnormalities, a urine sediment and possibly also a urine culture should be taken. Further, the prostate specific antigen (PSA) should be measured. It is a kallikrein-specific protease that is organ-specific but not disease-specific. Therefore, an increase in PSA should not be considered primarily malignant, but may also occur as part of a BPH or inflammatory event. The further procedure must be decided individually with each patient. This article will not discuss this further.
Imaging by sonography is also extremely helpful in the initial examination, but is not mandatory. Residual urine above 100 ml is considered a sign of incipient detrusor decompensation and may be the cause of additional complications of BPD. Further, sonographic evaluation of the kidneys is performed to rule out hydronephrosis as a late complication of BPH. Uroflowmetry is a simple and non-invasive method for objectifying maximum urine flow and micturition volume. The urine volume should be above 150 ml, otherwise the examination cannot be assessed conclusively. To assess subvesical obstruction, the maximum flow rate is the best parameter. A maximum flow rate below 12 ml/s is primarily considered subvesical obstruction, most often due to prostatogenic obstruction.
Therapy principles
Various options are available for the treatment of BPD, which differ in their efficacy and also in their invasiveness and thus tolerability. In most cases, the most effective forms of treatment are also the most invasive. Each patient must be discussed individually to find a therapy that offers the best risk-benefit ratio relative to his or her situation. If the discomfort is minor, a wait-and-see procedure may be chosen. As a rule, drug therapy is primarily initiated before a surgical procedure is chosen. Often, with drug treatment, surgical therapy can be postponed for a long time.
Drug therapy
Phytotherapy: According to international guidelines, published data are insufficient to allow official recommendations regarding the dispensing of phytotherapeutic preparations.
Alpha-1 receptor blockers: Alpha blockers are the drug group of choice for treating BPD. They act on the alphaadrenergic receptors in the urogenital tract, which are mainly located in the bladder neck, prostate smooth muscle, and urethra. Blocking the receptors does not reduce resistance in the prostate area, but it does significantly reduce symptoms. Possible side effects include fatigue, dizziness, headache, diarrhea, swelling of the nasal mucosa, flu-like symptoms, retrograde ejaculation, and hypotonic dysregulation. All side effects are reversible in principle after discontinuation of the drug. The effects on blood pressure are more pronounced in hypertensives than in normotensives.
There are several alpha blockers on the market. They can be distinguished both by selectivity for subtypes of alpha-1-adrenoceptors and by their pharmacokinetic properties. These differences have an impact on tolerability and route of administration. The latest products, which act on the alpha-1a receptors most abundant in the prostate, result in fewer orthostatic side effects. In patients with planned cataract surgery, therapy with the alpha blocker tamsulosin should be paused without fail, as intraoperative “floppy iris syndrome” may occur.
5α-Reductase Inhibitors: Currently, the 5α-reductase inhibitors dutasteride and finasteride are available. They differ in the selectivity of the isoenzymes. These inhibit the conversion of testosterone to the active metabolite dihydrotestosterone in the prostate, resulting in volume reduction. This aims to reduce the progression of prostate enlargement, but the symptoms are less affected. Patients with a large prostate volume benefit more from this therapy, but the effect develops only over months. The side effect profile includes impotence, decrease in libido, ejaculation disorders, and gynecomastia. Taking 5α-reductase inhibitors reduces PSA levels, which complicates the interpretation of this value in relation to prostate cancer screening. Studies have shown that prostate carcinomas newly diagnosed on therapy with 5α-reductase inhibitors have an increased proportion of undifferentiated carcinomas with a Gleason of 7-10. 5α-Reductase inhibitors can also be used to reduce BPH-associated hematuria. Finasteride is the main focus here.
Combination therapy: Combination therapy with an alpha blocker and 5α-reductase inhibitor is not indicated for symptom reduction alone. In the case of a large prostate, combination treatment is appropriate for inhibiting progression of BPH and is superior to monotherapy.
Anticholinergic therapy: Often irritative symptoms are the main focus in BPH, so that therapy with anticholinergics may be indicated. Because urinary retention can develop with the use of these medications, sonographic residual urine checks are recommended. The indication for these drugs must always be well considered.
Surgical therapy
The gold standard of surgical therapy is still TURP (transurethral electroresection) of the prostate. The indication is moderate to severe symptoms that are insufficiently reduced by an attempt at drug therapy. The procedure is mainly suitable for the treatment of obstructive complaints, but the irritative complaints can be indirectly influenced and improve postoperatively. For TURP to be performed, the volume of the prostate should not exceed 80 ml. The procedure is performed under general or partial anesthesia. There is no need to stop taking acetylsalicylic acid before TURP.
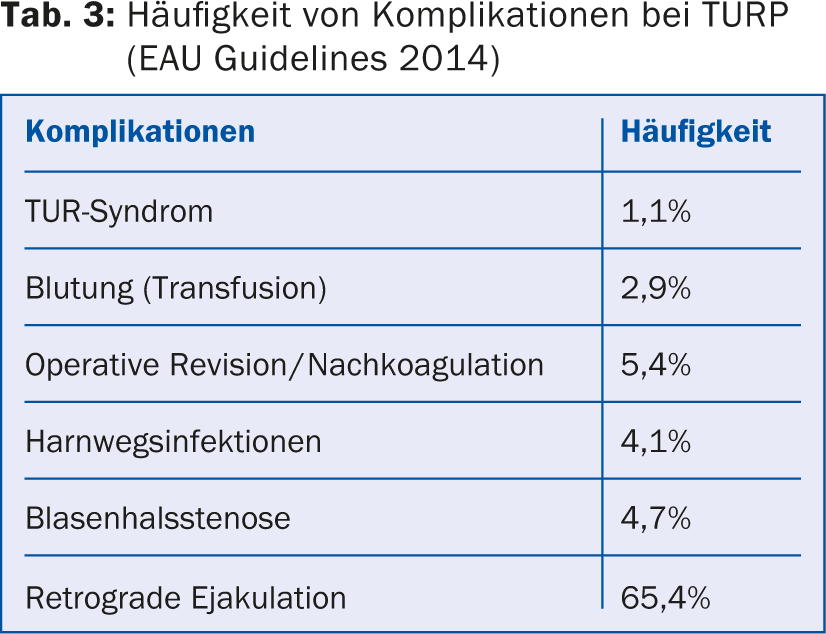
Intraoperatively, a number of complications may occur, but overall they are rather rare (Tab. 3) . The postoperative phase is characterized, especially in patients with long-standing complaints, by irritative complaints such as rapid urination, burning at the tip of the penis, etc., which can be explained by the internal wound. These complaints subside over the coming weeks to months. About 10-14 days postoperatively, a check of the urine by means of urine culture should be performed by the general practitioner. If significant bacteriuria is seen >105/ml, it should be treated with antibiotics according to resistance.
Permanent catheter therapy/cystofix
In certain cases, when drug therapy fails and surgical risk is too high or surgery is not desired by the patient, therapy with indwelling catheters or placement of a suprapubic catheter is indicated. Catheters should be changed at regular intervals of 6-8 weeks.
CONCLUSION FOR PRACTICE
- Anamnesis and assessment of suffering are essential components in the diagnosis of benign prostatic syndrome.
- Drug treatment with alpha-blockers and/or 5α-reductase inhibitors primarily allows sufficient symptom relief in many patients and is thus a reasonable alternative to surgery in these cases, at least in the short and medium term.
- Anticholinergic therapy may be attempted in BPH after established alpha blockade and persistent irritation and lack of residual urine.
- Postoperative irritative discomfort is most often triggered by healing of the resection cavity rather than by infection.
Literature:
- McVary K: BPH: Epidemiology and Comorbidities. Am J Manag Care 2006; 12(5): Suppl: S122.
- Guidelines of the German Society of Urology (DGU) and the Professional Association of German Urologists (BDU), S2-Leitlinie Urologie: Diagnostik und Differentialdiagnostik des Benignen Prostata-Syndroms (BPS).
- Kortmann BBM, et al: Urodynamic effects of alpha-adrenoceptor blockers: a review of clinical trials. Urology 2003; 62(1): 1-9.
- Gravas S (chair), et al: Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO), © European Association of Urology 2014.
- Campell-Walsh: Urology. 10th Edition.
- Chang D, Campbell J: Intraoperative floppy iris syndrome associated with tamsulosin. J Cataract Refract Surg 2005; 31(4): 664-673.
HAUSARZT PRAXIS 2014; 9(10): 10-14