Cardiovascular disease is one of the most important causes of perioperative morbidity and mortality. The goal of preoperative assessment and optimization is to reduce the incidence of perioperative cardiac complications and thus improve the short/long-term prognosis. The clarification strategy is based on physical performance, risk of the procedure, and clinical risk indicators. Patients with preserved exercise capacity (≥4 MET, MET = metabolic equivalents) and/or lack of clinical risk indicators usually do not need further cardiac evaluation before noncardiac surgery. Patients with impaired exercise capacity (<4 MET) and clinical risk indicators are further evaluated prior to major surgery. The recognized cardiological-internal indications apply to diagnostics and therapy. While very many medications are now passed on perioperatively unchanged, coagulation-modulating therapy often requires adjustment.
Preoperative evaluation is of great importance prior to (elective) surgical interventions. The focus is on identifying and – where possible – optimizing somatic concomitant diseases. Prior to major interventions and/or in polymorbid patients, clarification of the resuscitation status and the patient’s will regarding invasive forms of therapy such as prolonged stay in an intensive care unit, mechanical ventilation, renal replacement procedures and mechanical circulatory support (“advance care planning”) is no less important.
Because cardiovascular diseases are among the most frequent causes of perioperative morbidity and mortality and also have a significant influence on the long-term outcome of patients, cardiological assessment is of central importance in the context of preoperative evaluation. The overall goal of preoperative cardiac evaluations is to detect and – where possible – optimize previously unknown or underestimated cardiovascular diseases with great prognostic significance or high therapeutic priority. Preoperative clarifications should already take place a few weeks before the planned date of surgery and can to a large extent be handled by the family doctor. In addition to the type of surgery and the general medical history, the assessment of physical performance is of crucial importance. In the laboratory, Hb and creatinine are of particular interest. Apparative examinations are only necessary for special indications.
Clarification aisle
The clarification procedure used in our clinic is summarized schematically in Figure 1 [1]. The algorithm was developed based on the guidelines of the American cardiology societies published in 2007 [2] and is also compatible with the latest international guidelines [3,4].
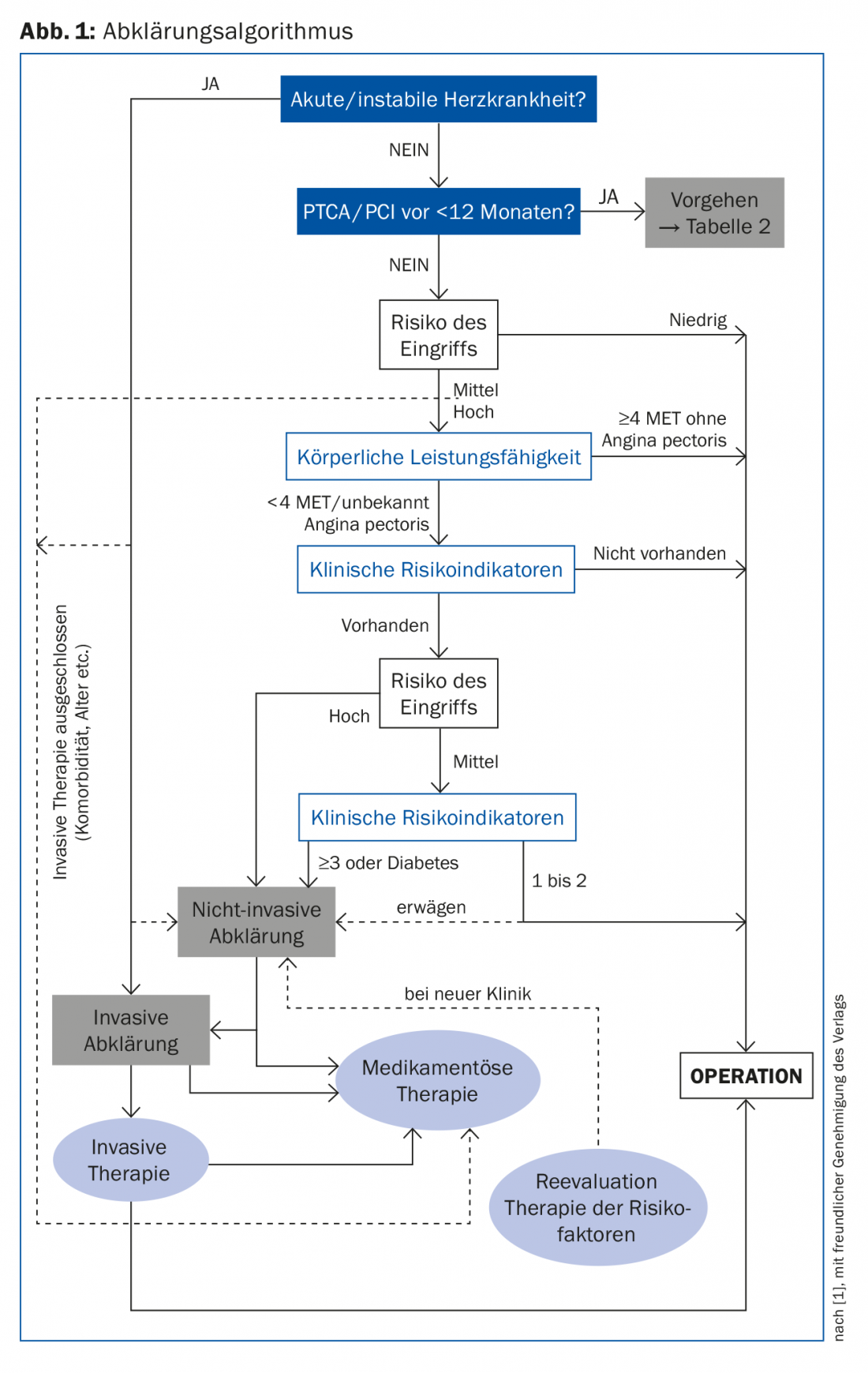
The first step is to identify or rule out acute or unstable heart disease (Tab. 1) . Particular attention should be paid to recent acute coronary syndromes (ACS) or recent coronary interventions. These require more intensive anticoagulant therapy and may force postponement of elective surgery.
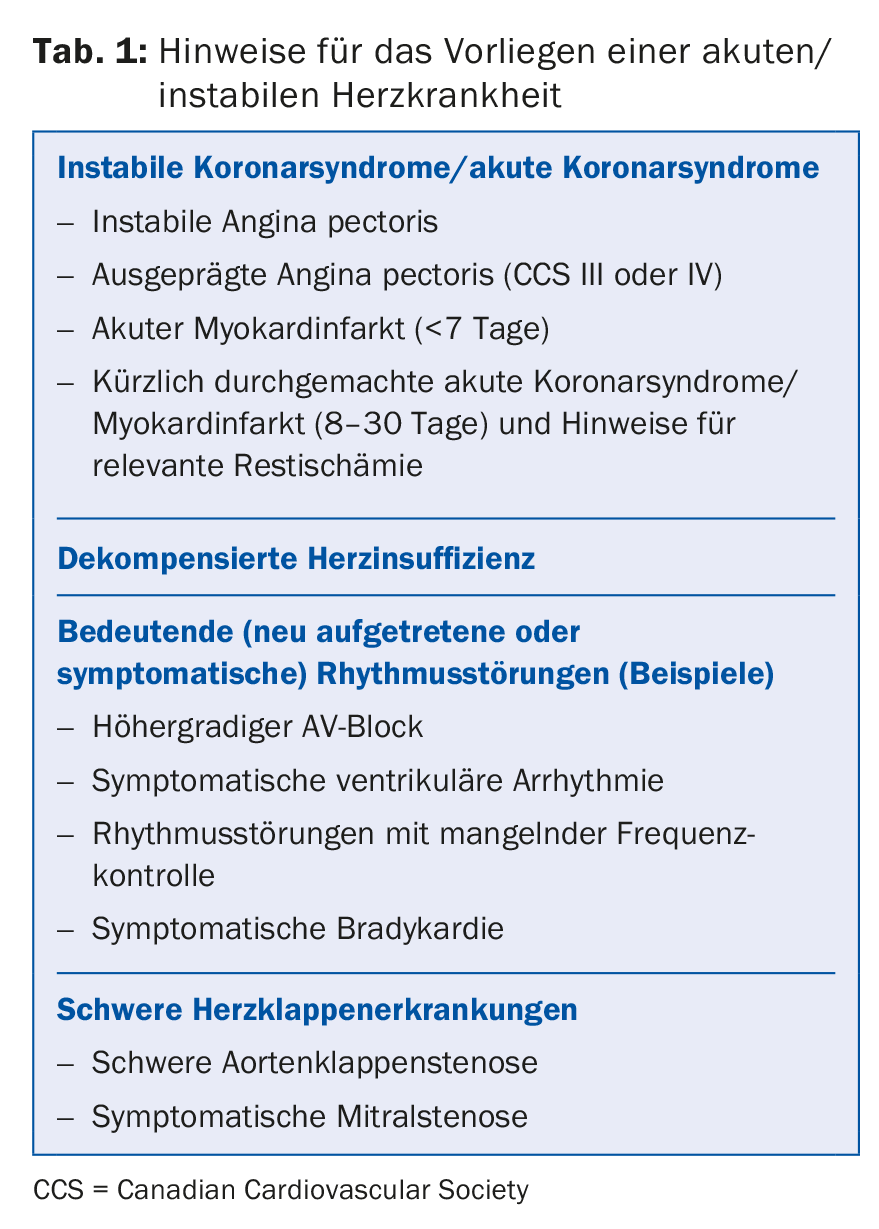
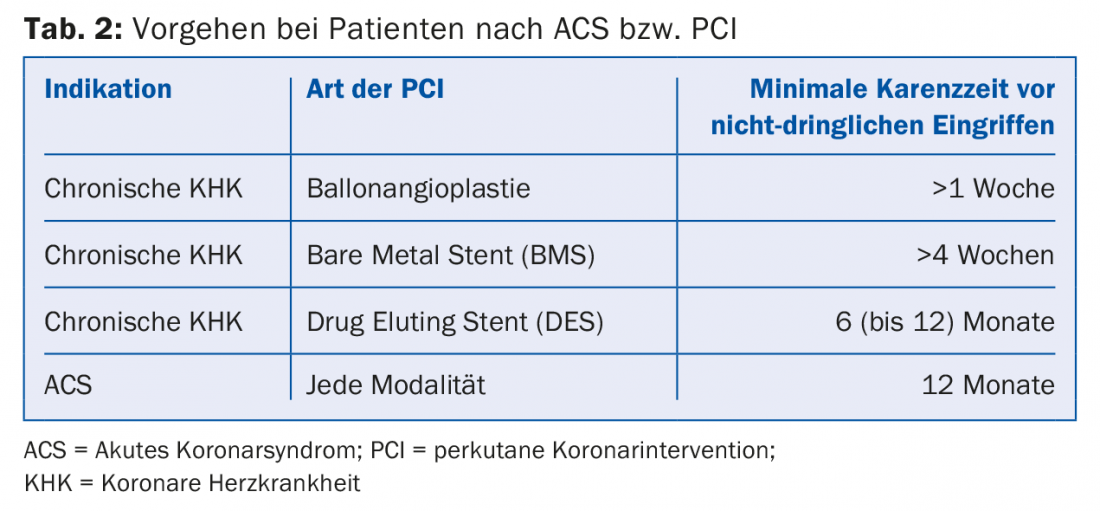
As a general principle, no elective procedures should be performed within the first twelve months after ACS and within the first six months after implantation of a drug-eluting stent (DES) in a coronary artery (Tab.2). Patients requiring urgent surgery within these timeframes are at very high perioperative risk and must be pre-discussed with surgeons, anesthesiologists, cardiologists, and intensivists on an interdisciplinary basis. If acute or unstable heart disease has been ruled out, the further procedure is based on the (cardiovascular) risk of the upcoming procedure (Tab.3), the physical capacity of the patient (Fig. 2) and the presence of clinical risk indicators. (Tab.4). These include documented coronary artery disease, drug-treated diabetes mellitus, history of heart failure, or presence of renal insufficiency (serum creatinine >170 μmol/l or calculated creatinine clearance [eGFR] <60 ml/min/1.73m2). Of great importance is the estimation of the physical capacity. A few simple questions about activities of daily living allow them to be roughly quantified. If a patient is able to climb two flights of stairs without stopping (which corresponds to an oxygen uptake of >4 metabolic equivalents [MET] ), performance is considered sufficient. Thus, based on the educational algorithm, patients with good exercise capacity (>4 MET) and/or lack of risk indicators do not require further cardiac workup and can be assigned directly to surgery.
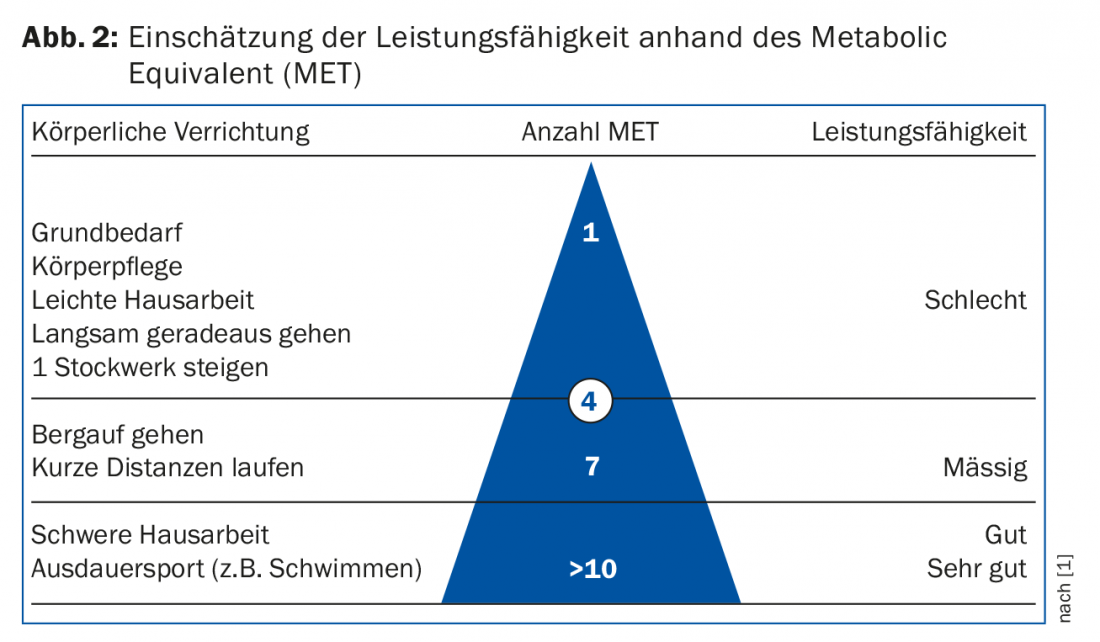
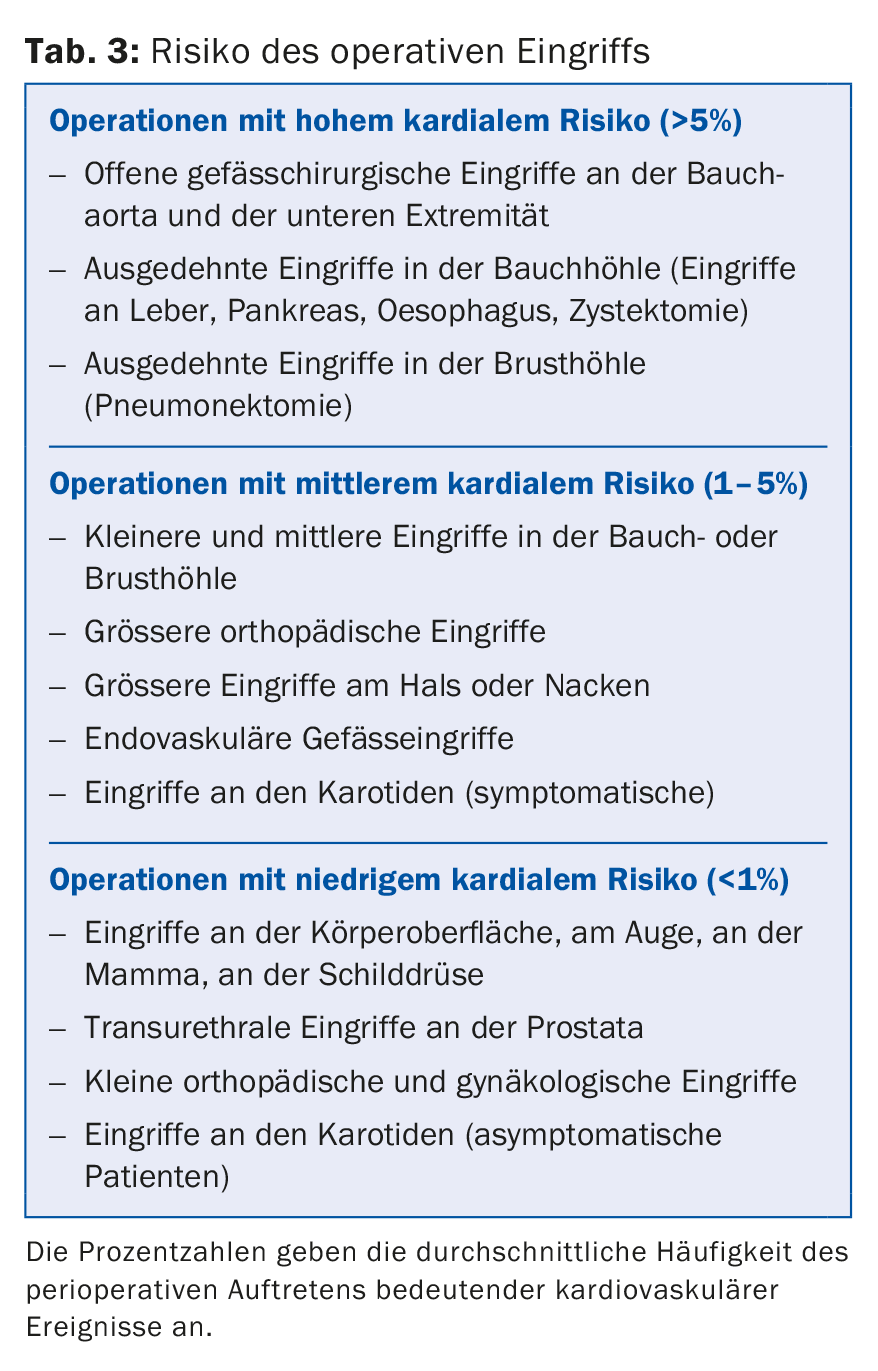
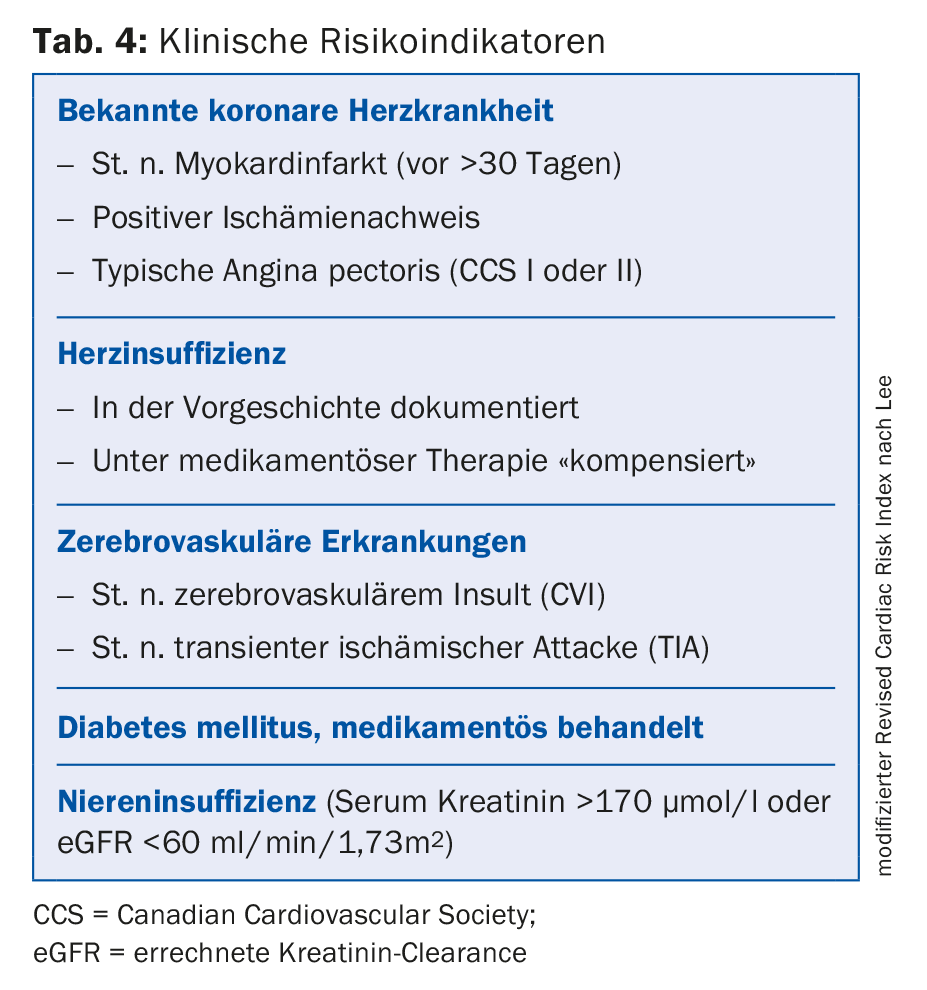
If, on the other hand, performance is impaired (or if this cannot be evaluated without doubt on the basis of medical history) and clinical risk indicators are present, a cardiological assessment must be considered, especially in advance of major surgical procedures with moderate or high cardiovascular risk (tab. 3) . The indication for further investigations depends on the suspected or excluded cardiac disease and is always based on general internal medicine and cardiology guidelines. Clarifications solely with a view to surgical intervention are hardly ever useful.
If coronary artery disease is suspected, myocardial ischemia imaging (myocardial scintigraphy, dobutamine stress echocardiography, stress MRI, etc.) is usually performed, while cardiac vitals are further clarified by echocardiography. These examinations belong under the aegis of the cardiologist and should be discussed with him.
If pathological findings are revealed by the apparative examinations, the therapy follows the generally accepted cardiological-internal criteria. This therapy primarily focuses on the long-term benefit for the patient, but also serves to optimize it with regard to the upcoming surgery.
In recent years, the preoperative determination of brain natriuretic peptide (BNP) or NT-proBNP has gained importance in the preoperative work-up, and especially the negative predictive value of this examination is well documented. Accordingly, a non-elevated value predicts with high confidence a perioperative course free of cardiovascular complications [5].
Of course, every cardiovascular risk patient should have an ECG performed prior to major surgery. It is also very important to check the kidney function and the red blood count, followed by a possible anemia evaluation.
Perioperative drug therapy
Perioperative drug therapy is based on the general principles of internal medicine and cardiology. Statins and beta-blockers, if indicated, should be started several weeks before the planned surgery, if possible, and continued beyond the perioperative period. Therapy with platelet aggregation inhibitors and other anticoagulant drugs is of great importance. Depending on the indication or risk for the occurrence of cardiovascular complications and depending on the potential bleeding complications associated with the procedure, they should be continued unchanged, reduced, or discontinued altogether. This topic is summarized in reference [6] and [7]. In our clinic, the use of the “coagulation map” has proven successful in this regard [8], which can be downloaded via the Internet or ordered from the authors.
Special situations
Heart failure: Heart failure is one of the most important perioperative risk factors and requires careful medication optimization. The general internal cardiological therapy recommendations also apply here. In this situation, the determination of BNP or NT-proBNP can not only provide diagnostic information, but can also be used as a follow-up parameter for the quality of drug therapy. In principle, medications for the treatment of heart failure are passed on unchanged perioperatively. Newly diagnosed heart failure requires a prolonged stabilization period, usually lasting several months [4].
Aortic valve stenosis: Previously, the presence of aortic valve stenosis was considered a contraindication for virtually all elective procedures. Today, in addition to the severity of the stenosis, great attention is paid to the patient’s symptomatology, so that even asymptomatic patients with formally severe aortic stenosis can be admitted for elective surgery, taking into account the hemodynamic circumstances. Such a procedure, however, requires an interdisciplinary discussion in which the indication and usefulness of an aortic valve replacement or the temporal procedure with regard to the non-cardiac surgery are evaluated and discussed with the patient.
Coronary artery disease: especially in vascular surgery patients, coronary artery disease is very common and must be looked for in impaired exercise capacity. Again, the indications for possible revascularization are consistent with general cardiology guidelines. However, the need for more intensive antiplatelet treatment after PCI must be taken into account.
Drug therapy with aspirin, statins, beta blockers, ACE inhibitors, etc. should be reviewed at an early stage and expanded where necessary. As a rule, the medication is continued unchanged preoperatively.
Perioperative phase
The perioperative phase is associated with pain, volume shifts, prolonged fasting, immobilization, etc., especially in major surgery. As a result, the patient’s previously achieved homeostasis is significantly disturbed, which not infrequently makes a modification of the pre-existing chronic medication unavoidable. Even with a favorable course of healing, the stable previous condition is not always restored at the time of hospital discharge, so that the medication requires further adjustments after hospital discharge. This task is usually the responsibility of the primary care physician.
Summary
Preoperative cardiac workup is an integral part of the preoperative evaluation of a patient before surgery. The main pillars are the assessment of physical capacity, the presence of clinical risk indicators and the risk of the upcoming procedure. Apparative cardiological examinations are only necessary in a small proportion of patients. Special attention must be paid to optimizing drug therapy; this is based on the generally accepted principles of internal medicine and cardiology. Today, virtually all chronic medication is passed on perioperatively as unchanged as possible. An important exception to this rule is anticoagulant medications, which not infrequently require adjustment. After hospital discharge, the cardiac risk patient must continue to be monitored closely and medication must be restored to a chronic balance.
Literature:
- Filipovic M, et al: Perioperative cardiac evaluation and therapy in the setting of noncardiac surgery. Update 2008. Schweiz Med Forum 2008; 8: 935-938.
- Fleisher LA, et al: ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation 2007; 116: 1971-1996.
- Fleisher LA, et al: 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 130: 2215-2245.
- Kristensen SD, et al: 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 2014; 35: 2383-2431.
- Devereaux PJ, Sessler DI: Cardiac Complications in Patients Undergoing Major Noncardiac Surgery. N Engl J Med 2015; 373: 2258-2269.
- Filipovic M, Korte W, Rickli H: Perioperative management of coagulation: “old” and “new” oral anticoagulants. Cardiovascular Medicine 2015; 18: 340-343.
- Koenig-Oberhuber V, Filipovic M: New antiplatelet drugs and new oral anticoagulants. Br J Anaesth 2016; 117 Suppl 2: ii74-ii84.
- Filipovic M, Korte W, Rickli H: Thrombosis prophylaxis and periinterventional antithrombotic therapy at the Cantonal Hospital St. Gallen. 6th ed. 2016. www.kardiologie.kssg.ch/home/aerzte_fachpersonen/thromboseprophylaxe-und-periinterventionelle-antithrombotische-t.html.
HAUSARZT PRAXIS 2017; 12(1): 8-12