The biggest enemy of fitness to drive – from a sleep medicine perspective – is sleepiness. The most common underlying cause is obstructive sleep apnea syndrome (OSAS). “Drowsiness: greater traffic hazard than alcohol” – “Drowsiness: a greater risk for causing traffic accidents than alcohol”. This statement is explored in the CME article.
You can take the CME test in our learning platform after recommended review of the materials. Please click on the following button:
The biggest enemy of fitness to drive – from a sleep medicine perspective – is sleepiness. The most common underlying cause is obstructive sleep apnea syndrome (OSAS). “Drowsiness: greater traffic hazard than alcohol” – “Drowsiness: a greater risk of causing traffic accidents than alcohol”. This statement will be investigated below [1].
According to the Federal Statistical Office, a total of 2,512,899 road accidents were recorded by the police in Germany in 2023. In this context, 366,478 people were involved in accidents, 52,464 people were seriously injured and 28,178 people were fatally injured. Overall, the number of road deaths has been falling sharply for years, as has the number of serious injuries. The reasons for this are, on the one hand, legal regulations such as maximum speeds on country roads, mandatory use of helmets, seat belts and child seats and changes in blood alcohol concentrations. Other factors include improved vehicle technology and road construction measures [2].
Looking at driver misconduct in accidents involving personal injury, 15,145 of 339,834 accidents involving personal injury were attributable to the influence of alcohol [2]. In the following, the significance of the factors drowsiness and OSAS on the accident frequency when driving a motor vehicle will be presented. In addition, existing regulations in Germany for the assessment of fitness to drive in the case of drowsiness/OSAS are presented.
Drowsiness, fatigue: definitions
The terms “sleepiness” and “fatigue” are often and incorrectly used interchangeably, but have different meanings. Sleepiness is defined as the inability to stay awake under low-stimulus conditions, especially at times of circadian rhythmic performance lows.
Fatigue, on the other hand, refers to a state of exhaustion with a need for rest and recuperation. It is often accompanied by symptoms of depression and difficulties in finding sleep and therefore rest [3]. Fatigue in conjunction with difficulty falling asleep and staying asleep can therefore also be a sign of depression. As the terms “fatigue” and “drowsiness” are often used interchangeably in statistical surveys and scientific papers, it is not possible to clearly differentiate between fatigue-related and drowsiness-related accidents, but it is likely that the vast majority of accidents are drowsiness-related events, i.e. unintentionally falling asleep at the wheel. In order to apply a uniform diction, the term drowsiness is used in the following.
Drowsiness and accident risk
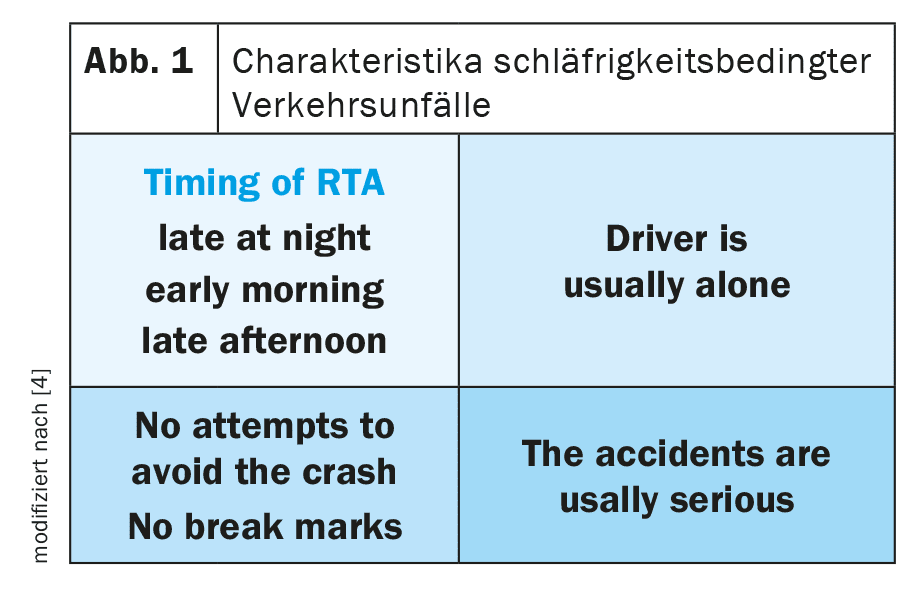
Drowsiness-related accidents have specific characteristics. They usually occur in the late evening and early morning hours. A further accumulation can be observed in the early afternoon. Both periods coincide with the circadian, physiological performance lows. As a rule, the driver is alone, i.e. there is no passenger present who could point out or warn of an imminent danger. The accidents are usually those with serious consequences. Furthermore, there is often no evidence of an attempt to avoid the accident, such as skid marks. Figure 1 shows the characteristics of drowsiness-related accidents [4].
As early as 1969, the Federal Court of Justice decided in a guiding principle: “According to the current state of medical science, experience shows that a driver always perceives or at least can perceive clear signs of fatigue (overtiredness) before he falls asleep (nods off) at the wheel of his vehicle while driving. An exception to this is the (rare) case where the driver suffers from narcolepsy” [5]. The fact that this guiding principle, in particular the passage “…always perceives clear signs of fatigue (overtiredness)” is by no means correct is proven by statements from patients with drowsiness-related accidents, who often state that the microsleep event occurred without prodromes.
Nevertheless, there are signs of drowsiness at the wheel. These include frequent yawning, eye blinking, eye rubbing, heavy eyelids and burning eyes. The most common countermeasures include turning up the radio and lowering the car windows to get some fresh air. However, making phone calls or even increasing driving speed to get that certain “kick” are also among the coping strategies, but these are not effective from a sleep/traffic medicine perspective.
In a survey conducted in the USA by the National Safety Council in 2005, 60% of respondents reported drowsiness when driving a vehicle. 17% had already fallen asleep at the wheel. Based on the data, it must be assumed that 10-30% of accidents in the USA were due to drowsiness at the wheel [6].
In a New Zealand study, 571 car drivers who had caused accidents with injuries/fatalities were compared with 578 drivers without accidents. Under the following conditions, the relative risk (OR, 95% confidence intervals in brackets) of causing an accident with injuries or fatalities was increased:
- The driver’s statement that he felt drowsy immediately before the accident: OR 8.2 (3.4-19.7)
- Less than 5 hours of sleep in the past 24 hours: OR 2.7 (1.4-5.4)
- Driving between 2.00-5.00 a.m. in the morning: OR 5.6 (1.4-22.7)
In this study, there was no increase in the risk of traffic accidents among drivers suffering from chronic fatigue [7].
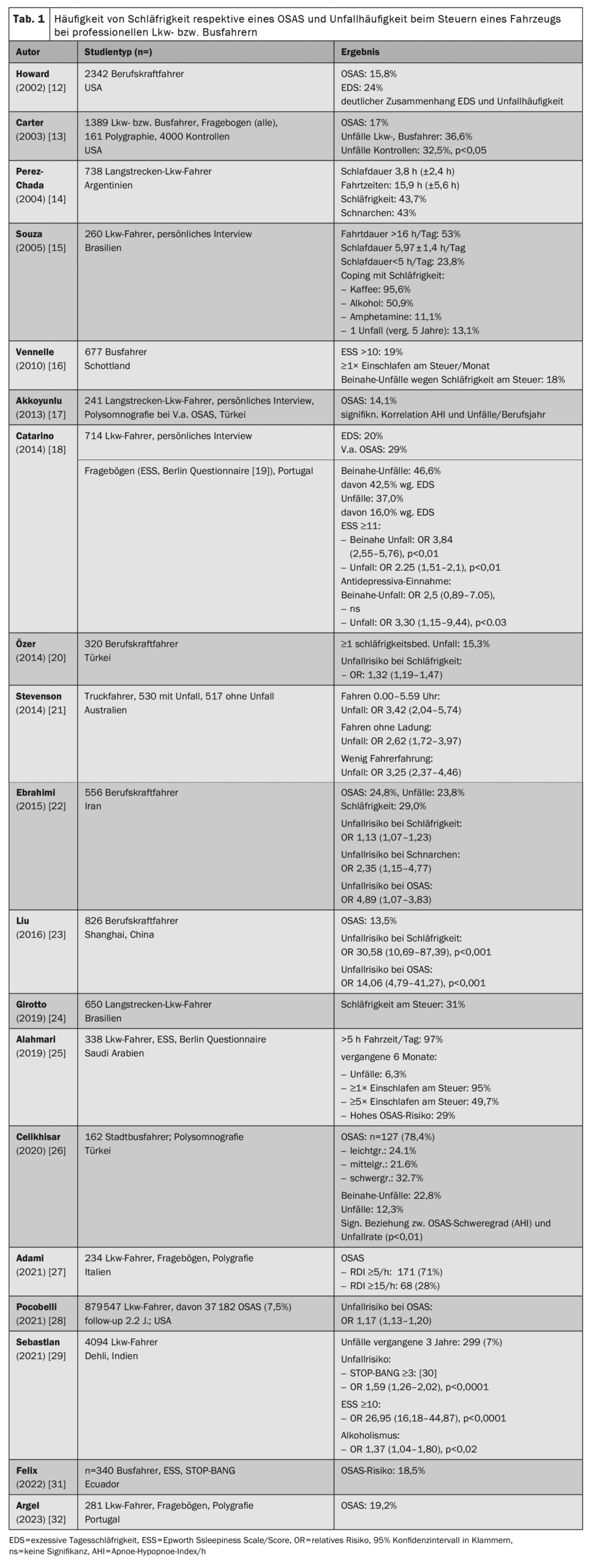
Sleepiness per se, without the presence of other sleep disorders, increases the relative risk of a traffic accident by a factor of 2.1. If OSAS is also present, the relative risk is 2.19 and therefore does not contribute to a significant increase in the risk of an accident. Figure 2 shows the relative risk of self-reported accidents for sleep disorders, sleepiness and OSAS compared to controls. It is noteworthy that in the presence of daytime sleepiness, additional OSAS does not significantly increase the relative risk of causing an accident [8].
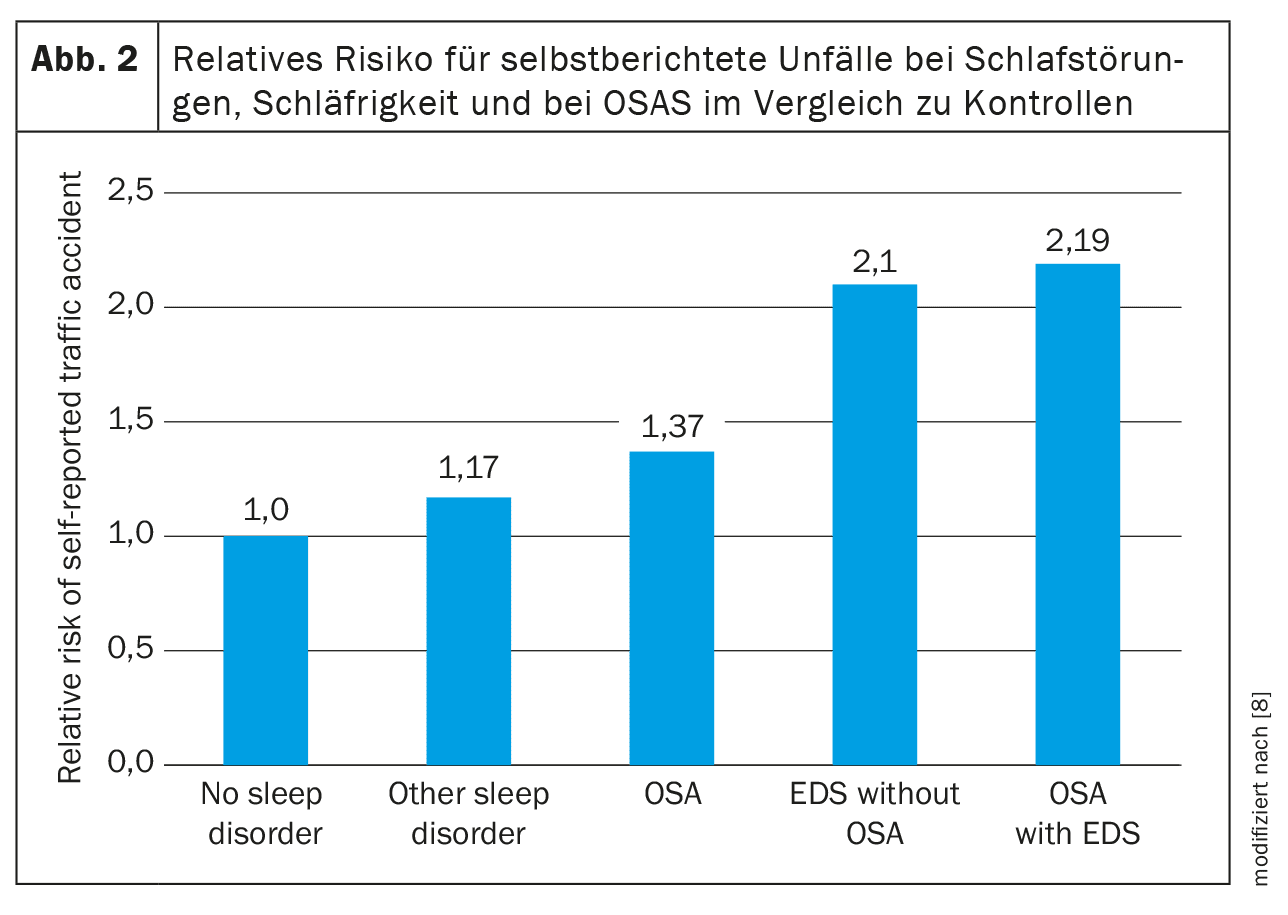
The importance of daytime sleepiness for the frequency of accidents in patients with OSAS is also underlined by a recent study by Sabil et al. (see also Table 2 and Figure 3). The study examined 843 patients with OSAS. Their data on drowsiness at the wheel and accidents caused in the last 5 years were rather moderate compared to other studies (drowsiness at the wheel 3.4%, traffic accidents 3.6%, near-accidents 16.3%). Previously experienced drowsy driving and an Epworth score ≥11 led to a significant increase in the risk of causing an accident [9,10].
Philip et al. compared the predictive value of self-reported sleepiness at the wheel with the objectively measured apnea-hypopnea index (AHI). 58,815 participants with suspected OSAS (polygraphy, polysomnography) took part in the study. The mean AHI in the overall collective was 22.0/h (8-39). The average Epworth score was 9 (6-13). 35% of the subjects reported drowsy driving, 8% had caused near-accidents and 2% had caused accidents due to drowsy driving. The authors then compared the frequency of accidents at different levels of OSAS severity as measured by the AHI (AHI <10/h, AHI ≥10/h, AHI <30/h, AHI ≥30/h) with and without the presence of drowsiness. The results showed that it was not the severity of OSAS measured by AHI, but rather the presence of sleepiness that was decisive for causing (near) accidents. Figure 4 shows the accident risk in subgroups, divided according to OSAS severity and the absence or presence of drowsiness at the wheel [11].
The following comments on daytime sleepiness with consecutive accident frequency among professional truck/bus drivers and car drivers relate exclusively to OSAS.
Daytime sleepiness, OSAS and accident proneness in truck drivers – yesterday and today
Initially, the focus of accident medical sleep research was on truck and bus drivers. This is easy to understand, as they are often involved in heavy transportation, the transportation of hazardous goods or even people with consecutive high-profile accidents. In addition, the physiognomy of many truck drivers predisposes them to OSAS.
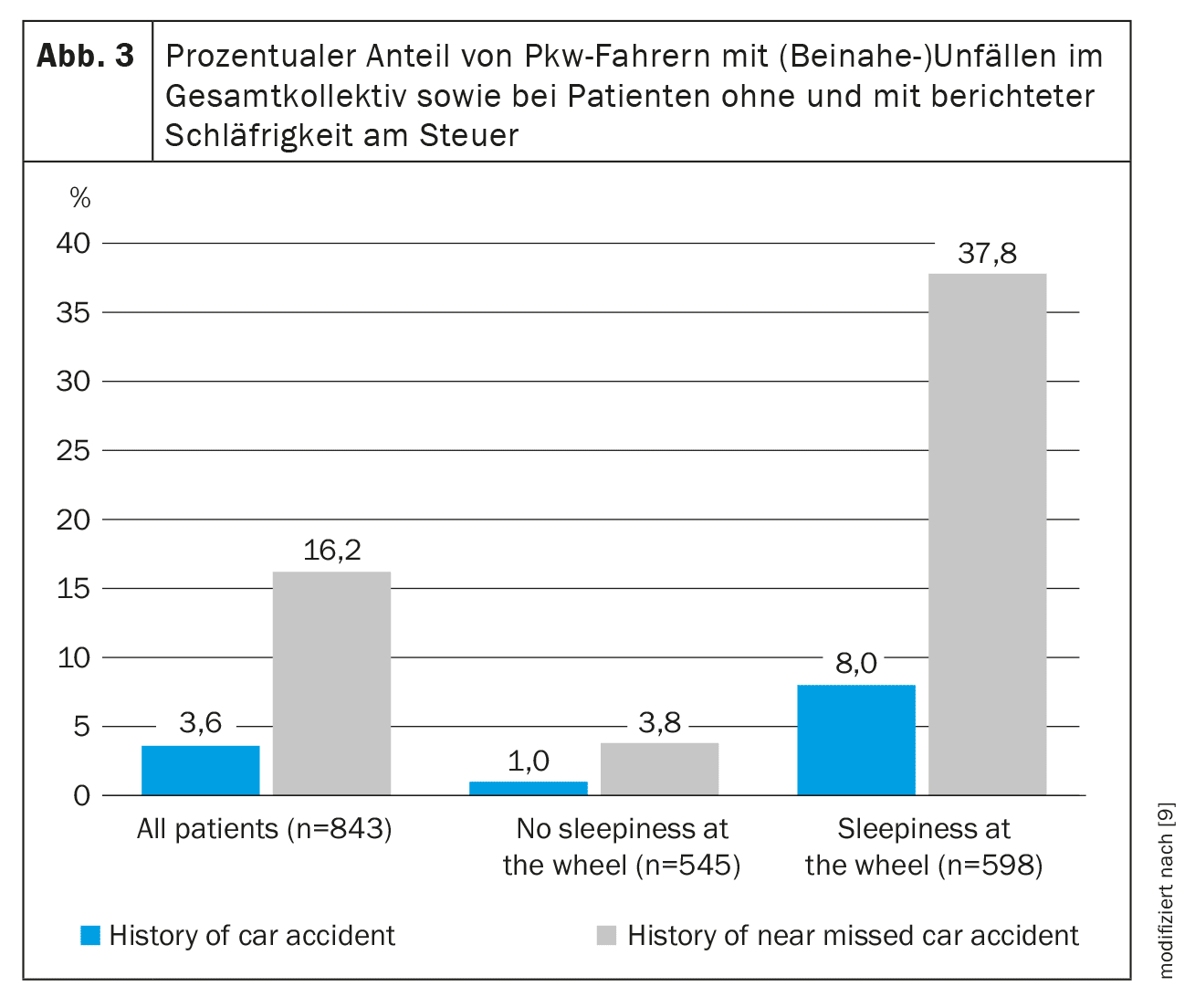
Table 1 shows the frequency of drowsiness or OSAS when driving a vehicle among professional truck and bus drivers [12-32].
The following results can be summarized from the studies:
- Compared to the normal population, in which an OSAS frequency of 13% in men and 6% in women is assumed (AHI ≥15/h + daytime sleepiness, 30-70 years of age) [33], this is increased in professional drivers.
- Despite numerous campaigns, little or nothing has changed in the frequency of OSAS or drowsiness while driving among professional drivers over the 20-year period shown.
- There is a close link between daytime sleepiness and (near) accidents.
- Excessively long driving times, far too short sleep and rest breaks are not uncommon and, it is easy to understand, increase drowsiness.
The study by Girotto et al. analyzes the working conditions that increase the relative risk (OR) for the occurrence of drowsiness at the wheel. These include:
- a distance from the last shipment of more than 1000 km -> OR 1.54 (1.07-2.23),
- an employment contract with performance-related remuneration -> OR 2.65 (1.86-2.23),
- the use of illegal psychoactive drugs -> OR 1.99 (1.14-3.47) [24].
In an industry with high competitive pressure (e.g. bus trips to other countries at dumping prices or often only one driver per means of transport (which means a financial loss for the operator if the driver breaks down and cannot be replaced) and moderate pay, the first two points in particular play a key role in the authors’ view for driving under conditions that actually prohibit it.
The importance of psychoactive drugs as factors promoting drowsiness and consecutive accident frequency on the one hand, and as “coping strategies” for dealing with drowsiness on the other, should not be underestimated.
In the study Catarino et al. the use of antidepressants increased the relative risk of causing an accident by a factor of 3.30 (1.15-9.44), p<0.03 [18]**. Looking at the study by Souza et al., the coping strategies for dealing with drowsiness at the wheel include coffee (95.6% of drivers, legitimate, but: no long-term effect) and alcohol (50.9% of drivers, prohibited, promoting drowsiness and the tendency to fall asleep) as well as the use of amphetamines (11.1% of drivers, illegal) [15].
** Authors’ note: Portugal had the highest death rate due to traffic accidents at the time of the 2014 study
Bus drivers with drowsiness at the wheel or OSAS and the people they transport are also at risk. The studies on bus drivers also showed an increased prevalence of OSAS and an increased accident rate compared to the general population. The corresponding studies included both city bus drivers and long-distance bus drivers [13,16,26]. The predominant accident patterns in drowsiness-related accidents are lane departure and rear-end collisions [34].
Naps and breaks can significantly reduce the relative risk of causing an accident or (near) accident. In a study of 949 drivers, 34.9% of whom had caused accidents and 9.2% of whom had caused (near) accidents, the relative risk of a traffic accident was reduced to 0.59 (0.44-0.79) by taking “naps” and to 0.59 (0.45-0.89) by taking breaks. The relative risk of causing a (near) accident was reduced to 0.52 (0.32-0.85) by taking naps and to 0.49 (95% CI 0.29-0.82) by taking breaks [35].
Daytime sleepiness and accident propensity in car drivers – yesterday and today
It is not only the spectacular accidents involving truck or bus drivers and the transportation of hazardous goods that need to be taken into account. Car drivers also cause accidents due to drowsiness at the wheel. As early as the 1980s and 1990s, Findley et al. demonstrated that the accident rate of patients with OSAS in the simulated driving situation was around 7 times higher than that of healthy people, and that these results also correlated well with the accidents actually caused [36,37].
In 1994, a study by the HUK association showed that in 1991, drowsiness/drowsiness at the wheel was the cause of 24% of accidents with fatalities on Bavarian highways [38].
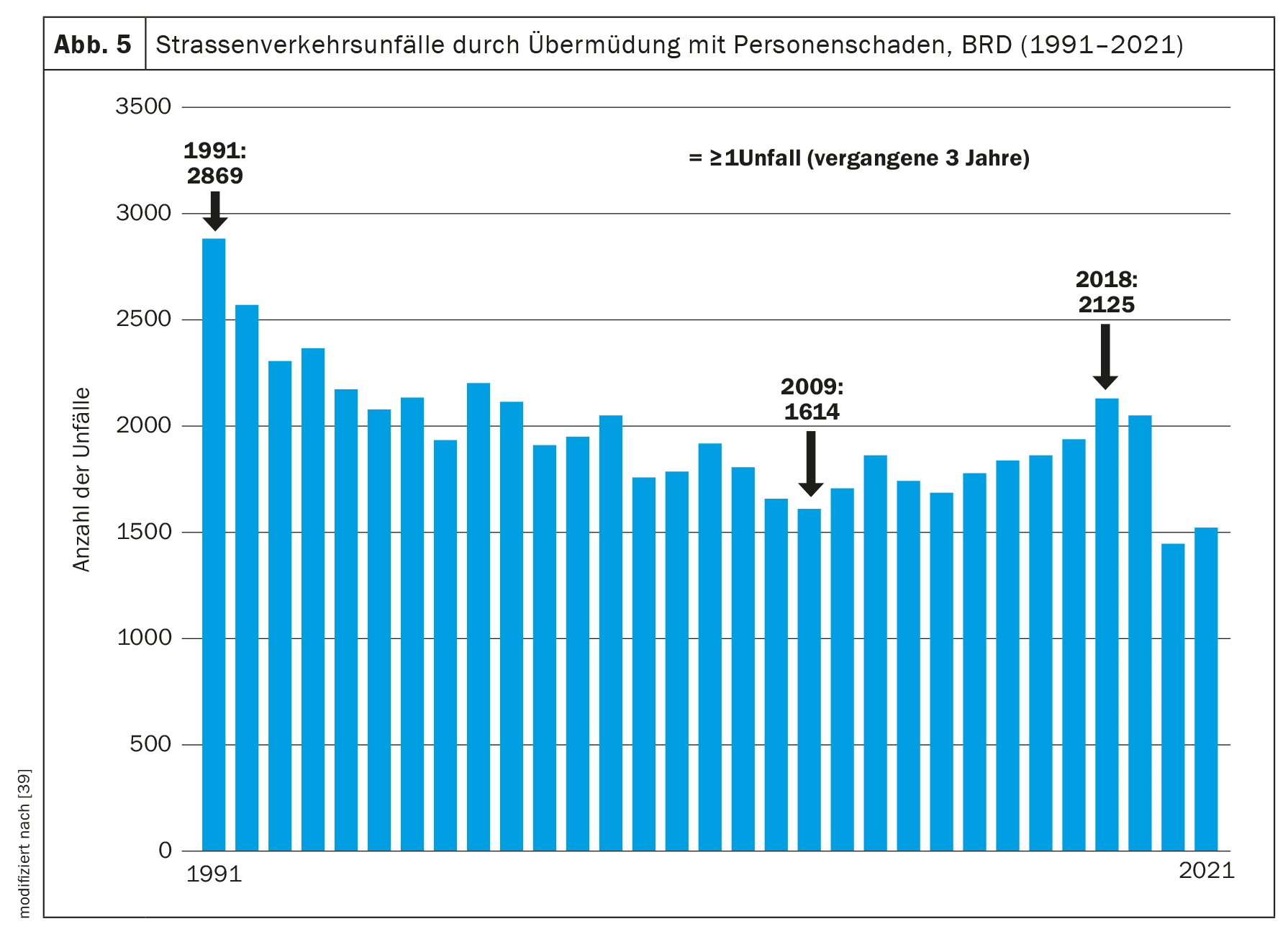
The statistics on road accidents caused by fatigue/drowsiness at the wheel in Germany in the period from 1991 to 2021 show a continuous decline in accident frequency from 1991 with 2869 accidents to 2009 with 1614 accidents. From 2010, the frequency of accidents caused by fatigue increased again until 2018 with a number of 2124 accidents, from 2018 to 2021 the number of accidents decreased again (Fig. 5) [39]. Table 2 shows a list of studies on accident frequency and accident risk due to drowsiness or OSAS in car drivers.
The prospective pilot study by Purtle et. al. The study examined 80 patients with trauma as a result of a car accident. The results showed that there was a high risk of OSAS in 26% of the traumatized patients in the collective examined [54]. In a meta-analysis of 2022, which included 49 studies on the topic of “OSAS and accident frequency”, a significantly increased relative risk of causing an accident was found in all collectives compared to the controls, both in the overall collective (OR 2.36; 1.92-2.91; p<0.001) and in the differentiation between professional drivers (OR 2.8; 1.82-4.31) vs. car drivers (OR 2.32; 1.84-2.34). Furthermore, around 25% of serious truck accidents were attributable to drowsiness at the wheel. Most of these accidents occur at night [58].
The EU bus study
The most comprehensive and, with regard to the revision of the driving license regulation, the most important study of car drivers on the subject of “drowsy driving” and other risk factors for causing accidents among car drivers is the so-called “EU bus study” from 2015. Starting in Portugal, the bus visited all EU countries. On board the bus were qualified sleep physicians who were supported by local sleep specialists in the respective capital cities. In addition to information events and on-site consultations, a questionnaire was also provided. When asked about the frequency of falling asleep at the wheel, the responses varied between 6.2% (Croatia) and 34.7% (Netherlands). In Germany, the proportion of those who had ever fallen asleep at the wheel was in the middle third at 17.1%. The frequency of accidents caused by drowsiness at the wheel was reported to be between 0% (Turkey, Netherlands) and 2.7% (Estonia); in Germany, 1.2% of accidents were caused by falling asleep at the wheel. Risk factors for causing drowsy driving-related accidents in car drivers were male gender (OR 1.79; 1.61-2.00), the number of kilometers driven [10,000-19,999km: OR 1.36; 1.16-1.58; ≥20,000 km: OR 2.02; 1.74-2.35]. Other risk factors were the severity of OSAS (measured by AHI) and an elevated Epworth score ESS ≥10 (42% of car drivers). Figures 6A-D show the risk factors mentioned and the associated accident risk [59,60].
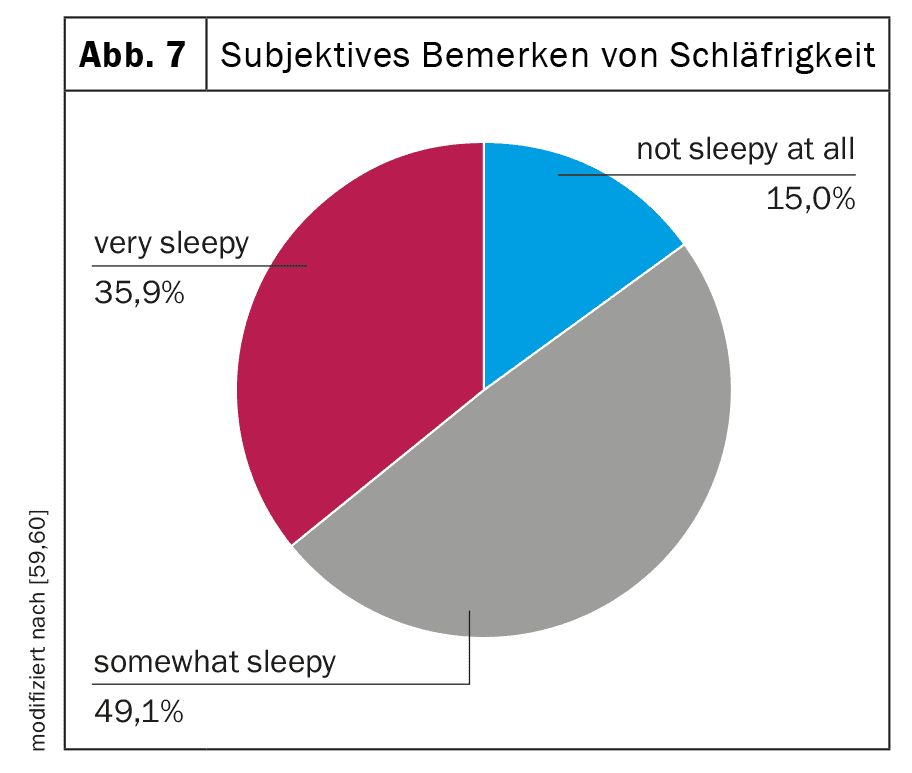
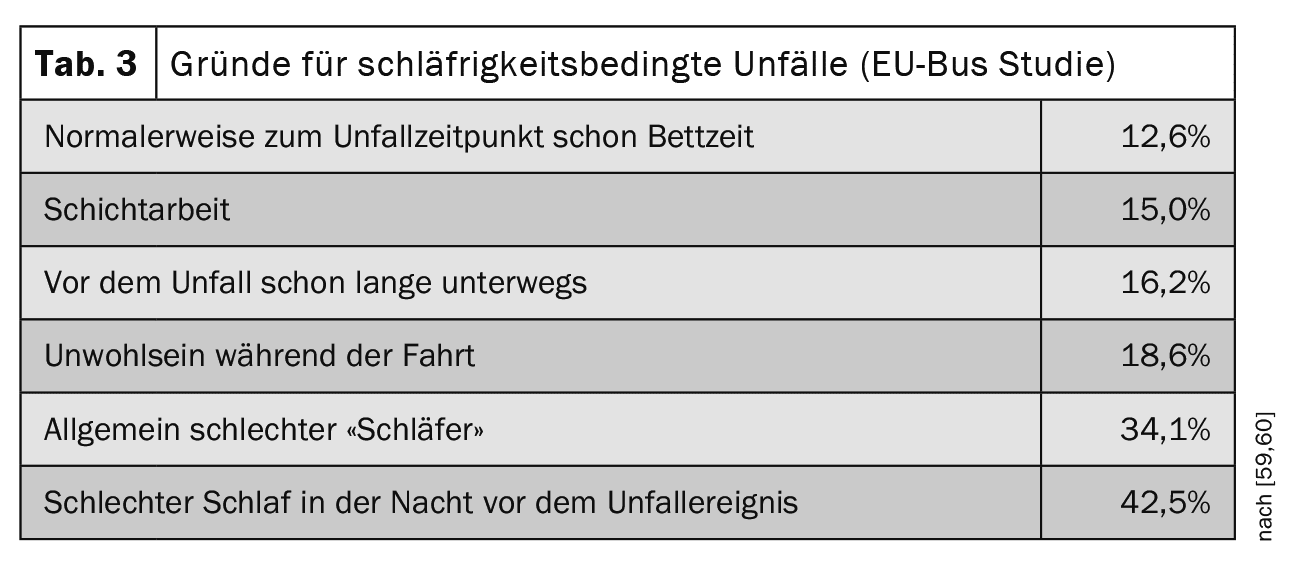
The fact that almost 90% of the drivers did not react adequately (e.g. break, fresh air, coffee, nap) to the drowsiness they noticed (35% pronounced, 49.1% moderate) is incomprehensible (Fig. 7). In terms of vehicle type, 90% of the accidents involved passenger cars and 56% occurred on highways. Table 3 shows the reasons for causing drowsiness-related accidents. The main reasons were poor sleep quality the night before the accident and generally poor sleep quality [59,60].
The EU Directive
The results of the EU bus campaign were presented to the EU Parliament in October 2013. Together with the “Council on Driving Licenses”, a directive was issued in July 2014 [61]. The contents of the directive are summarized below.
It is noted,
…that OSAS is one of the greatest risk factors for causing an accident and that this
…can no longer be ignored with a view to the uniform issuing of driving licenses in the EU (Article 1, paragraph 2).
The directive also defines a severity classification of OSAS:
-> Moderately severe OSAS: AHI 15-29/h
-> Severe OSAS: AHI ≥30/h
in each case in connection with excessive “daytime sleepiness” (Article 11, paragraph 2). It should be noted here that the somnologist/sleep physician would have preferred the term “daytime sleepiness” (see previous explanations for definition) instead of the term “daytime sleepiness”.
The directive goes on to comment on the treatment of drivers suspected of having OSAS. Article 11, paragraph 3 provides for the following:
Applicants or drivers with suspected moderate or severe OSAS must
- obtain a medical certificate (from a recognized medical authority) and present it before the driver’s license is issued or renewed. If this is not the case, it may be necessary to advise against driving until a diagnosis has been made (Article 11, paragraph 3).
- The directive also called on the member states to draw up the laws and regulations resulting from Article 1, paragraph 2 by 31.12.16 at the latest.
In Germany, the timely implementation was carried out by the Federal Highway Research Institute (BaSt – Assessment Guidelines on Fitness to Drive [62]) in close consultation with sleep medicine experts. The contents of the BaSt guidelines for the assessment of fitness to drive with regard to “measurably conspicuous daytime sleepiness” or OSAS are summarized below.
The assessment guidelines were drawn up on the basis of the following principles:
- Anyone suffering from moderate or severe OSAS is not able to meet the requirements for driving a motor vehicle in either group.
- Applicants or drivers suspected of having moderate or severe OSAS must undergo an examination by the relevant specialist discipline using sleep medicine or somnology qualifications before a driving license is issued or renewed. The specific practical procedure is staged:
Stage 1: Medical history
The following factors should be taken into account:
- Disturbed attention, especially in monotonous situations (reading, watching television, sitting quietly),
- Falling asleep or microsleep in monotonous situations,
- Unintentional or compulsive falling asleep, even in socially demanding situations,
- standardized questionnaires.
Stage 2: Measurement method for daytime sleepiness/wakefulness and alertness
This involves testing the attention components required when driving a motor vehicle [63,64]. These include
a) simple alertness = ability to react quickly to a simple warning stimulus
b) Vigilance = long-term (at least 30 minutes) maintenance of attention in monotonous environmental conditions, e.g. long highway drive, night, no passengers,
c) sustained attention = longer-term (at least 30 minutes) maintenance of attention in non-monotonous environmental conditions, e.g. longer journeys in busy surroundings, traffic, passengers, attention to traffic signs/traffic lights, pedestrians
d) Divided attention = serial and parallel information processing; reaction to relevant stimuli from different stimulus sources, e.g. passengers, conversations, traffic, traffic lights (see below for test instruments suitable for attention).
Stage 3: Driving test
Monotony, at least 30 minutes, presence of an assessor.
Both neurophysiological (e.g. multiple sleep latency MSLT, multiple waking lead test, MWT, pupillography) and neuropsychological examination procedures with corresponding test instruments and driving simulators are available to carry out the examinations mentioned under a) to c) (see the following explanations).
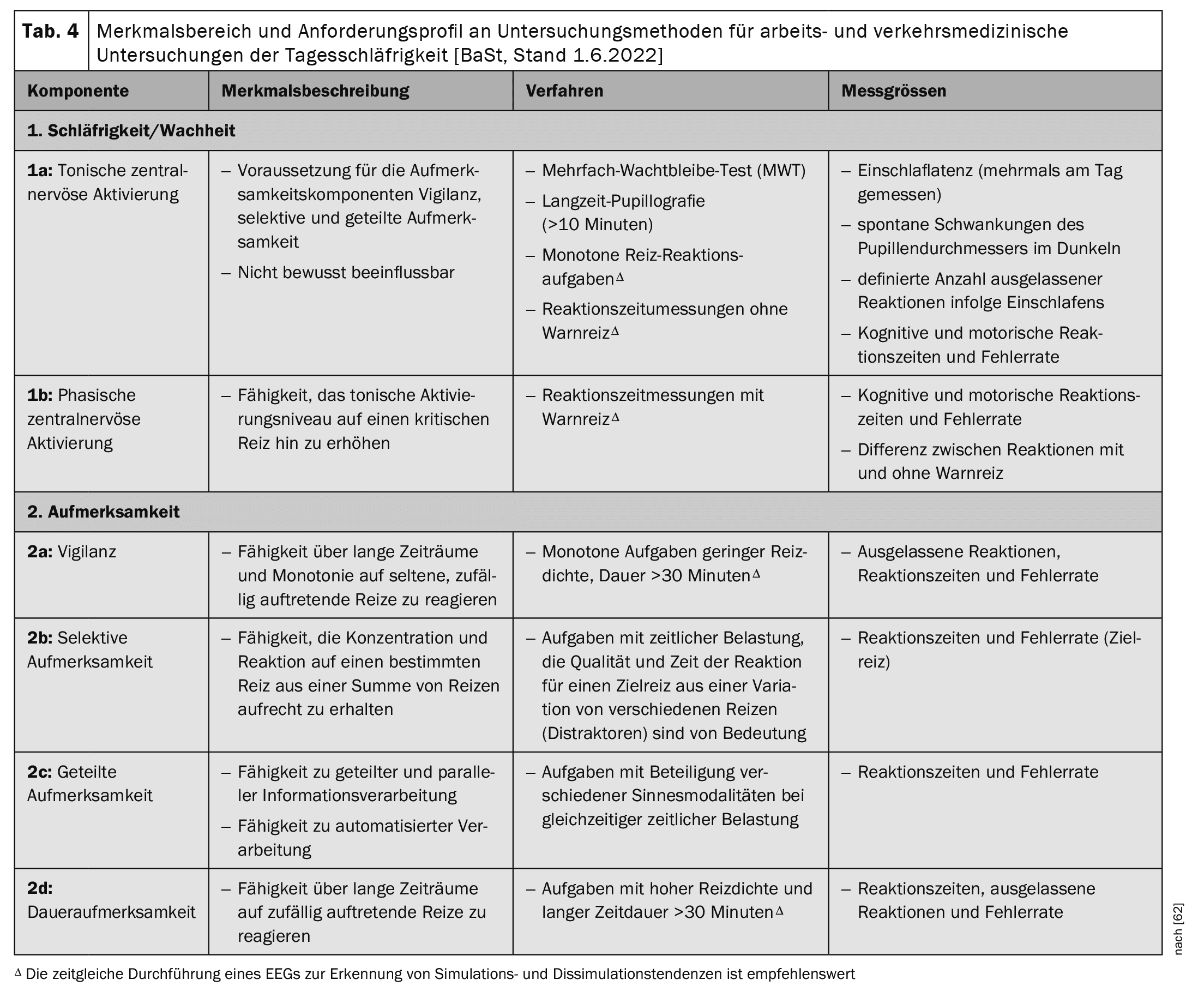
Table 4 shows the characteristic areas and the requirement profile for examination methods for occupational and traffic medical examinations of daytime sleepiness [62].
Assessment of fitness to drive with measurable abnormal daytime sleepiness (MATS) and OSAS with MATS
The assessment of fitness to drive is based on the respective test results. test results. In addition to the objective test results, the expert’s personal impression is an essential component in the assessment of fitness to drive.
Fitness to drive is given if: The drowsiness is successfully treated and the test result is documented by a new assessment. In this case, however, regular check-ups are required (Group 1: A1, A2, B, BE, AM, L, T every 3 years, Group 2: C, C1, CE, C1E, D, D1, D1E, passenger transport annually).
Not fit to drive if:
- ≥1 conspicuous result in the wakefulness/sleepiness/vigilance test
- ≥2 conspicuous findings as part of the attention test
- positive clinical symptoms and ≥2 borderline findings (vigilance or attention)
Conditional fitness to drive is given if: The driver to be assessed indicates a conscious perception of drowsiness and demonstrates responsible handling of drowsiness in road traffic (e.g. by interrupting the journey, taking a break) [62].
Neurophysiological test procedures: Multiple sleep latency test (MSLT) and multiple wakefulness test (MWT)
The neurophysiological examination methods are used to examine central nervous activation (level of alertness or sleepiness). This is the activity level, the activity level influenced by the autonomic nervous system and by physiological daily fluctuations. A distinction is made between a “tonic” (= stable level of alertness over a longer period of time, cannot be consciously influenced) and a “phasic” (= ability to increase the tonic activity level for a reaction to a warning stimulus) component [63,64].
During the MSLT, the patient lies in bed in a darkened room and is asked to fall asleep. At the same time, an electroencephalogram (EEG), electrooculogram (EOG) and electromyogram (EMG) are recorded. The procedure consists of four or five sessions, each lasting 20 minutes at two-hour intervals. The MSLT measures the average sleep onset latency (ESL) and the premature occurrence of so-called “SOREMP” (sleep onset REM sleep phases) within the first 15 minutes after falling asleep [65,66].
In the multiple wakefulness test, the room should be completely darkened and have a single, precisely defined, weak light source behind the subject’s head. The room temperature should be suitable for the subject’s well-being. The test person should sit leaning in bed with their head supported by a bolster. At the start of the measurement, the test person is asked to sit still, keep their eyes open and look forward and to stay awake for as long as possible and not to keep themselves awake with actions such as singing, pinching or standing up. The sleep architecture is also recorded in this test using EEG, EOG and EMG. The test is carried out in four sessions according to the 40-minute protocol at two-hour intervals. Sleep onset is the first epoch in which more than 15 seconds of sleep are detected. If no sleep occurs, the session ends after 40 minutes, otherwise after “definite sleep”, defined as three consecutive epochs in sleep stage N1 or one epoch in another sleep stage. Sleep onset latency is defined as the time until sleep onset or 40 minutes if sleep is missed [65,67]. The results of these tests are directly related to the number of accidents.
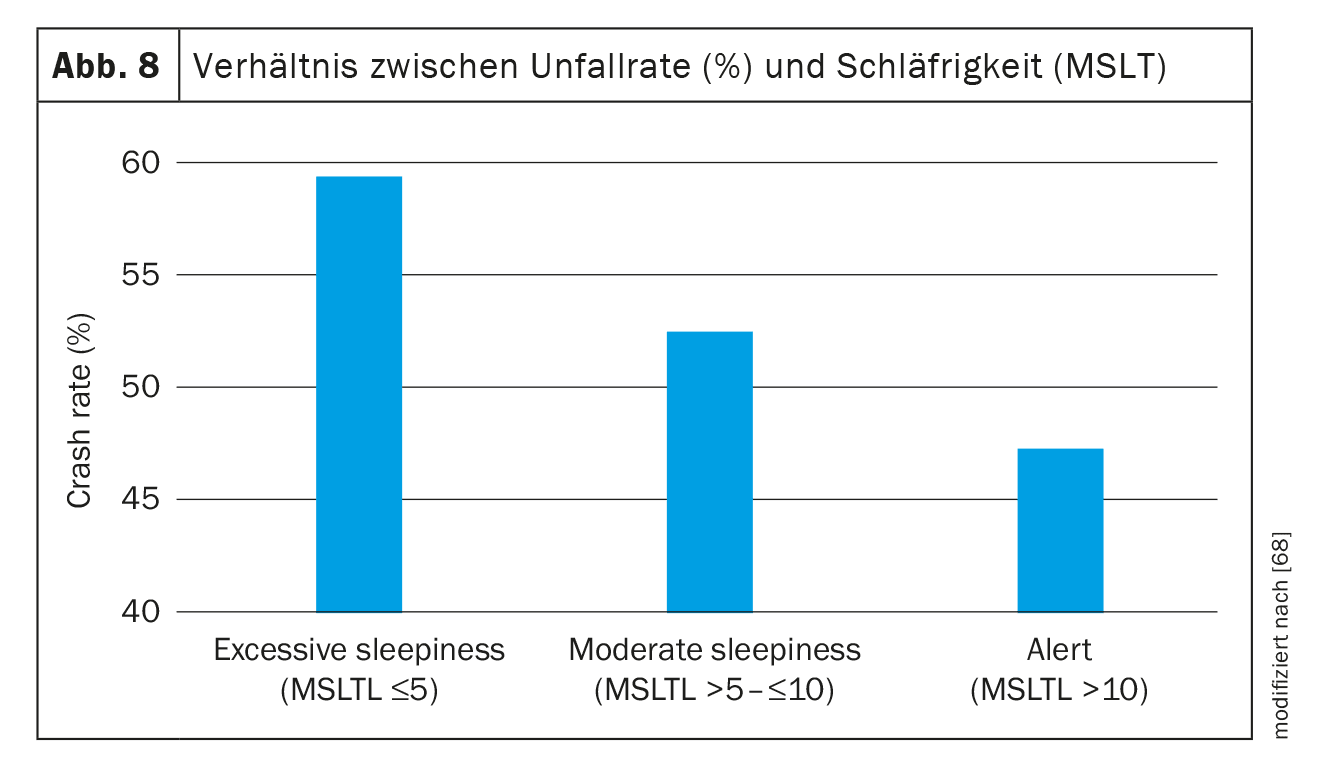
In a study of 618 participants from the general population, the participants were divided into three groups based on their sleep onset latency in the MSLT as follows: excessive sleepiness (sleep onset time 0.0-≤5 min, n=69), moderate sleepiness (sleep onset time 5.0-≤10.0 min, n=204) and awake/attentive sleep onset latency (>20.0 min., n=345). The number of accidents in the past 10 years was determined. There was a clear relationship between the sleep onset latency and the accident rate. This amounted to 59.4% for subjects with excessive sleepiness, 52.9% for moderate sleepiness and 47.3% for awake or alert subjects. Subjects with excessive sleepiness therefore had a significantly higher accident rate compared to those with normal sleep latencies. The same could be proven for the proportion of accidents with serious injuries. This was significantly higher with excessive daytime sleepiness than with normal sleep onset latency (4.3% vs. 0.6%, p=0.002) (Fig. 8) [68].
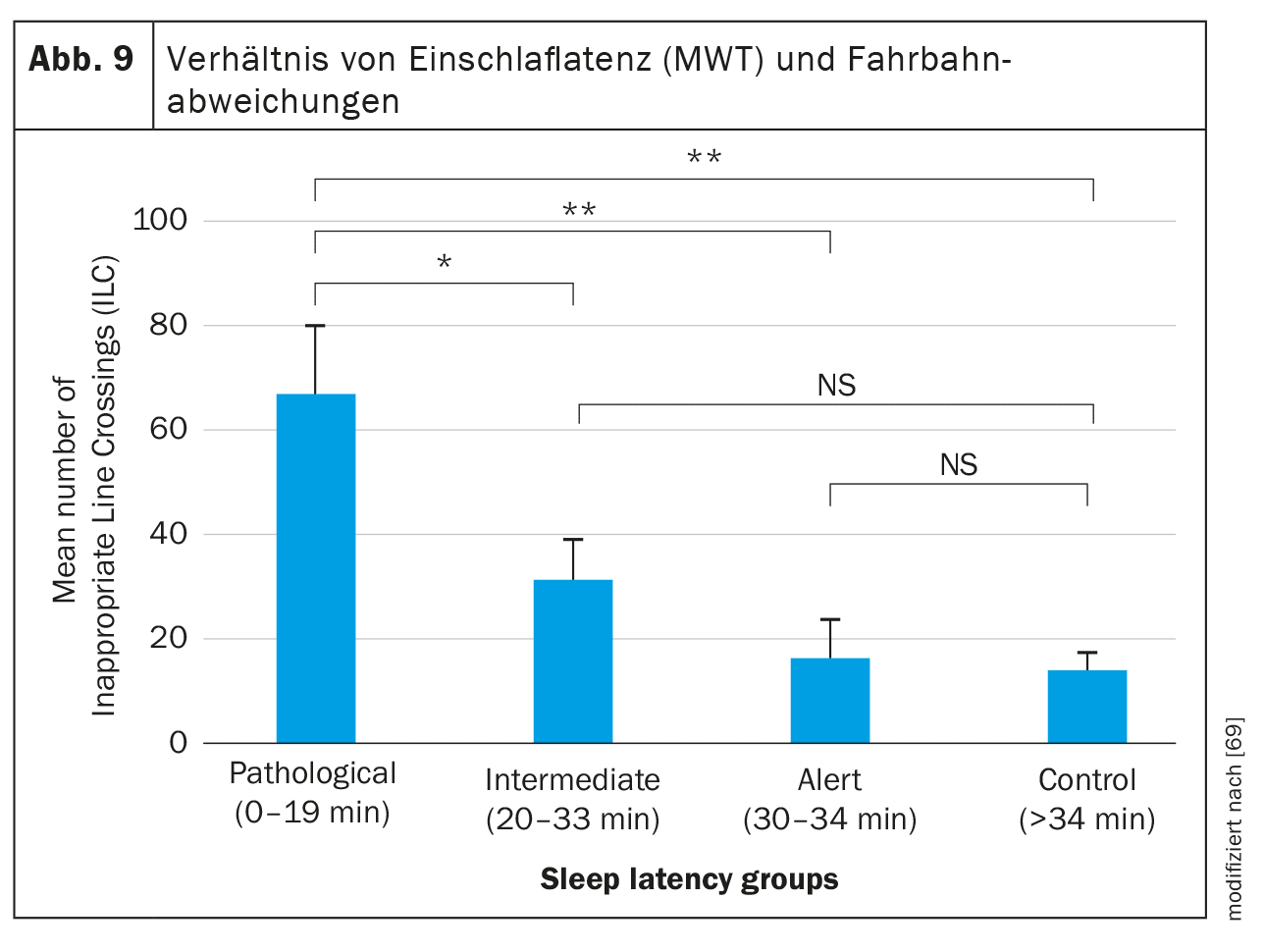
The same can be seen with regard to the MWT, in which the patient/subject is asked to stay awake for as long as possible. In a study of 19 patients with hypersomnia of central origin (9 narcolepsy, 9 idiopathic hypersomnia, 17 OSAS) and 19 healthy subjects, the patients with pathological MWT sleep latencies (0-19 min.) had significantly more lane deviations (classic sign of drowsiness at the wheel) in the driving simulation than patients with sleep latencies between 20 and 33 min. and 34-40 min. or the control subjects (p<0.001) (Fig. 9) [69].
Comparable results were found in a 2021 study. The study examined 176 patients with sleep disorders (OSAS, idiopathic hypersomnia, narcolepsy, restless legs syndrome, non-restorative sleep). 74 patients reported a sleepiness-related (near) accident in the previous year, 102 patients denied such an event. Of the patients with a (near) accident event, 37.5% reported experiencing drowsiness while driving at least once a week, while 8.8% of patients without accidents reported this symptom. There was a significant relationship between the relative risk of causing a (near) accident and MWT latencies. For patients with sleep onset latencies between 19 and 33 minutes, the relative risk was 3.2 (1.5-6.8), p<0.0001. For sleep onset latencies below 19 minutes, the relative risk was 5.5 (2.2-13.8), p=0.003 compared to sleep onset latencies above 33 min. significantly increased [70].
Neuropsychological examination methods
The neuropsychological examination methods record the attention components that are relevant when driving a motor vehicle. These include: simple attention, vigilance, sustained attention and divided attention.
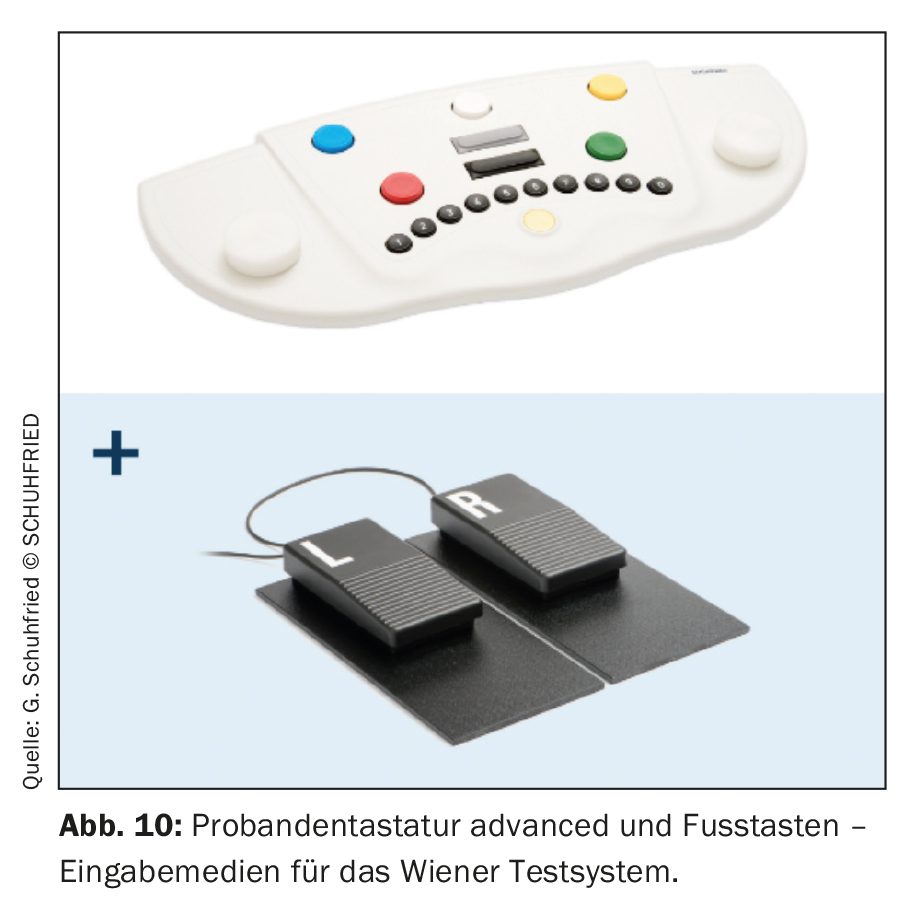
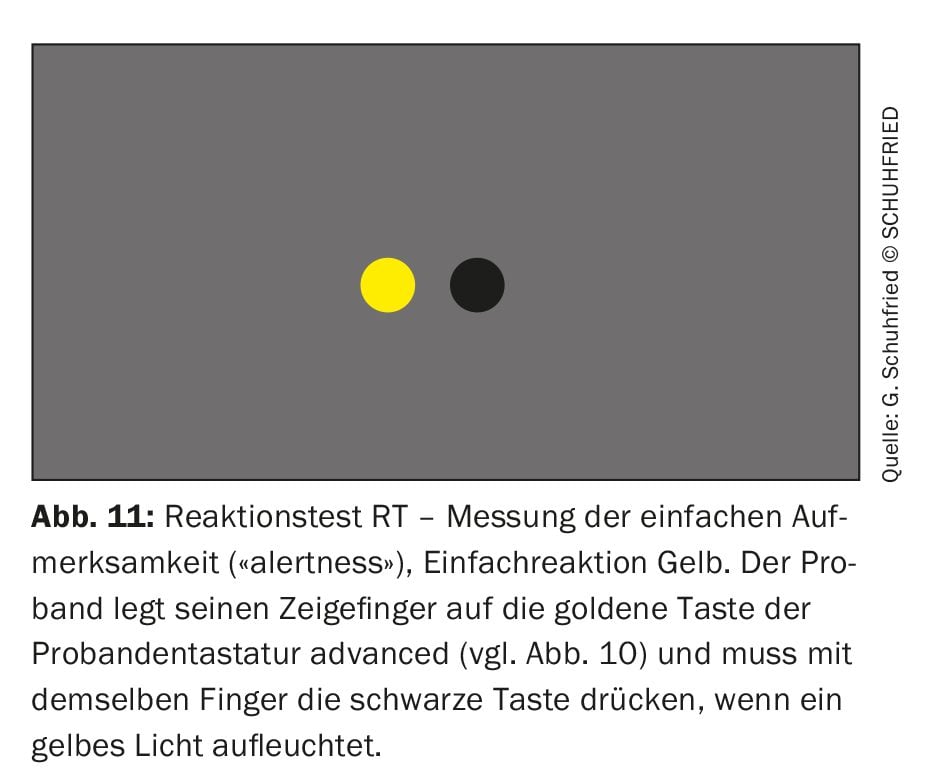
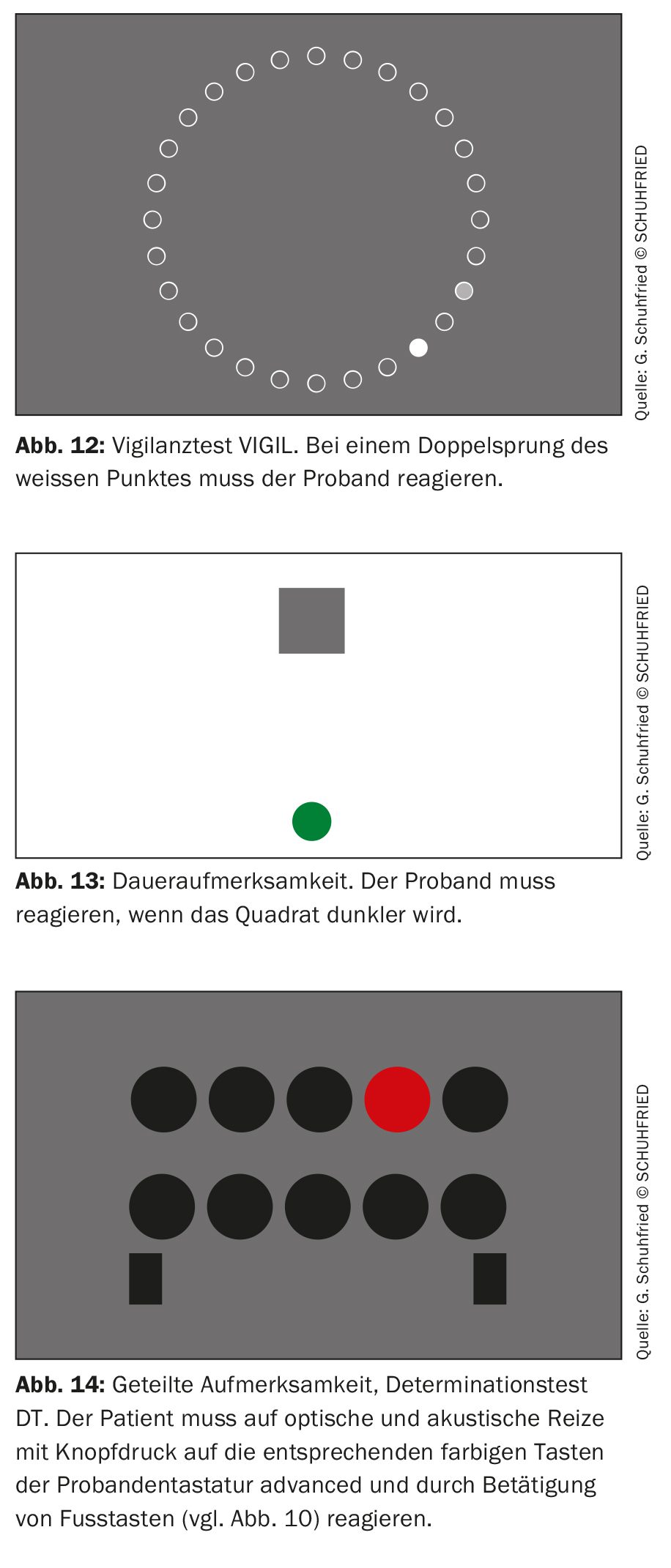
Tests of simple attention (“alertness”) are reaction time measurements. This means that the respondent must react immediately to a simple stimulus. A suitable test instrument for this is the Vienna Test System (Fig. 10 + 11). Vigilance is the long-term (at least >30 min.) maintenance of attention in monotonous environmental conditions. The VIGIL ( Mackworth Clock) vigilance test is suitable for testing vigilance (Fig. 12 ). Sustained attention is the long-term (at least >30 min.) maintenance of attention in non-monotonous environmental conditions. Figure 13 shows a test to measure sustained attention. Divided attention is serial and parallel information processing. In these test procedures, the test person must react to relevant stimuli from different stimulus sources (visual, acoustic) (e.g. buttons and foot pedals) (Fig. 14).
Recommendations of the German Social Accident Insurance (DGUV): Driving, controlling and monitoring activities (formerly G 25).
The DGUV recommends the following step-by-step procedure as a suitability test for employees who carry out driving, controlling and monitoring activities [71]:
Stage 1: Medical history
In addition to a general medical history ([Dauer-]medication, diabetes mellitus, cardiovascular disorders, balance disorders, neurological and mental disorders), the presence of sleep-related breathing disorders (SBAS) is already asked about in stage 1. The presence of SBAS is suspected if the patient has a BMI >30 kg/m2, existing cardiovascular disease or COPD. If these factors are present, the probability of SBAS is high.
Stage 2: extended anamnesis
The respondent answers the questions in the Epworth Sleepiness Scale about the probability of falling asleep in the situations mentioned there [10]. In addition, a personal medical history is taken, which includes the following questions:
- Do you snore frequently (almost every night or more than 3× per week) or does your partner report it?
- Do you have breathing interruptions or does your partner report them?
- Do you suffer from drowsiness during the day (do your eyes close, do you fall asleep unintentionally?)
- Have you ever fallen asleep at work? Have you ever fallen asleep at the wheel?
According to the recommendations of the DGUV, the results of stage 2 are interpreted as follows:
- ESS ≥11& -> urgent V.a. pathological daytime sleepiness
- Question 3 or 4 with yes -> V.a. daytime sleepiness
- Question 1 and 2 with yes -> V.a. sleep apnea
- If the answers to questions 3 and 4 are “yes”, then according to the DGUV, V.a. daytime sleepiness$ exists.
& Authors’ note: An ESS score ≥10 already indicates manifest pathological sleepiness.
$ Authors’ note: If questions 3 and 4 are answered with “yes”, this is manifest, pathological daytime sleepiness.
Stage 3: Clinical examinations
In the case of breathing-related sleep disorders with daytime sleepiness identified in the medical history -> further sleep medical clarification. In the case of daytime sleepiness§ without breathing-related sleep disorders -> immediate further specialist diagnostics.
§ The term “breathing-related sleep disorders” is misleading. It should be replaced by the term “sleep-related breathing disorders”.
Stage 4: Follow-up examination
The procedure here is the same as for level 1.
Outlook
Although the significance of daytime sleepiness in terms of causing accidents, some of them catastrophic and resulting in significant fatalities, has been known for a long time, the measures taken to date to prevent accidents, as described above, often do not appear to have any far-reaching or long-term effect. Many campaigns have attempted to sensitize the population to this issue, but the “hard figures” on the subject of “drowsiness/OSAS and accident risk” show, on the contrary, no change or even an increase in drowsiness-related accidents over the past decade.
So what can we do to make the knowledge of this danger as accessible as possible to a wider group? Three factors are decisive here. These are: Prevention, education and awareness-raising.
With regard to prevention, it would be desirable for every new driver’s license applicant or person applying for a renewal to be asked about drowsiness when driving a vehicle. Here, the personal medical history can be supplemented by standardized questionnaires. For the sake of simplicity, such an interview and/or the completion of a standardized questionnaire (e.g. Epworth Sleepiness Score, or STOP-Bang) [10,30] could take place, for example, when applying for a driving license or renewal at the traffic authority.
If there are indications of drowsiness on the basis of the questioning, the family doctor, for example, should arrange for a so-called “non-laboratory monitoring” examination to check whether OSAS may be the cause and determine the further procedure (e.g. sleep laboratory examination). When renewing a driver’s license, the applicant should be asked again about drowsiness and, if necessary, undergo the procedure described.
The second key factor that can help prevent accidents caused by drowsy driving is education. Driving schools, for example, could implement a module entitled “Drowsiness at the wheel – what to do?” in the theoretical part of training.
Ultimately, however, the police and assessors also need to be made more aware of drowsiness as a cause of accidents. The situations in which drowsiness should be considered as a cause when recording accidents are Rear-end collisions, accidents involving lane departure, accidents under monotonous environmental conditions, accidents at night, accidents without a passenger, and accidents in which no avoidance reactions (such as braking lanes or evasive maneuvers) are evident [4]. The police, who record the accident, are primarily responsible for this. Here too, a module on “drowsiness and accidents”, ideally presented by a sleep or traffic physician, could be integrated into the training.
Take-Home-Messages
- Drowsiness while driving is the main cause of accidents. This applies to both professional drivers and car drivers.
- Obstructive sleep apnoea syndrome is the most common cause of drowsiness at the wheel. Despite numerous campaigns on the subject of “drowsy driving”, the statistics show a renewed increase in accidents caused by drowsiness since 2014, at least in Germany, following a temporary drop.
- The EU bus campaign had the most significant influence on the EU directive on the issue of issuing or renewing driving licenses for driving license applicants with drowsiness or obstructive sleep apnoea syndrome. The instructions of the EU directive were implemented in all EU countries by the end of 2016.
| Declaration Articles by the authors Orth and Rasche on the above topic have been published in the following journals: – Atemwegs- und Lungenkrankheiten, 2016 – Zeitschrift für Verkehrssicherheit, 2022 |
Literature:
- Haraldsson PO, et al: Drowsiness – greater traffic hazard than alcohol. Causes, risks and treatment. Lakartidningen 2001; 98(25): 3018-3023.
- Federal Statistical Office, as of March 26, 2023.
- Peter H, et al. (Eds.): Encyclopedia of Sleep Medicine. Springer, Heidelberg 2007.
- Morsy NE, et al: Obstructive sleep apnea: personal, societal, public health, and legal implications. Rev Environ Health 2019; 34(2): 153-169; doi: 10.1515/reveh-2018-0068.
- 1st guiding principle – BGH, decision of 18.11.1969 – 4 StR 66/69 2018.
- Wise MS: Objective measures of sleepiness and wakefulness: application to the real world? J Clin Neurophysiol 2006; 23(1): 39-49; doi: 10.1097/01.wnp.0000190416.62482.42.
- Connor J, et al: Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ 2002; 324(7346): 1125; doi: 10.1136/bmj.324.7346.1125.
- Karimi M, et al: Impaired vigilance and increased accident rate in public transport operators is associated with sleep disorders. Accid Anal Prev 2013; 51: 208-214; doi: 10.1016/j.aap.2012.11.014.
- Sabil A, et al: Risk factors for sleepiness at the wheel and sleep-related car accidents among patients with obstructive sleep apnea: data from the French Pays de la Loire Sleep Cohort. Nat Sci Sleep 2021; 13: 1737-1746; doi: 10.2147/NSS.S328774.
- Johns MW: A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14(6): 540-545; doi: 10.1093/sleep/14.6.540.
- Philip P, et al: Self-reported sleepiness and not the apnoea hypopnoea index is the best predictor of sleepiness-related accidents in obstructive sleep apnoea. Sci Rep 2020; 10(1): 16267; doi: 10.1038/s41598-020-72430-8.
- Howard ME, et al: Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med 2004; 170(9): 1014-1021; doi: 10.1164/rccm.200312-1782OC.
- Carter N, et al: Sleep debt, sleepiness and accidents among males in the general population and male professional drivers. Accid Anal Prev 2003; 35(4): 613-617; doi: 10.1016/s0001-4575(02)00033-7.
- Pérez-Chada D, et al: Sleep habits and accident risk among truck drivers: a cross-sectional study in Argentina. Sleep 2005; 28(9): 1103-1108; doi: 10.1093/sleep/28.9.1103.
- Souza JC, et al: Sleep habits, sleepiness and accidents among truck drivers. Arquivos de Neuro-Psiquiatria 2005; 63: 925-930; doi: 10.1590/s0004-282×2005000600004.
- Vennelle M, et al: Sleepiness and sleep-related accidents in commercial bus drivers. Sleep and Breathing 2010; 14(1): 39-42; doi: 10.1007/s11325-009-0277-z.
- Akkoyunlu ME, et al: Investigation of obstructive sleep apnea syndrome prevalence among long-distance drivers from Zonguldak, Turkey. Multidisciplinary Respiratory Medicine 2013, 8(1): 10;
doi: 10.1186/2049-6958-8-10. - Catarino R, et al: Sleepiness and sleep-disordered breathing in truck drivers. Risk analysis of road accidents. Sleep and Breathing 2014; 18: 59-68; doi: 10.1007/s11325-013-0848-x.
- 19 Netzer NC, et al: Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999; 131(7): 485-491; doi: 10.7326/0003-4819-131-7-199910050-00002.
- Özer C, et al: Daytime sleepiness and sleep habits as risk factors of traffic accidents in a group of Turkish public transport drivers. International Journal of Clinical and Experimental Medicine 2014; 7(1): 268-273.
- Stevenson MR, et al: The role of sleepiness, sleep disorders, and the work environment on heavy-vehicle crashes in 2 Australian states. American Journal of Epiemiology 2014; 179(5): 594-601; doi: 10.1093/aje/kwt305.
- Ebrahimi MH, et al: Sleep habits and road traffic accident risk for Iranian occupational drivers. International Journal of Occupational and Medical Environmental Health 2015; 28(2): 305-312; doi: 10.13075/ijomeh.1896.00360.
- Liu Y, et al: Prevalence of obstructive sleep apnea hypopnea syndrome in professional drivers and the relationship with traffic accidents. Zhonghua Yi Xue Za Zhi 2016; 96(48): 3902-3905;
doi: 10.3760/cma.j.issn.0376-2491.2016.48.011. - 24 Girotto E, et al: Working conditions and sleepiness while driving among truck drivers. Traffic Injury Prevention 2019; 20(5): 504-509; doi: 10.1080/15389588.2019.1609670.
- 25 Alahmari MD, et al: Sleepy driving and risk of obstructive sleep apnea among truck drivers in Saudi Arabia. Traffic Injury Prevention 2019; 20(5): 498-503; doi: 10.1080/15389588.2019.1608975.
- Celikhisar H, et al: Association of presence and severity of obstructive sleep apnea syndrome with accident risk in city bus drivers. The Journal of the Pakistan Medical Association 2020; 70(12(A): 2184-2189; doi: 10.47391/JPMA.435.
- Adami A, et al: Poor performance of screening questionnaires for obstructive sleep apnea in male commercial drivers. Sleep Breath 2022; 26(2): 541-547; doi: 10.1007/s11325-021-02414-z.
- Pocobelli G, et al: Obstructive sleep apnea and risk of motor vehicle accident. Sleep Med 2021; 85: 196-203; doi: 10.1016/j.sleep.2021.07.019.
- Sebastian SK, et al: Clinical use of STOP-BANG and ESS questionnaires in the evaluation of obstructive sleep apnea-related risk factors for motor vehicle accidents among public transport drivers in Delhi, India. Sleep Breath 2021; 25(3): 1461-1466; doi: 10.1007/s11325-020-02277-w.
- Chung F, et al: STOP-Bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest 2016; 149(3): 631-638; doi: 10.1378/chest.15-0903.
- Felix M, et al: Risk of obstructive sleep apnea and traffic accidents among male bus drivers in Ecuador: Is there a significant relationship? Ann Med Surg (Lond) 2022; 74: 103296; doi: 10.1016/j.amsu.2022.103296.
- Argel M, et al: Screening for obstructive sleep apnea in truck drivers. Cien Saude Colet 2023; 8(6): 1863-1872; doi: 10.1590/1413-81232023286.16022022.
- Peppard PE, et al: Increased prevalence of sleep-disordered breathing in adults. American Journal of Epidemiology 2013; 177(9): 1006-1014; doi: 10.1093/aje/kws342.
- Phillips RO, et al: Road accidents caused by sleepy drivers: Update of a Norwegian survey. Accident Analysis & Prevention 2013; 50: 138-146; doi: 10.1016/j.aap.2012.04.003.
- Garbarino S, et al: Sleep apnea, sleep debt and daytime sleepiness are independently associated with road accidents. A cross-sectional study on truck drivers. PLOs One 2016; 11(11): e0166262; doi: 10.1371/journal.pone.0166262.
- Findley LJ, et al: Driving simulator performance in patients with sleep apnea. Am Rev Respir Dis 1989; 140: 529-530; doi: 10.1164/ajrccm/140.2.529.
- Findley LJ, et al: Severity of sleep apnea and automobile crashes.
N Engl J Med 1989; 320(13): 868-869; doi: 10.1056/nejm198903303201314. - Langwieder K: Structure of accidents with fatalities on highways in the Free State of Bavaria in 1991: a contribution to the analysis of accidents. HUK Association 1994.
- Statista 2023.
- Barbé F, et al. with the Technical Collaboration of MARIA de LLUC: (1998): Automobile accidents in patients with sleep apnea syndrome. An epidemiological and mechanistic study. Am J Respir Criti Care Med 1998; 158: 18-22; doi: 10.1164/ajrccm.158.1.9709135.
- Young T, et al: Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep 1997; 20(8): 608-613; doi: 10.1093/sleep/20.8.608.
- Terán-Santos J, et al: The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander.
N Engl J Med 1999; 340(11): 847-851; doi: 10.1056/NEJM199903183401104. - Lloberes P, et al: Self-reported sleepiness while driving as a risk factor for traffic accidents in patients with obstructive sleep apnea syndrome and in non-apnoeic snorers. Respiratory Medicine 2000; 94(10): 971-976; doi: 10.1053/rmed.2000.0869.
- Masa JF, et al: Habitually sleepy drivers have a high frequency of automobile crashes associated with respiratory disorders during sleep. Am J Respir Crit Care Med 2000; 162(4 Pt 1): 1407-1412; doi: 10.1164/ajrccm.162.4.9907019.
- Horstmann S, et al: Sleepiness-related accidents in sleep apnea patients. Sleep 2000; 23(3): 383-389.
- Komada Y, et al: Elevated risk of motor vehicle accident for male drivers with obstructive sleep apnea syndrome in the Tokyo metropolitan area. Tohoku J Exp Med 2009; 219(1): 11-16; doi: 10.1620/tjem.219.11.
- Philip P, et al: Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Medicine 2010; 11(10): 973-979; doi: 10.1016/j.sleep.2010.07.010.
- Ward KL, et al: Excessive daytime sleepiness increases the risk of motor vehicle crash in obstructive sleep apnea. Journal of Clinical Sleep Medicine 2013; 9(10): 1013-1021; doi: 10.5664/jcsm.3072.
- Basoglu OK, et al: Elevated risk of sleepiness-related motor vehicle accidents in patients with obstructive sleep apnea syndrome: a case-control study. Traffic Injury Prevention 2014; 15(5): 470-476; doi: 10.1080/15389588.2013.830213.
- Arita A, et al: Risk factors for automobile accidents caused by falling asleep while driving in obstructive sleep apnea syndrome. Sleep and Breathing 2015; 19: 1229-1234; doi: 10.1007/s11325-015-1145-7.
- Karimi M, et al: Sleep apnea-related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish Traffic Accident Registry data. Sleep 2015; 38(3): 341-349;
doi: 10.5665/sleep.4486. - Lichtblau M, et al: Risk of sleepiness-related accidents in Switzerland: results of an online sleep apnea risk questionnaire and awareness campaigns. Frontiers in Medicine (Lausanne) 2017; 4; doi: 10.3389/fmed.2017.00034.
- Matsui K, et al: Insufficient sleep rather than the apnea-hypopnea index can be associated with sleepiness-related driving problems of Japanese obstructive sleep apnea syndrome patients residing in metropolitan areas. Sleep Medicine 2017; 33: 19-22; doi: 10.1016/j.sleep.2016.07.022.
- Purtle MW, et al: Driving with undiagnosed obstructive sleep apnea (OSA): High prevalence of OSA risk in drivers who experienced a motor vehicle crash. Traffic Inj Prev 2020; 21(1): 38-41; doi: 10.1080/15389588.2019.1709175.
- Cheng AC, et al: Effect of obstructive sleep apnea on the risk of injuries-a nationwide population-based cohort study. Int J Environ Res Public Health 2021; 18(24): 13416; doi: 10.3390/ijerph182413416.
- Fanfulla F, et al: Determinants of sleepiness at wheel and missing accidents in patients with obstructive sleep apnea. Front Neurosci 2021; 15: 656203; doi: 10.3389/fnins.2021.656203.
- Udholm N, et al: Obstructive sleep apnea and road traffic accidents: a Danish nationwide cohort study. Sleep Med 2022; 96: 64-66; doi: 10.1016/j.sleep.2022.04.003.
- Luzzi V, et al: Correlations of obstructive sleep apnea syndrome and daytime sleepiness with the risk of car accidents in adult working population: a systematic review and meta-analysis with a gender-based approach. J Clin Med 2022; 11(14): 3971; doi: 10.3390/jcm11143971.
- Goncalves M, et al: Sleepiness at the wheel across Europe: a survey of 19 countries. Journal of Sleep Research 2015; 24(3): 242-253; doi: 10.1111/jsr.12267.
- Goncalves M, et al: Sleepiness at the wheel across Europe: a survey of 19 countries. J Sleep Res 2015; doi: 10.1111/jsr.12267.
- 61 COMMISSION DIRECTIVE 2014/85/EU of 1 July 2014 amending Directive 2006/126/EC of the European Parliament and of the Council on driving licenses.
- Federal Highway Research Institute (BaSt) Assessment guidelines on fitness to drive. Reports of the Federal Highway Research Institute (status: 1.6.2022).
- Posner M, Rafal R: Cognitive theories of attention and the rehabilitation of attentional deficits. In: Meier, M./Benton, A./Diller, L. (eds.): Neuropsychological Rehabilitation, Churchil Livingstone, Edinburgh 1987, 182-201.
- Weeß HG, et al: Vigilance, propensity to fall asleep, sustained attention, sleepiness, drowsiness – The measurement of sleepiness-related processes in hypersomnia – Theoretical foundations. Somnology 1998; 2(1): 32-41.
- Carskadon MA, et al: Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep 1986; 9(4): 519-524; doi: 10.1093/sleep/9.4.519.
- Wikipedia(https://de.wikipedia.org/wiki/Multipler_Schlaflatenz
test); last accessed: 23.07.2024. - Littner MR, et al: Standards of Practice Committee of the American Academy of Sleep Medicine. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 2005; 28(1): 113-121; doi: 10.1093/sleep/28.1.113.
- Drake C, et al: The 10-year risk of verified motor vehicle crashes in relation to physiologic sleepiness. Sleep 2010; 33(6): 745-752; doi: 10.1093/sleep/33.6.745.
- Philip P, et al: Maintenance of Wakefulness Test scores and driving performance in sleep disorder patients and controls. Int J Psychophysiol 2013; 89(2): 195-202.
- Philip P et al: Maintenance of wakefulness test: how does it predict accident risk in patients with sleep disorders? Sleep Medicine 2021; 77: 249-255; doi: 10.1016/j.sleep.
- DGUV recommendations for occupational health consultations and examinations. Gentner 2022.
InFo PNEUMOLOGY & ALLERGOLOGY 2024; 6(3): 6-21