Genodermatoses are diseases of the skin and its appendages resulting from mutation of a single gene and inherited according to Mendelian rules. These hereditary skin conditions are often not apparent at birth, but develop in the first months or years of life, in adolescence, or even in adulthood. Prof. Dr. Peter Itin, Chief Physician of the Dermatological University Clinic Basel, spoke about four of the five most frequently occurring genodermatoses in practice at the 6th Zurich Dermatological Training Days 2016.
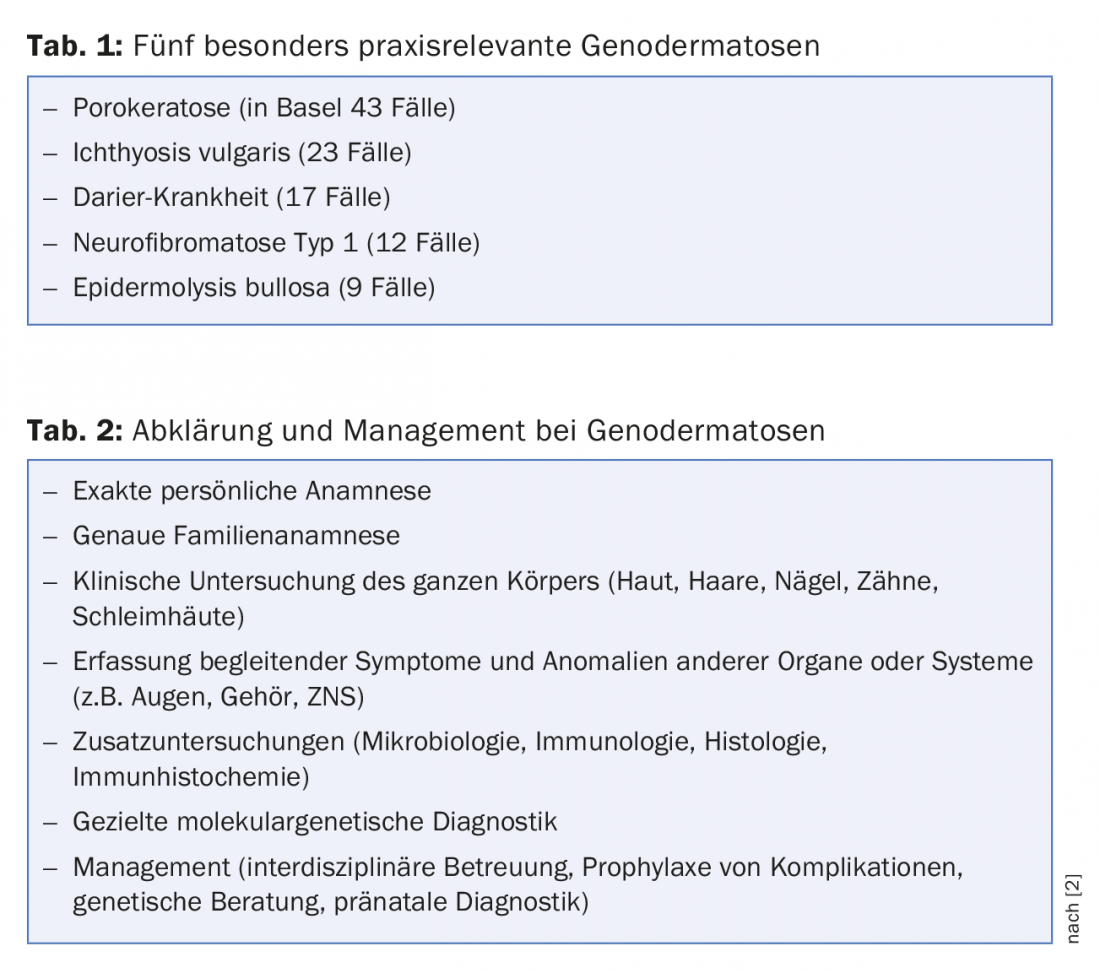
The skin is not only affected in the more than 500 known genodermatoses, but is also involved in one third of the total 10,000 known monogenic hereditary diseases, which can manifest in various organs. Physicians in practice should be aware of the five most common genodermatoses, which account for 91% of monogenic skin diseases encountered in practice [1]. Based on an analysis of the diagnoses of outpatient consultations in the Dermatological University Clinic Basel, in the period from 2002 to 2008, a list of the five most frequent genodermatoses could be compiled (Table 1). Table 2 gives an overview of diagnostic clarification steps.
Genodermatoses groups
Hereditary keratinization disorders, which include porokeratosis, ichthyosis vulgaris, and Darier’s disease, account for about half of genodermatoses [1]. All hereditary cornification disorders are based on either a protein or lipid disorder, with a mismatch of epithelial proliferation and desquamation. Other groups of genodermatoses include, in order of decreasing frequency [1]:
- Genodermatoses with benign tumors (in the foreground neurofibromatosis type 1 and tuberous sclerosis).
- Hereditary epidermolysis (Epidermolysis bullosa)
- Hereditary metabolic disorders (e.g., porphyria cutanea tarda, hereditary angioneurotic edema).
- Genodermatoses with malignant tumors
- Hereditary connective tissue diseases
- Hereditary pigment disorders
- Hereditary diseases of nails and hair
- Ectodermal dysplasias
Porokeratosis
This genodermatosis, most commonly diagnosed in Basel, can be diffuse or segmental, often with a distribution along the Blaschko lines. Characteristic is the corneal lamella, whereby the finger gets stuck when passing over it (histopathological correlate: parakeratotic flag). Inheritance is autosomal dominant. Genes whose mutations can cause porokeratosis include the gene SLC17A9, which is important for transmembrane protein transport, and the gene PMVK, which is important for cholesterol synthesis. Patients with porokeratosis have a higher incidence of squamous cell carcinoma.
Ichthyosis vulgaris
The frequency of autosomal-dominant inherited ichthyosis vulgaris is 1:300 to 1:1000. This hereditary cornification and barrier disorder is based on a filaggrin mutation that leads to abnormal keratohyaline granules. It is not until the third to sixth month of life that this genodermatosis becomes noticeable with xerosis, scaling and pruritus. The scaling is variably pronounced, often only in winter when the indoor air is dry during the heating season. Typically, the flexures (elbow, poplitea) are left out. Hand lines are accentuated and in half of the cases there is an association with atopic dermatitis. Therapeutically, the focus is on greasing the skin, especially overnight. Dandruff can be removed with preparations containing urea. In the case of painful fissures, glycerin-containing topicals are suitable for treatment, and in the case of a keratoderm, salicylaseline 20%. Pruritus can be relieved with mentholated, cooling preparations. For severe erythema, topical corticosteroids used in the short term help. As for anhidrosis, cooling vests are useful for athletes.
Darier’s disease
Dyskeratosis follicularis Darier is the second most common keratinization disorder. Responsible for this genodermatosis is an autosomal-dominant inherited mutation of the ATP2A2 gene, which codes for a calcium pump. Truncal dirty-brownish papules are found, also palmar pits, follicular keratoses, nail changes (leukonychia, peripheral usures), palmoplantar keratoderm – typical hemorrhages in the palms. On inspection of the oral mucosa, which should be part of the clinical examination in all patients, the cobblestone relief of the gingiva is striking. The congenital form of Darier’s disease is rare. Most often, genodermatosis is not marked until after puberty. Palmare pits, however, are present in children as young as about five years old. Neuropsychiatric disorders are associated but not mandatory in Darier’s disease.

Neurofibromatosis type 1 (NF1)
This autosomal dominant hereditary disease occurs at a frequency of 1:3000. In half of those affected, NF1 is not yet known in the family (new mutation). Loss of the tumor suppressor neurofibromin due to mutation of the neurofibromin gene on chromosome 17 causes an increased risk of benign and malignant tumors [3]. When the diagnosis is made, an optic glioma should be sought by MRI of the skull. NF1 is a complex physical and often motor and cognitive developmental disorder. Complications shorten the life expectancy of affected individuals by 15 years. Typical café-au-lait spots are not infrequently present at birth or develop during the first two years of life. One to two of these spots are found in 10% of the general population [3]. If there are six or more of these spots (Table 3), the speaker said, NF1 should be considered and a thorough full-body pediatric examination should be performed.
Source: 6th Zurich Dermatology Training Days, June 15-17, 2016.
Literature:
- Itin P, et al: Genodermatoses the practitioner needs to know. Dermatologist 2013; 64: 26-31.
- Has C, et al: Practical aspects of molecular diagnostics in genodermatoses. Dermatologist 2016; 67: 53-58.
- Ferner RE, et al: Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet 2007; 44: 81-88.
DERMATOLOGIE PRAXIS 2016; 26(4): 44-45











