Psoriatic arthritis (PsA) manifests clinically as a heterogeneous disease with phenotypically highly variable expression. Most of those affected already suffer from skin psoriasis. Predicting which psoriasis patients are at increased risk for developing joint involvement is proving difficult, but is critical for early therapeutic intervention. These and other challenges in the management of PsA were discussed from an interdisciplinary perspective at the World Psoriasis & Psoriatic Arthritis Congress.
Approximately 20-30% of all psoriasis patients develop psoriatic arthritis (PsA) during the course of the disease, with an average time latency of 10 years [1]. Drug treatment options for PsA have expanded significantly in the recent past, and a wide range of disease-modifying pharmacotherapies (DMARDs) are now available. Recommendations from the European League Against Rheumatism (EULAR) and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) provide guidance for selecting the appropriate treatment strategy. Despite the progress made in recent years in understanding the pathophysiology and treatment options of PsA, there are still many unanswered questions. According to a review published in 2020, current disease-modifying antirheumatic drugs achieve an ACR20 response in 40-60% of patients, meaning that over 40% of patients do not show a sufficient response [2]. As part of the triennial World Psoriasis & Psoriatic Arthritis Congress, Christopher T. Ritchlin, MD, MPH, University of Rochester (USA), reported on current challenges in the management of psoriatic arthritis (PsA) [11].
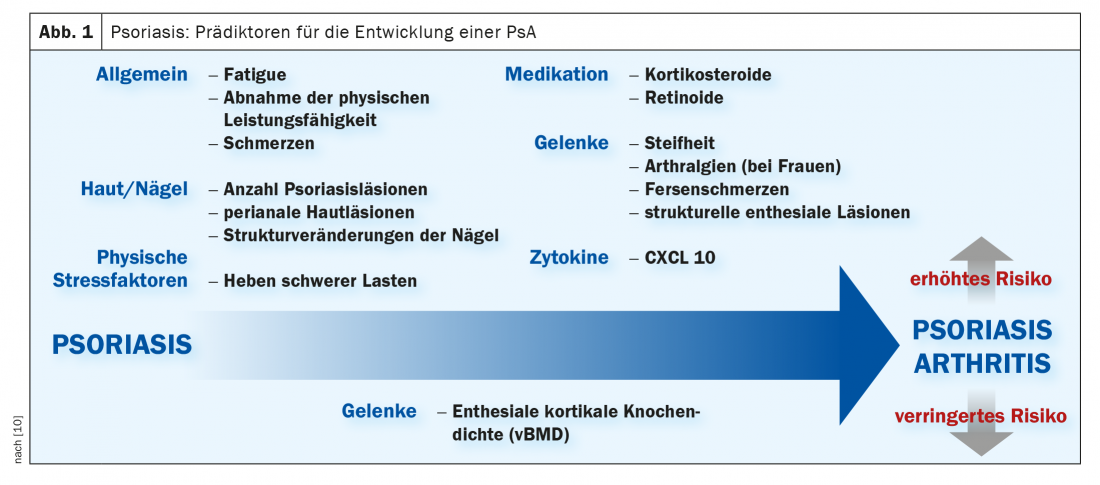
What are predictors of the development of PsA?
Predicting which psoriasis patients are at increased risk for developing PsA has proven difficult to date, but there are numerous research initiatives addressing issues related to this. Among other things, there is evidence that high disease activity of skin psoriasis is a risk factor for the development of PsA [3,4]. The PAMPA project (Preventing Arthritis in a Multi-center Psoriasis At-risk Population) was launched to identify specific predictors of psoriasis patients at increased risk for progression to PsA [5]. The focus is on the study of clinical, genetic, immunological and environmental markers. Although there are already isolated findings on biomarkers such as Mulder et al. reveal in a Systematic Review to be published in 2021. According to this, the cytokine CXCL10 has a positive predictive value for the development of PsA in psoriasis patients (Fig. 1) . But further studies are needed to find out more details. DUET” (“Diagnostic Ultrasound Enthesitis Tool”), a subproject of the GRAPPA initiative [6], is concerned with the development of a sonographic tool for early diagnosis of PsA.
In the focus of research: Tissue-resident memory T cells.
Deciphering the pathophysiology enables the identification of new targets for pharmacotherapies. In one study, tissue-resident memory T cells (TRMs) were detected in the synovium of patients with psoriatic arthritis. These are thought to play an important role in disease recurrence [7]. Therefore, a better understanding of the pathophysiologically relevant tissue-resident memory T cells is among an important approach to drive advances in the field of pharmacotherapy for PsA. Memory cells remain in the body for years after a disease has subsided and form the “immunological memory”. In an autoimmune disease, however, the immune system is unable to distinguish foreign pathogens from its own tissue: the body’s own structures are mistakenly identified by the immune system as foreign bodies. The pathogenic memory cells are repeatedly activated, which has an unfavorable effect on a chronic inflammatory disease such as psoriatic arthritis.
|
New GRAPPA recommendations The multidisciplinary international expert forum GRAPPA (“Group for Research and Assessment of Psoriasis and Psoriatic Arthritis”) regularly issues revised recommendations for the management of PsA, taking into account new scientific findings on therapeutic options. The release of the most current new edition is planned for 2021. |
Obese patients: Lifestyle program for weight reduction
Obesity is more prevalent in patients with psoriatic arthritis than in the general population and is associated with increased disease activity, decreased treatment response, and increased cardiovascular risk. That a reduction in body weight in overweight PsA patients under constant baseline therapy contributes to a reduction in disease activity was shown in a study by Klingberg et al. could be demonstrated [8]: At baseline, the mean BMI was 35.2 kg /m2. After a change in diet over the period of 12 to 16 weeks, an average weight reduction of 18.7 kg was achieved. This weight reduction was accompanied by significant improvements in several disease-related parameters, including joint index, CRP, enthesitis index, Health Assessment Questionnaire Disability Index (HAQ), and patient-oriented indices such as global health, pain, and fatigability. The improvement concerning ACR 20, 50, and 70, respectively, was 51.2% (n=21), 34.1% (n=14), and 7.3% (n=3).
Congress: World Psoriasis & Psoriatic Arthritis Conference 2021
Literature:
- Mulder MLM, et al: Clinical, laboratory, and genetic markers for the development or presence of psoriatic arthritis in psoriasis patients: a systematic review. Arthritis Res Ther 2021; 23: 168.
- Ritchlin CT, et al: Moving Toward Precision Medicine in Psoriasis and Psoriatic Arthritis. The Journal of Rheumatology Supplement June 2020; 96: 19-24.
- ASPAT/ÖGR: Peripheral Spondyloarthritis Guideline 2020, https://rheumatologie.at, (last accessed 07/03/2021).
- Busse K, Liao W: Which Psoriasis Patients Develop Psoriatic Arthritis? Psoriasis Forum 2010:16(4): 17-25.
- GRAPPA, www.grappanetwork.org (last accessed 07/03/2021).
- Ullman K: Combined Clinic, a Rheumatologist & Dermatologist See Patients Together, 2019, www.the-rheumatologist.org (last accessed July 03, 2021).
- Kirkham BM, Menon B, Taams LS: Immunological and clinical relationships of synovial IL-17+ T cells in psoriatic arthritis. ACR/ARHP Annual Meeting 2014; 633.
- Klingberg E, et al: Weight loss improves disease activity in patients with psoriatic arthritis and obesity: an interventional study. Arthritis Res Ther 2019; 21(1): 17.
- Coates LC, et al: OP0229. The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA). Treatment Recommendations 2021. annals of the Rheumatic Diseases 2021; 80: 139-140.
- Erlangen University Medical Center, Disease Patterns, Psoriasis and Joints, www.medizin3.uk-erlangen.de (last accessed 07/03/2021).
- Ritchlin CT: Unmet needs in psoriatic arthritis, Interactive discussion session, Christopher T. Ritchlin, MD, MPH, University of Rochester (USA), World Psoriasis & Psoriatic Arthritis Conference, Stockholm, July 03, 2021.
DERMATOLOGIE PRAXIS 2021; 31(4): 25-26 (published 8/19-21, ahead of print).