Nausea, reflux and other functional gastrointestinal symptoms are common in pregnancy and can often be managed with dietary or lifestyle modification. Drug interventions, although safe for mother and child, are reserved for refractory symptoms. A careful history and diagnosis are necessary for pregnancy-associated liver disease. In the case of preeclampsia, HELLP syndrome or acute fatty liver of pregnancy, delivery is the only effective therapy. Gallbladder symptoms are common in pregnancy, and cholecystectomy should be performed laparoscopically in the second trimester. In choledocholithiasis, ERCP is a justifiable form of therapy.
The majority of all pregnant women suffer from nausea and vomiting mostly during the first trimester. The extreme form of nausea and vomiting, hyperemesis gravidarum, requires active treatment to ensure the health of both mother and child. In addition, functional gastrointestinal complaints such as heartburn, reflux and constipation are very common during pregnancy. Lifestyle modifications and a change in diet are often successful as initial measures. If symptoms persist, drug therapies are necessary to improve quality of life and prevent complications. Pregnancy-associated liver diseases are complex and potentially very severe medical conditions. The spectrum ranges from biliary colic and benign intrahepatic cholestasis to life-threatening preeclampsia and HELLP syndrome, which necessitate immediate delivery. Patients and physicians are often uncertain about low-risk medications or treatment options during pregnancy. This review presents the spectrum of pregnancy-associated gastrointestinal disorders and liver diseases and their therapy.
Nausea and vomiting
50-90% of all pregnant women suffer from nausea and vomiting mostly during the first trimester [1–3]. Risk factors for nausea and vomiting in pregnancy are recognized as young age, obesity, first pregnancy, and smoking. If symptoms persist into the third trimester, other causes should be investigated. For some women, dietary changes (smaller, high-carbohydrate meals) or alternative remedies such as acupuncture or ginger are sufficient for symptom management [4]. According to recent meta-analyses, however, the efficacy of alternative healing methods is questionable [5,6]. Vomiting should be differentiated from gastroesophageal reflux and regurgitation, which patients often refer to as “vomiting,” by taking a detailed history. For reflux or regurgitation, antacids, alginates, H2 receptor blockers, or, if necessary, proton pump inhibitors (PPIs) may be effective.
The extreme form of nausea and vomiting in pregnancy is hyperemesis gravidarum; rehydrating and antiemetic therapy is indicated for weight loss and exsiccosis. Thus, rare, severe complications such as Wernicke’s encephalopathy can be prevented by thiamine deficiency [7]. For severe nausea and vomiting, antiemetics that have a low risk to the fetus when used include metoclopramide (10 mg orally, rectally – soon to be available as a nasal spray), prochlorperazine (5 mg orally), trimethobenzamine (300 mg orally), and ondansetron (4-8 mg sublingually). However, after continuous use of metoclopramide, prochlorperazine, or trimethobenzamine during pregnancy, withdrawal symptoms and extrapyramidal side effects have been observed in neonates [3,8]. Doxylamine pyridoxine (10 g) and vitamin B6 (10 g) are recommended by several guidelines as safe and effective first-line therapies and have high fetal safety [9–11].
Gastroesophageal reflux
Reflux symptoms in pregnancy are no different from symptoms of typical gastroesopahegal reflux disease. Heartburn, belching, and regurgitation occur in 30-80% of pregnant women. Often, pre-existing reflux symptoms are exacerbated by pregnancy [2,12]. Extraesophageal manifestations of reflux disease are rare in pregnancy [13]. Pathophysiologically, there is a decrease in lower esophageal sphincter pressure during pregnancy due to increased estrogen levels. In addition, there are structural changes at the gastroesophageal junction, increased intra-abdominal pressure, and gastric compression due to the enlarged uterus.
Because of the relatively short duration of reflux during pregnancy, severe complications are rare. Thus, endoscopic diagnosis is necessary only in isolated cases and only in the presence of clear alarm symptoms such as dysphagia or evidence of gastrointestinal bleeding [2,14].
Lifestyle modifications and dietary changes have great therapeutic importance in gastroesophageal reflux in pregnancy. Figure 1 summarizes a possible treatment algorithm. For mild symptoms, elevating the head of the bed, avoiding late meals, and eating smaller meals more frequently are often sufficient.
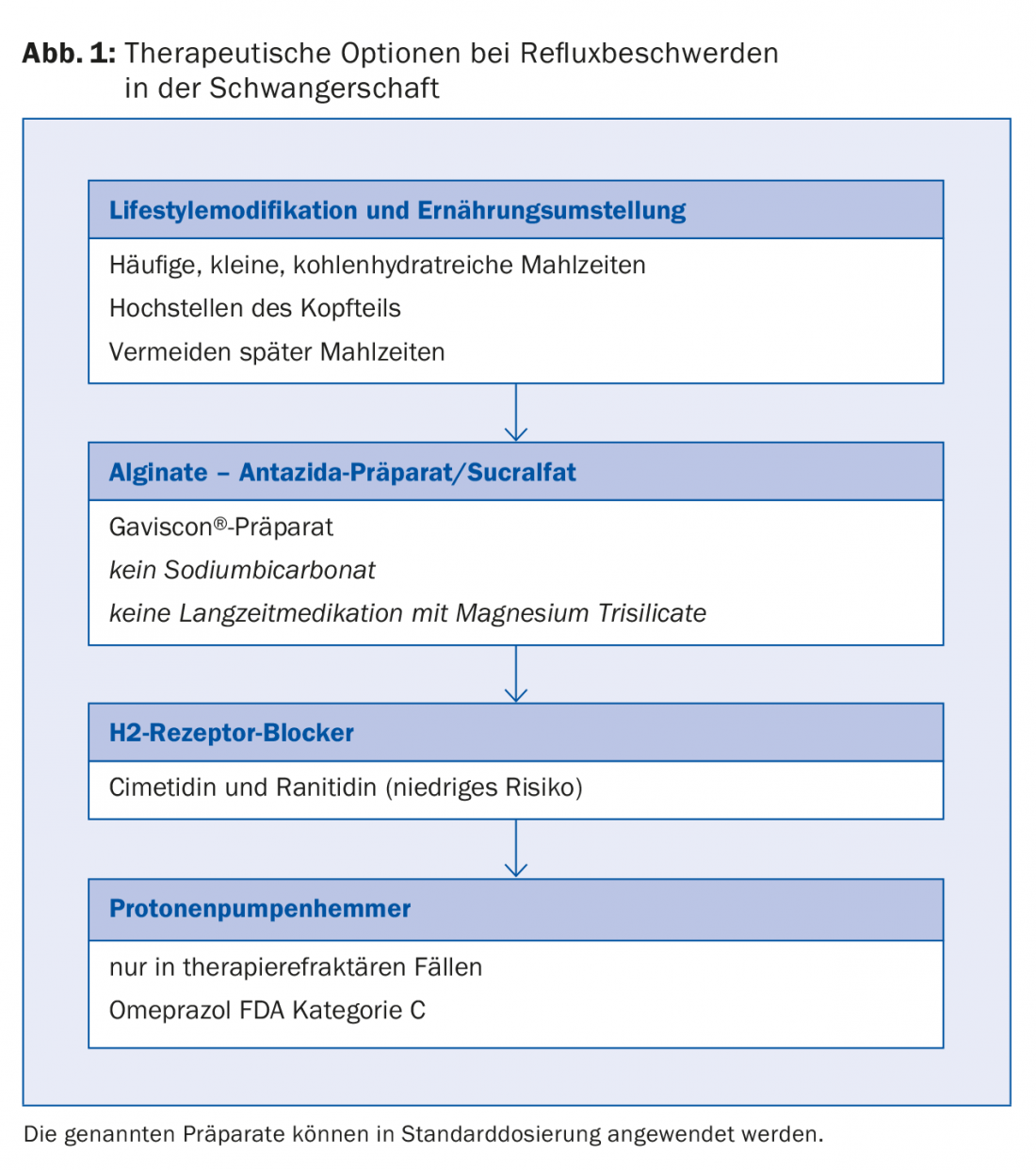
Medication should be considered for persistent, severe symptoms. Antacids may improve symptoms in the short term and have no teratogenic effects. However, sodium bicarbonate (risk of metabolic alkalosis and fluid overload) and long-term therapy with magnesium-containing preparations (risk of decreased uterine contractility) should be avoided [8]. Alginate preparations (e.g., Gaviscon® 5-10 ml after meals and before going to bed) form a viscous layer on the stomach contents, reducing acid and non-acid reflux for up to two hours. This mechanism reduced the number of reflux episodes in studies compared to conventional antacids (Alucol®) [15]. The safety and efficacy of the use of Gaviscon® during pregnancy has already been demonstrated in clinical studies [16,17]. Sucralfate is also not absorbed and, along with alginates, appears to be another first-line drug option in pregnancy, although limited data on its use are available [18–20].
If there is no response to the above measures, H2 receptor blockers may be used. Although one study reported an increased preterm birth rate with regular medication with H2 blockers, large meta-analyses were able to refute this conjecture [8,21].
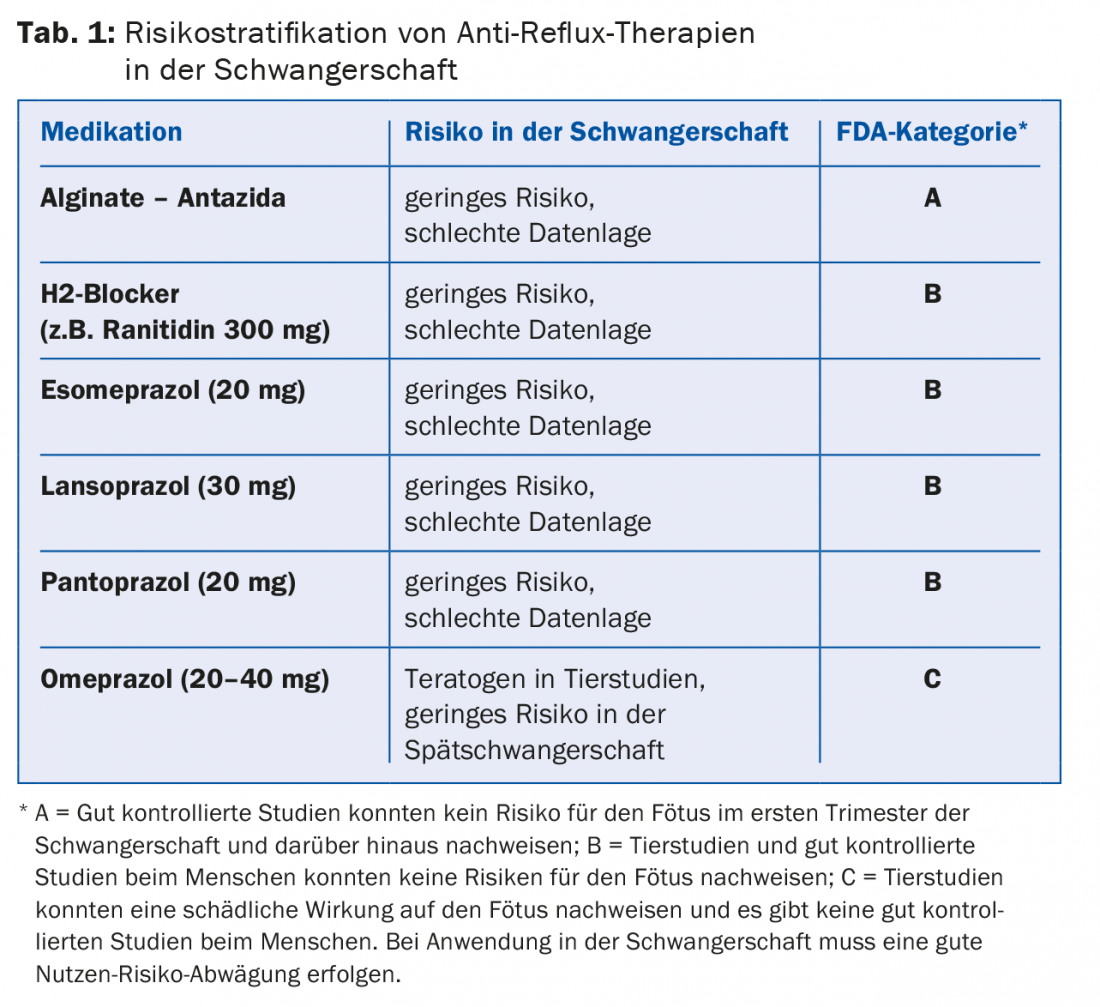
Proton pump inhibitors (PPIs) should be used only in cases of refractory symptoms, as increased embryonic mortality had been shown in animal studies at therapeutic doses of omeprazole. No relevant toxicity to the fetus has been demonstrated for esomeprazole and lansoprazole in animal studies. Prospective studies of human use are not available [3,22,23], but according to larger retrospective studies and meta-analyses, the use of omeprazole, esomeprazole, lansoprazole, and pantoprazole appears to be safe in humans during pregnancy even in the first trimester [23–29]. If PPIs are used in pregnancy, they show a good effect on reflux symptoms in many patients. Table 1 summarizes the risk stratification of the individual PPIs that can also be used in pregnancy at standard doses [3].
Flatulence, constipation and other abdominal complaints
Bloating and constipation are also common during pregnancy, occurring in 25-40% of pregnant women. These symptoms are mainly hormonal (slowing effect on gastrointestinal motility and altered water absorption). Additionally, decreased physical activity contributes to constipation [2,30,31]. Constipation in pregnancy rarely has a serious cause, yet a careful history and clinical examination are mandatory. Endoscopic workup should be considered only when alarm symptoms are present.
In this patient group, hemorrhoids are the first thing to think of when fresh blood is discharged ab ano. Anemia is very common in pregnancy and is physiological up to a hemoglobin level of approximately 105 g/l. However, a lower hemoglobin value should be clarified. Mostly it is caused by iron deficiency with ferritin <20 µ/l. In these cases, iron should be substituted [32]. In addition, folate and vitamin B12 deficiency may occur. These vitamins should also be substituted to avoid complications such as low birth weight and prematurity [33].
Pregnant women should be advised to maintain adequate fluid intake and physical activity [34]. A diet rich in fiber is equally important. Fiber-rich stool regulants are effective in pregnant women but may also increase bloating [35,36].
Only in cases of severe constipation symptoms is drug therapy indicated during pregnancy. Many drugs with prokinetic agents, such as antraquinone and castor oil, are contraindicated because of their teratogenic or labor-inducing effects. In contrast, bulking agents such as psyllium (e.g., Metamucil®) or Sterculia (e.g., Normacol®) and also osmotic laxatives such as polyethylene glycol (PEG) can be used safely in pregnancy; these appear to be effective [37].
Hemorrhoids
One third of all pregnant women suffer from symptomatic hemorrhoids. Again, stool-regulating measures and local therapies should be recommended. Scheriproct® can be used as a topical measure after the first trimester [38]. For persistent bleeding from internal hemorrhoids, rubber band ligation, infrared coagulation, or sclerotherapy during pregnancy are safe and effective [39,40].
Inflammatory bowel disease and pregnancy
Inflammatory bowel disease (IBD) includes Crohn’s disease and ulcerative colitis. With currently available therapeutic options, a good outcome of pregnancy and IBD can be expected in more than 80% of patients, especially with remission at the time of conception [41]. While the clinical course of Crohn’s disease is not affected by pregnancy, disease activity of ulcerative colitis appears to be somewhat increased during and immediately after pregnancy [41,42]. The reasons for this are unclear, but could be related to hormonal effects or smoking cessation.
Significant activity of IBD during pregnancy increases the risk of preterm birth, low birth weight, and genital blood leakage, among others [43–46].
For investigations and therapies during pregnancy, the risk of intestinal inflammation to the pregnancy must be weighed against potential risks of the therapies [41]. Endoscopy is also justifiable in pregnancy after careful consideration of the benefits and risks, whereas imaging procedures should be limited to ultrasound or MRI. 5-Aminosalicylic acid is considered a safe drug, and azathioprine should also be passed during pregnancy. Methotrexate is absolutely contraindicated due to its highly teratogenic effect. For infliximab and adalimumab, a pause in therapy during the third trimester should be considered to minimize transfer to the unborn child via the placenta. Short-term glucocorticoid administration is considered acceptable when well indicated, at least after the first trimester. In case of doubt and complicated courses, always consult with a center [41].
Gall bladder disease during pregnancy
Pregnancy, gallbladder disease prior to becoming pregnant, and obesity are risk factors for developing gallstone disease. The incidence is 0.3-0.5%, and the symptoms of biliary colic or cholecystitis are the same as in non-pregnant patients [47–49]. In the first trimester, symptomatic cholecystolithiasis should be treated conservatively with analgesics and antibiotics. Laparoscopic cholecystectomy as the surgical method of choice should be performed only in the second trimester. Several studies show that continuation of conservative therapy until delivery increases the risk of recurrence of biliary colic with complications including pancreatitis [2,50]. In cases of choledocholithiasis, endoscopic retrograde cholangiopancreatography (ERCP) is acceptable, even in pregnant women, provided that the use of ionizing radiation is minimized [50,51].
Liver diseases of pregnancy
Pregnancy-associated liver disease is described in up to 3% of all pregnancies. The individual diseases occur at different stages of pregnancy, which can facilitate diagnosis (Tab. 2) . During pregnancy, liver function and blood flow change due to hormonal influences. Gamma-glutamyltransferase (GGT) is decreased, as is albumin. Alkaline phosphatase (AP) is elevated due to the production of an isoenzyme in the placenta. In contrast, alanine transaminase (ALT) and aspartate transaminase (AST) are within the normal range during pregnancy. Any transaminase elevation should be clarified [2,52].
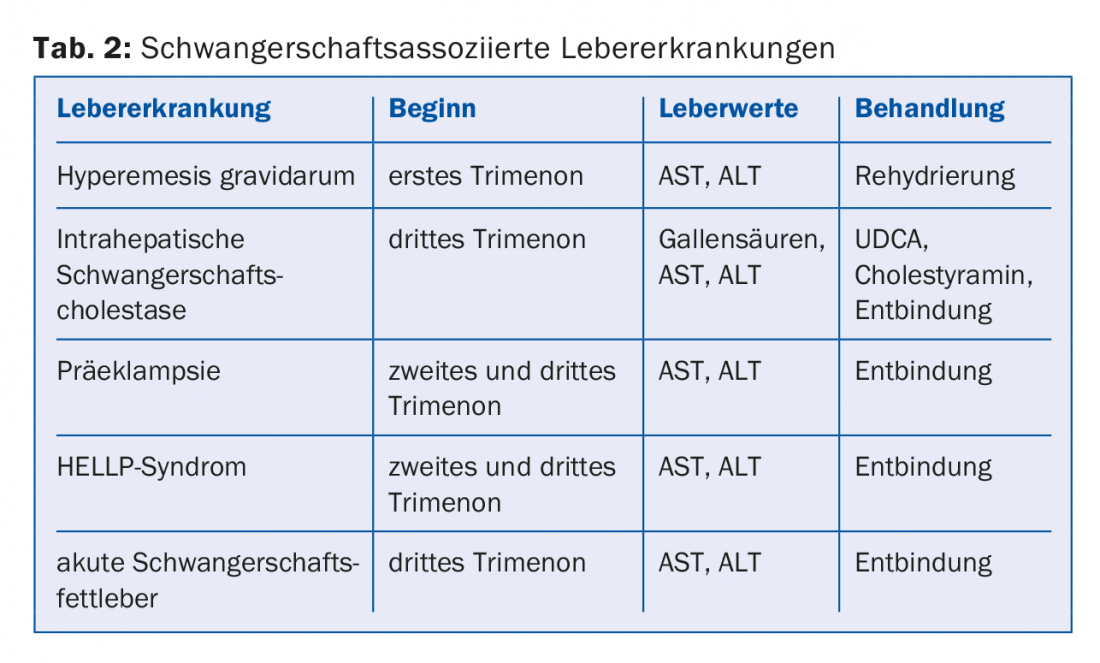
In the first trimester, hyperemesis gravidarum may explain elevated transaminases. In 70% of patients with this clinical picture, there is an increase in transaminases, which disappears after adequate rehydration. Risk factors include late-onset hyperemesis and severe ketonuria. Intrahepatic pregnancy cholestasis occurs from the 30th week of pregnancy and disappears after delivery [53]. The etiology is multifactorial and includes genetic risks and alterations in progesterone metabolism. The increase in bile acids can cause severe pruritus and jaundice. Transaminases and GGT are often normal. Gestational cholestasis is associated with prematurity and increased fetal mortality [54]. Ursodeoxycholic acid (UDCA) reduces pruritus and jaundice as does cholestyramine. Because bile acid sequestrants decrease the absorption of fat-soluble vitamins (A, D, E, K), vitamin supplementation should be considered during cholestyramine therapy [55].
Preeclampsia and HELLP syndrome
Preeclampsia accounts for more than half of all cases of elevated liver enzymes in pregnancy and occurs in 2-8% of all pregnancies, usually after 20 weeks of gestation. Hypertension, proteinuria, and edema are leading symptoms. First-time mothers, women with multiple pregnancies, and patients with pre-existing arterial hypertension or diabetes mellitus are particularly at risk [53]. A 1.5- to 5-fold increase in transaminases and mild AP elevation with normal liver function are observed in the setting of preeclampsia. Although pregnant women with preeclampsia require close monitoring and possibly antihypertensive therapy (magnesium sulfates), therapy for elevated liver enzymes is not necessary [54].
In 5-10% of patients, severe preeclampsia develops into HELLP syndrome characterized by hemolytic anemia, transaminase elevation, and thrombocytopenia. HELLP syndrome typically occurs in the second and third trimesters. However, especially in the setting of preexisting preeclampsia, HELLP syndrome may also manifest at most two days postpartum. Clinically, HELLP syndrome presents with nausea, vomiting, headache, and visual disturbances. Coagulation disorders and renal failure are often complicating factors [54]. The only effective therapy is delivery. Maternal mortality is 1-3.5%, and infant mortality is determined by gestational age at delivery [56].
Acute fatty liver of pregnancy
Acute fatty liver of pregnancy is a serious condition that occurs in the last trimester of pregnancy. A defect in the metabolism of long-chain fatty acids leads to an accumulation of the fatty acids first in the liver of the unborn child and subsequently in the liver of the mother with consecutive liver damage. Nausea, vomiting, upper gastrointestinal bleeding due to liver failure, encephalopathy, renal and multi-organ failure are part of the clinical picture of acute fatty liver of pregnancy. Delivery is also the treatment of choice in this case. In severe cases, liver transplantation is necessary in the mother. Neonatal mortality in mothers with acute fatty liver of pregnancy ranges from 20% to 60% [54].
Literature:
- Koch KL: Gastrointestinal factors in nausea and vomiting of pregnancy. Am J Obstet Gynecol 2002; 186: S198-203.
- Keller J, Frederking D, Layer P: The spectrum and treatment of gastrointestinal disorders during pregnancy. Nat Clin Pract Gastroenterol Hepatol 2008; 5: 430-443.
- van der Woude CJ, Metselaar HJ, Danese S: Management of gastrointestinal and liver diseases during pregnancy. Gut 2014; 63: 1014-1023.
- Jarvis S, Nelson-Piercy C: Management of nausea and vomiting in pregnancy. BMJ 2011; 342: d3606.
- Matthews A, et al: Interventions for nausea and vomiting in early pregnancy. Cochrane Database Syst Rev 2015; 9: CD007575.
- Van den Heuvel E, et al: Effect of acustimulation on nausea and vomiting and on hyperemesis in pregnancy: a systematic review of Western and Chinese literature. BMC complementary and alternative medicine 2016; 16: 13.
- Yahia M, et al: Wernicke’s encephalopathy: A rare complication of hyperemesis gravidarum. Anaesthesia Critical Care & Pain Medicine 2015; 34: 173-177.
- Mahadevan U, Kane S: American gastroenterological association institute medical position statement on the use of gastrointestinal medications in pregnancy. Gastroenterology 2006; 131: 278-282.
- Maltepe C, Koren G: The management of nausea and vomiting of pregnancy and hyperemesis gravidarum – a 2013 update. J Popul Ther Clin Pharmacol 2013; 20: e184-192.
- Niebyl JR, Briggs GG: The pharmacologic management of nausea and vomiting of pregnancy. J Fam Pract 2014; 63: S31-37.
- Arsenault MY, et al: The management of nausea and vomiting of pregnancy. J Obstet Gynaecol Can 2002; 24: 817-831.
- Rey E, et al: Gastroesophageal reflux symptoms during and after pregnancy: a longitudinal study. Am J Gastroenterol 2007; 102: 2395-2400.
- Malfertheiner M, et al: Extraesophageal symptoms of gastroesophageal reflux disease during pregnancy. Journal of Gastroenterology 2015; 53: 1080-1083.
- Richter JE: Review article: the management of heartburn in pregnancy. Aliment Pharmacol Ther 2005; 22: 749-757.
- Sweis R, et al: Post-prandial reflux suppression by a raft-forming alginate (Gaviscon Advance) compared to a simple antacid documented by magnetic resonance imaging and pH-impedance monitoring: mechanistic assessment in healthy volunteers and randomised, controlled, double-blind study in reflux patients. Aliment Pharmacol Ther 2013; 37: 1093-1102.
- Strugala V, et al: Assessment of the Safety and Efficacy of a Raft-Forming Alginate Reflux Suppressant (Liquid Gaviscon) for the Treatment of Heartburn during Pregnancy. ISRN Obstet Gynecol 2012; 2012: 481870.
- Lindow SW, et al: An open-label, multicentre study to assess the safety and efficacy of a novel reflux suppressant (Gaviscon Advance) in the treatment of heartburn during pregnancy. Int J Clin Pract 2003; 57: 175-179.
- Bassey OO: Pregnancy heartburn in Nigerians and Caucasians with theories about aetiology based on manometric recordings from the esophagus and stomach. British J obstetrics and gynaecology 1977; 84: 439-443.
- Bredenoord AJ, Pandolfino JE, Smout AJPM: Gastro-oesophageal reflux disease. Lancet 2013; 381: 1933-1942.
- Quartarone G: Gastroesophageal reflux in pregnancy: a systematic review on the benefit of raft forming agents. Minerva ginecologica 2013; 65: 541-549.
- Garbis H, et al: Pregnancy outcome after exposure to ranitidine and other H2-blockers. A collaborative study of the European Network of Teratology Information Services. Reproductive toxicology 2005; 19: 453-458.
- Källén BA: Use of omeprazole during pregnancy – no hazard demonstrated in 955 infants exposed during pregnancy. Europ J obstetrics & gynecology and reproductive biology 2001; 96: 63-68.
- Diav-Citrin O, et al: The safety of proton pump inhibitors in pregnancy: a multicentre prospective controlled study. Aliment Pharmacol Ther 2005; 21: 269-275.
- Lalkin A, et al: The safety of omeprazole during pregnancy: a multicenter prospective controlled study. Am J Obstet Gynecol 1998; 179: 727-730.
- Dulgheru R: The Safety and Efficiency of Proton Pump Inhibitors during Pregnancy and Conception. Maedica (Bukhar) 2010; 5: 304.
- Gerson LB: Proton pump inhibitors and safety during pregnancy. Gastroenterology 2011; 141: 389-391.
- Gill SK, et al: The safety of proton pump inhibitors (PPIs) in pregnancy: a meta-analysis. Am J Gastroenterol 2009; 104: 1541-1545.
- Matok I, et al: The safety of fetal exposure to proton-pump inhibitors during pregnancy. Dig Dis Sci 2012; 57: 699-705.
- Nielsen GL, et al: The safety of proton pump inhibitors in pregnancy. Aliment Pharmacol Ther 1999; 13: 1085-1089.
- Bradley CS, et al: Constipation in pregnancy: prevalence, symptoms, and risk factors. Obstet Gynecol 2007; 110: 1351-1357.
- Cullen G, O’Donoghue D: Constipation and pregnancy. Best Pract Res Clin Gastroenterol 2007; 21: 807-818.
- Breymann C: Iron Deficiency Anemia in Pregnancy. Seminars in Hematology 2015; 52: 339-347.
- Scanlon KS, et al: High and low hemoglobin levels during pregnancy: differential risks for preterm birth and small for gestational age. Obstet Gynecol 2000; 96: 741-748.
- García Duarte S, et al: Prevention of constipation during pregnancy with the hydration. Nutrición hospitalaria 2015; 32: 10298.
- Rungsiprakarn P, et al: Interventions for treating constipation in pregnancy. Cochrane Database Syst Rev 2015; 9: CD011448.
- Quartero AO, et al: Bulking agents, antispasmodic and antidepressant medication for the treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2005: CD003460.
- Tytgat GN, et al: Contemporary understanding and management of reflux and constipation in the general population and pregnancy: a consensus meeting. Alimentary pharmacology & therapeutics 2003; 18: 291-301.
- Ebrahimi N, et al: The fetal safety of hydrocortisone-pramoxine (Proctofoam-HC) for the treatment of hemorrhoids in late pregnancy. Journal of obstetrics and gynaecology Canada 2011; 33: 153-158.
- Avsar AF, Keskin HL: Haemorrhoids during pregnancy. J obstetrics and gynaecology 2010; 30: 231-237.
- Wald A: Constipation, diarrhea, and symptomatic hemorrhoids during pregnancy. Gastroenterology clinics of North America 2003; 32: 309-322, vii.
- van der Woude CJ, et al: The second European evidenced-based consensus on reproduction and pregnancy in inflammatory bowel disease. J Crohns Colitis 2015; 9: 107-124.
- Oresland T, et al: Gynaecological and sexual function related to anatomical changes in the female pelvis after restorative proctocolectomy. Int J Colorectal Dis 1994; 9: 77-81.
- Beyer-Berjot L, et al: A total laparoscopic approach reduces the infertility rate after ileal pouch-anal anastomosis: a 2-center study. Ann Surg 2013; 258: 275-282.
- Cornish J, et al: A meta-analysis on the influence of inflammatory bowel disease on pregnancy. Gut 2007; 56: 830-837.
- Pedersen N, et al: The course of inflammatory bowel disease during pregnancy and postpartum: a prospective European ECCO-EpiCom Study of 209 pregnant women. Aliment Pharmacol Ther 2013; 38: 501-512.
- Broms G, et al: Complications from inflammatory bowel disease during pregnancy and delivery. Clin Gastroenterol Hepatol 2012; 10: 1246-1252.
- Malangoni M: Gastrointestinal surgery and pregnancy. Gastroenterology clinics of North America 2003; 32: 181-200.
- Mendez-Sanchez N, et al: Pregnancy and gallbladder disease. Ann Hepatol 2006; 5: 227-230.
- Lindseth G, Bird-Baker MY: Risk factors for cholelithiasis in pregnancy. Res Nurs Health 2004; 27: 382-391.
- Mihu D, et al: HELLP syndrome – a multisystemic disorder. J Gastrointestin Liver Dis 2007; 16: 419-424.
- Lu EJ, et al: Medical versus surgical management of biliary tract disease in pregnancy. Am J Surg 2004; 188: 755-759.
- Angel Garcia AL: Effect of pregnancy on pre-existing liver disease physiological changes during pregnancy. Ann Hepatol 2006; 5: 184-186.
- Allen AM, et al: The Epidemiology of Liver Diseases Unique to Pregnancy in a US Community: A Population-Based Study. Clin Gastroenterol Hepatol 2016; 14: 287-294 e2.
- Schutt VA, Minuk GY: Liver diseases unique to pregnancy. Best Pract Res Clin Gastroenterol 2007; 21: 771-792.
- Ahmed KT, et al: Liver diseases in pregnancy: diseases unique to pregnancy. World J Gastroenterol 2013; 19: 7639-7646.
- Martin JN, et al: Understanding and managing HELLP syndrome: the integral role of aggressive glucocorticoids for mother and child. Am J Obstet Gynecol 2006; 195: 914-934.
HAUSARZT PRAXIS 2016; 11(2): 18-23











