Case report: A 31-year-old, previously internally healthy woman was admitted for psychiatric treatment due to increasing disorientation and neglect. She described a lack of drive and limitation of memory that had been accentuating for two months.
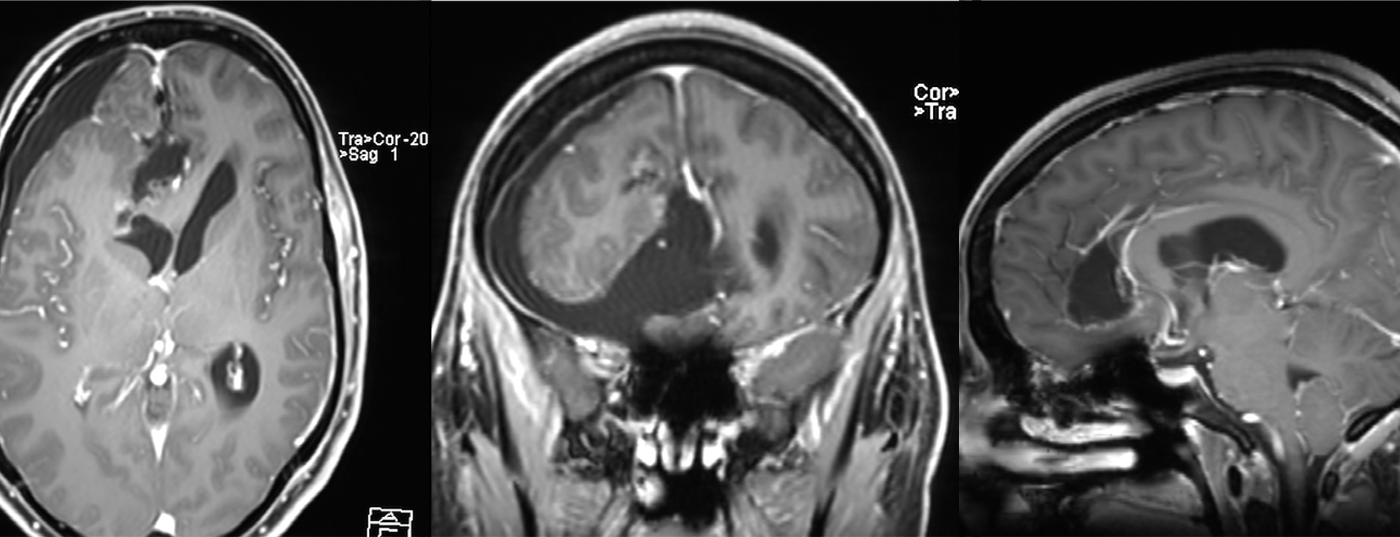
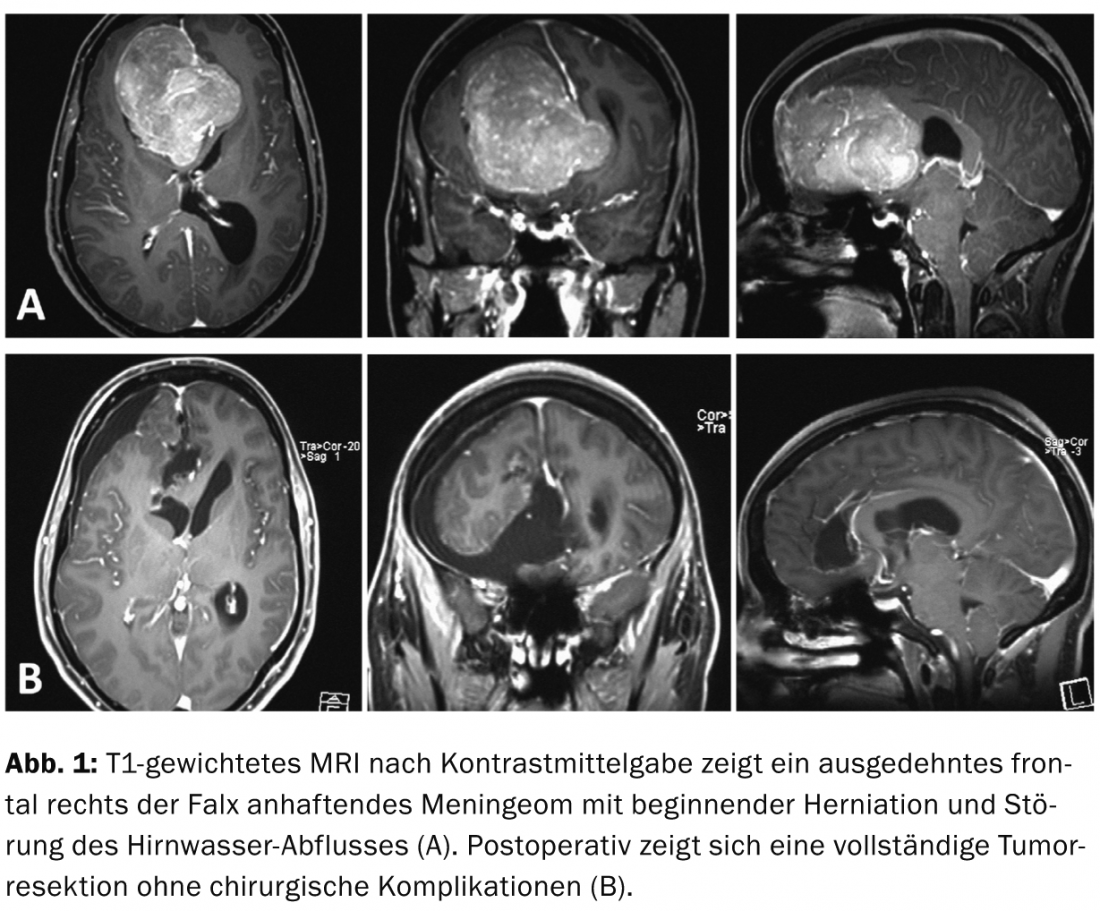
With a suspected diagnosis of organically caused frontal brain syndrome, an MRI of the skull was performed; this revealed a huge, highly contrast-enhancing mass adherent to the frontal right of the falx. The most likely differential diagnosis was a meningioma; the onset of herniation and a disturbance of cerebrospinal fluid outflow from the left lateral ventricle were conspicuous (Fig. 1a) . From a neurosurgical point of view, urgent removal of the tumor was indicated to prevent progressive brain entrapment with possible permanent neurological damage or even a lethal outcome.
Classically, large cranial openings are also used to remove large intracranial masses. However, these extensive incisions and craniotomies are associated with a high risk, as healthy brain areas are always exposed and thus exposed to possible injury. In recent years, on the other hand, the principles of keyhole surgery in terms of optimized access planning and smaller craniotomies, as well as the use of neuroendoscopy, have become increasingly widespread.
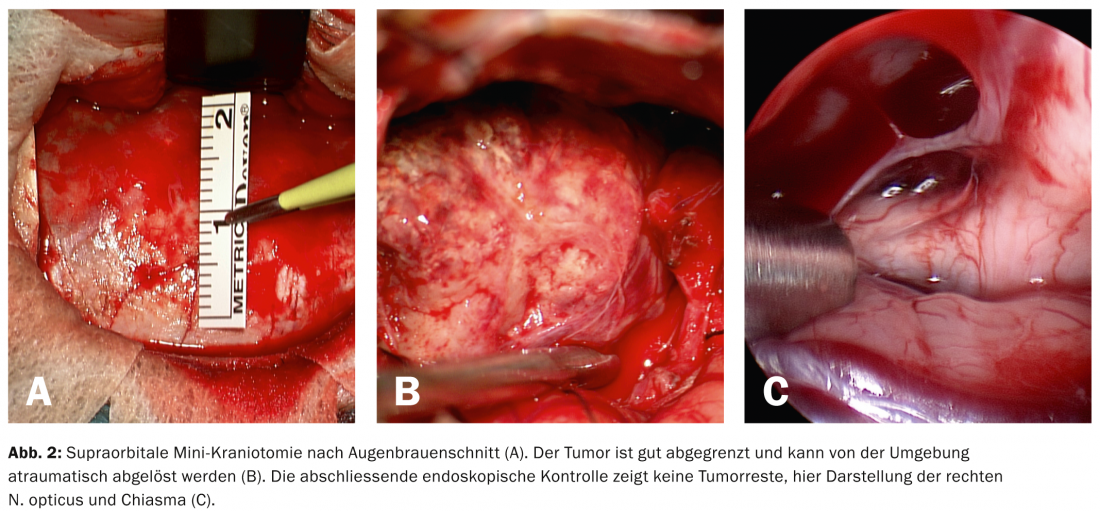
In this patient, removal of the tumor was performed via a supraorbital brow incision and frontal mini-craniotomy (Fig. 2a) . After entering the subfrontal space, the surface of the tumor could be visualized directly underneath. This showed good boundary to normal brain tissue, strong vascularization, and consistency typical of meningioma (Fig. 2b). After removal of the tumor, the hidden corners of the resection cavity were now inspected by endoscope for tumor remnants (Fig. 2c).
The patient awoke promptly from anesthesia without the appearance of a fresh focal neurologic deficit. On the following day, complete resection of the tumor without complications was documented by MRI (Fig. 1b).
Discussion: From Lahmeyer et al. comes the first description of a frontal meningioma diagnosed due to initial symptoms of refractory depression [1]. The first major series of cases with frontal lesions and resulting psychiatric illnesses comes from Starkstein et al. from the year 1988 [2]. In a 1995 study, Lampl et al. describe. a significantly increased incidence of psychiatric comorbidities in patients with frontal meningioma compared with those patients with meningioma of other locations [3]. In addition, a significant correlation between the size of the perilesional edema and the occurrence of psychiatric symptoms, but not the occurrence of neurological symptoms, was described by these authors.
Complete regression of preoperative depression after extirpation of a large sphenoid wing meningioma is reported by Ciobanu et al. described in a 68-year-old female patient [4]. In this case, a depressive mood state that increased over three months and eventually met the criteria for major depressive disorder led to the diagnosis of meningioma. After tumor resection, all preoperative symptoms showed normalization within six months.
Summary: Intracranial space-occupying lesions can cause severe psychiatric symptoms even in the absence of focal neurologic deficits and/or epileptic seizures. The prognosis appears very favorable after surgical extirpation. Therefore, early exclusion of an organic cause using cranial imaging is recommended for new, rapidly progressive psychiatric disorders.
Prof. Dr. med. Robert Reisch
Marton Eördögh
PD Stefan Kaiser, MD
Prof. Dr. med. Stephan G. Wetzel
Literature:
- Lahmeyer HW: Frontal lobe meningioma and depression. The Journal of clinical psychiatry. 1982; 43(6): 254-255. Epub 1982/06/01.
- Starkstein SE, Boston JD, Robinson RG: Mechanisms of mania after brain injury. 12 case reports and review of the literature. The Journal of nervous and mental disease. 1988; 176(2): 87-100. Epub 1988/02/01.
- Lampl Y, et al: Intracranial meningiomas: correlation of peritumoral edema and psychiatric disturbances. Psychiatry research. 1995; 58(2): 177-180. epub 1995/09/29.
- Ciobanu AM, et al: Giant wing sphenoid meningioma with principal manifestation depression. Romanian journal of morphology and embryology = Revue roumaine de morphologie et embryologie 2009; 50(4): 713-717. Epub 2009/11/28.
InFo Neurology & Psychiatry 2014; 12(2): 20-21.