Relapses characterized by large pustules on the skin are characteristic of generalized pustular psoriasis (GPP) and can be associated with systemic inflammatory reactions and serious complications. A study published this year in JEADV analyzed data from a large European cohort of GPP patients. It was confirmed that the clinical picture is heterogeneous, with the severity of symptoms varying inter- and intra-individually.
The symptoms associated with GPP, such as pain, fever and fatigue, as well as frequently associated comorbidities, can significantly impair quality of life [1,2]. In addition, patients with GPP often suffer from anxiety and depression [3]. The European Rare and Severe Psoriasis Expert Network (ERASPEN) defines GPP as a disease with primary, sterile, macroscopically visible pustules on non-acral skin (outside of psoriatic plaques) [4]. The deep-seated pustules manifest in the area of the upper dermis (“spongiform Kogoj pustules”), the stratus spinosum (“Munro microabscesses”) and within or adjacent to the horny layer of the epidermis. The formation of pustules is accompanied by a pronounced infiltration of neutrophil granulocytes and mononuclear cells into the epidermis [4,5].
Multicenter European case series
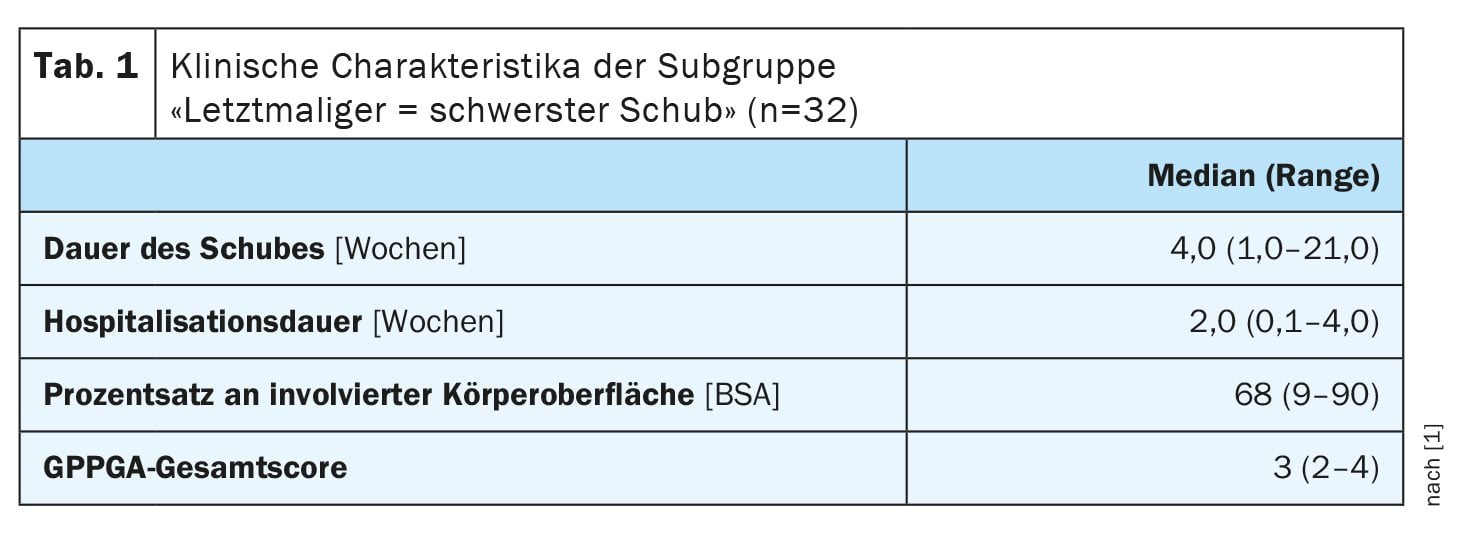
According to the ERASPEN definition, GPP is characterized by a recurrent or persistent course, whereby the pustular formation may be accompanied by systemic inflammation and/or occur simultaneously with symptoms of psoriasis vulgaris [4]. The Generalized Pustular Psoriasis Physician Global Assessment (GPPGA) score is often used to assess the severity of GPP [6–8]. Characteristic features of GPP can be detected in histological preparations, such as a pronounced neutrophil infiltrate in the upper dermis, spongiform Kogoj pustules and hyperkeratosis with neutrophil microabscesses in the epidermis. A definitive diagnosis is usually only possible by looking at the medical history and clinical findings together. In a study conducted in 2022 and published in 2024 by Wolf et al., 58 patients with GPP were recruited from 12 medical centers in nine European countries [1]. The GPP diagnosis was verified using the ERASPEN criteria. In 80.4% of patients, the diagnosis was confirmed by additional skin biopsies. The average age of the participants was 61 years (range: 16-92) and 60.3% were female. The most common comorbidities were hypertension (43.1%) and hyperlipidemia (32.8%). 34 patients (58.6%) had concurrent plaque psoriasis before or during the course of GPP [1]. Data from two separate relapses were recorded in 26 individuals; in 32 patients, the last relapse was reported as the most severe.
To obtain a quantitative measure of the severity of a patient’s systemic symptoms, each patient was assigned a combined systemic disease score (0-6) based on the presence of systemic inflammatory symptoms and inflammatory markers during each episode. One point was assigned for the presence of each of the following criteria:
- Fever [>38°C]
- Elevated C-reactive protein (CRP) levels (>5 mg/L)
- Elevated leukocyte levels (>10 000 or >13 000 μL)
- Hypocalcemia (<2.1 mmol/L),
- Hypoalbuminemia (<35 g/L)
- elevated transaminase levels (serum alanine transaminase level >35 or >45 U/L; serum aspartate transaminase level >35 or >40 U/L).
Among all participants (N=58), the doctor determined the (a) most recent and (b) most severe relapse based on all documented episodes. In 32 patients, the most recent episode proved to be the most severe episode to date (Table 1). Over 90% of patients were hospitalized as a result of a most severe episode, of which over 75% had an overall GPPGA score of 3 or 4. Systemic symptoms were more common in patients with a GPPGA score of 3 or 4, but were also seen in patients with a GPPGA score ≤2. A Pearson correlation analysis was performed on the data from all individual relapses to determine the relationship between the combined systemic disease score and the GPPGA total score, the GPPGA pustulation subscore and the duration of the relapse. A significant correlation was found between a combined systemic disease score of clinical and laboratory features and the GPPGA total score (r=0.385, p<0.001) and the GPPGA pustulation subscore (r=0.305, p<0.05).
Correlations with GPPGA scores
Surprisingly, systemic symptoms also occurred in patients with a GPPGA total score or GPPGA pustulation subscore of 1 or 2 [1]. But overall, a significant association was found between the combined systemic disease score and both the GPPGA total score (r=0.385, p<0.001) and the GPPGA pustulation subscore (r=0.305, p<0.05) as well as the length of hospital stay (r=0.349, p<0.05). The GPPGA total score also correlated significantly with CRP concentration (r=0.360, p<0.05) and neutrophils (r=0.331, p<0.05), as did the GPPGA pustulation subscore (CRP: r=0.332; neutrophils: r=0.320, p<0.05 for both). The leukocyte values did not correlate significantly with the GPPGA total score (r=0.253) or the GPPGA pustule subscore (r=0.259).
A greater increase in systemic symptoms, including fever (>38°C), elevated CRP and leukocyte levels, and higher GPPGA scores, was observed in the subgroups with the most severe flare by history (n=26) and the most recent and most severe flare simultaneously (n=32) compared to the subgroup with other recent flares (n=26). In the subgroup of those in whom the most recent flare was also the most severe, a higher proportion of patients had GPPGA scores of 3 or 4 compared to the other patients. A greater proportion of patients had systemic symptoms and elevated markers of systemic inflammation during their most severe flare than during their most recent flare.
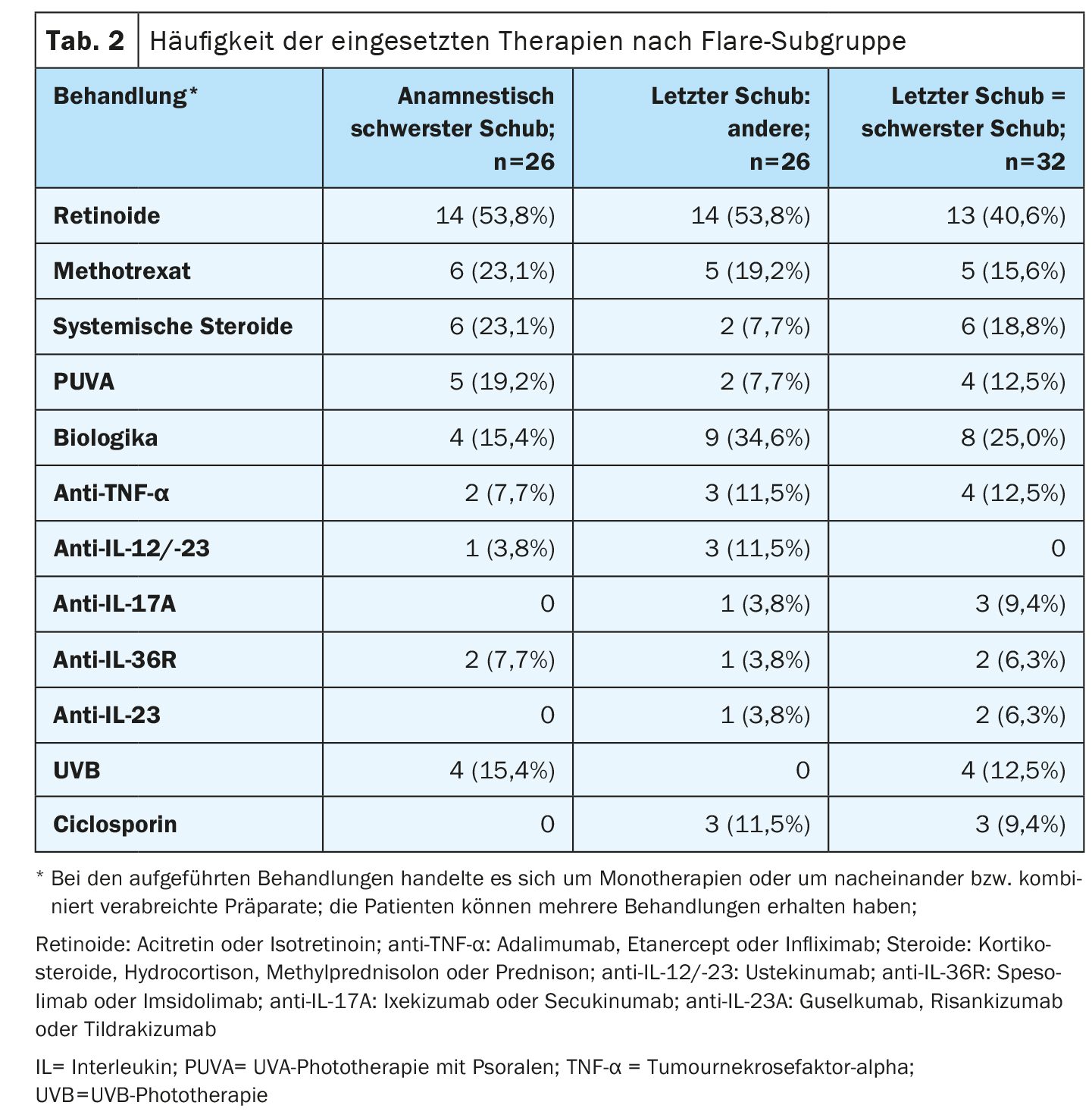
Therapies used at a glance
Retinoids were the most frequently used treatment in all subgroups (Table 2), whereby the percentage of patients treated with biologics was higher in the subgroup “last relapse = most severe relapse” (25.0%; 8 of 32) compared to the subgroup “anemnestic most severe relapse” (15.4%; 4 of 26). The use of phototherapy in the form of PUVA (psoralen with UV-A) or UVB was higher in the subgroup with the anamnestic most severe relapse than in the subgroups in which the most recent relapse corresponded to the most severe relapse to date, as well as other recent relapses. The same applies to the treatment option of systemic steroids. Ciclosporin was rarely used both in the subgroup with the most severe relapse in the patient’s history and in the subgroup with the most recent and most severe relapse: 0% (n=0) and 9.4% (3 of 32) respectively.
With a relative frequency of 77.4% (65 out of 84), the majority of episodes resolved. The mean time from the start of treatment to the resolution of the relapse was comparable in all subgroups:
- History of most severe relapse, 4 (range 1-16) weeks
- Last and most severe episode: 4 (range 0.1-52) weeks
- Other last relapses: 4 (range 1-54) weeks.
In summary, all GPP relapses were associated with a significant clinical burden, which emphasizes the importance of early diagnosis as a basis for prompt adequate treatment.
Literature:
- Wolf P, et al: Characteristics and management of generalized pustular psoriasis (GPP): Experience from the Central and Eastern Europe (CEE) GPP Expert Network. JEADV 2024; 38(8): 1531-1542.
- Prinz JC, et al: JEADV 2022; 37: 256-273.
- Lebwohl M, et al: J Psoriasis Psoriatic Arthritis. 2022; 7(2): 71-78.
- Navarini AA, et al: JEADV 2017; 31(11): 1792-1799.
- Benjegerdes KE, et al: Psoriasis (Auckl) 2016; 6: 131-144.
- Bachelez H, et al: NEJM 2019; 380(10): 981-983.
- Bachelez H, et al: NEJM 2021; 385(26): 2431-2440.
- Burden AD, et al: Am J Clin Dermatol 2022; 23(Suppl 1): 39-50.
DERMATOLOGY PRACTICE 2024; 34(5): 42-43