Polyarteritis Nodosa (PAN) is a vasculitis of medium and small vessels. The incidence is estimated at 1.6 to 1.9 cases per million inhabitants per year, which is probably one reason why the guidelines have not been updated for some time and why there are some new findings that have not yet been incorporated. An expert gave an overview of current diagnostics and therapy at the DGRh congress.
One reason for the statistically significant decline in PAN cases in recent years may be the improved treatment options for hepatitis B, explained Prof. Dr. Ina Kötter, Clinic for Rheumatology and Immunology, Section for Rheumatology and Inflammatory Systemic Diseases at the UKE, Klinikum Bad Bramstedt [1]. However, with a prevalence of 30 per million inhabitants, it is not surprising that there are not many studies on the subject. “It is a problem that, unlike with other vasculitides, there are no new classification and diagnostic criteria, but the old ACR guidelines from 1990 still apply.” On the one hand, hepatitis B is listed as the trigger, which is hardly the case today. Secondly, renal involvement is defined as elevated serum urea or creatinine. “Of course, by the time that happens, you’re already too late,” says the rheumatologist.
Pediatric rheumatologists were quicker in this regard and in 2010 defined renal involvement much more sensitively in the EULAR/PRINTO criteria for pediatric PAN and included proteinuria. Hepatitis also no longer occurs here. Prof. Kötter believes that in the future there will also be a points system in which factors such as mononeuritis multiplex, gastrointestinal symptoms, absence of MPO-ANCA, proteinuria, general symptoms, angiographic abnormalities, i.e. multiple connected aneurysms, and also typical histology will each count for one point and the criteria will be fulfilled when a certain total number of points is reached.
In terms of symptoms, many patients have arthralgia and over 60% also have myalgia. Neuropathies, CNS involvement, skin changes and kidney involvement are also relatively common. There is a significant difference between children and adults: Adults have significantly more peripheral neurological involvement (PNS), whereas children have more CNS involvement. “You also have to bear in mind that childhood PAN is always suspicious of adenosine deaminase 2 deficiency (DADA2), a genetic vasculitis with predominant CNS involvement, but also with an immunodeficiency.”
Coronariitis – the forgotten symptom
In a retrospective Chinese analysis of 145 PAN patients, 13.7% (n=19) had coronary artery aneurysms resulting in CHD. The evaluation showed that patients with aneurysms had less weight loss, less subcutaneous and more peripheral vascular involvement, especially cranial arteries, carotid, kidney, intestine and lower extremities. Hypertension also occurred more frequently.
If someone with CHD has no typical cardiovascular factors, then you should definitely look for other organ involvement, examine antibodies, check inflammation parameters and, if in doubt, also consult a rheumatologist, was the conclusion. The multivariate analysis showed that intestinal artery involvement (OR 3.722; p=0.033) and hypertension (OR 6.668; p=0.003) were the main risk factors for coronary artery involvement. “If you have patients with PAN and these symptoms, then you should definitely look for coronary involvement before the patients become symptomatic in this regard,” Prof. Kötter advises.
Older people are more often systemic
A look at the age distribution shows that patients with a mild cutaneous clinical picture are younger, those with severe cutaneous PAN are slightly older, and people with systemic PAN are the oldest.
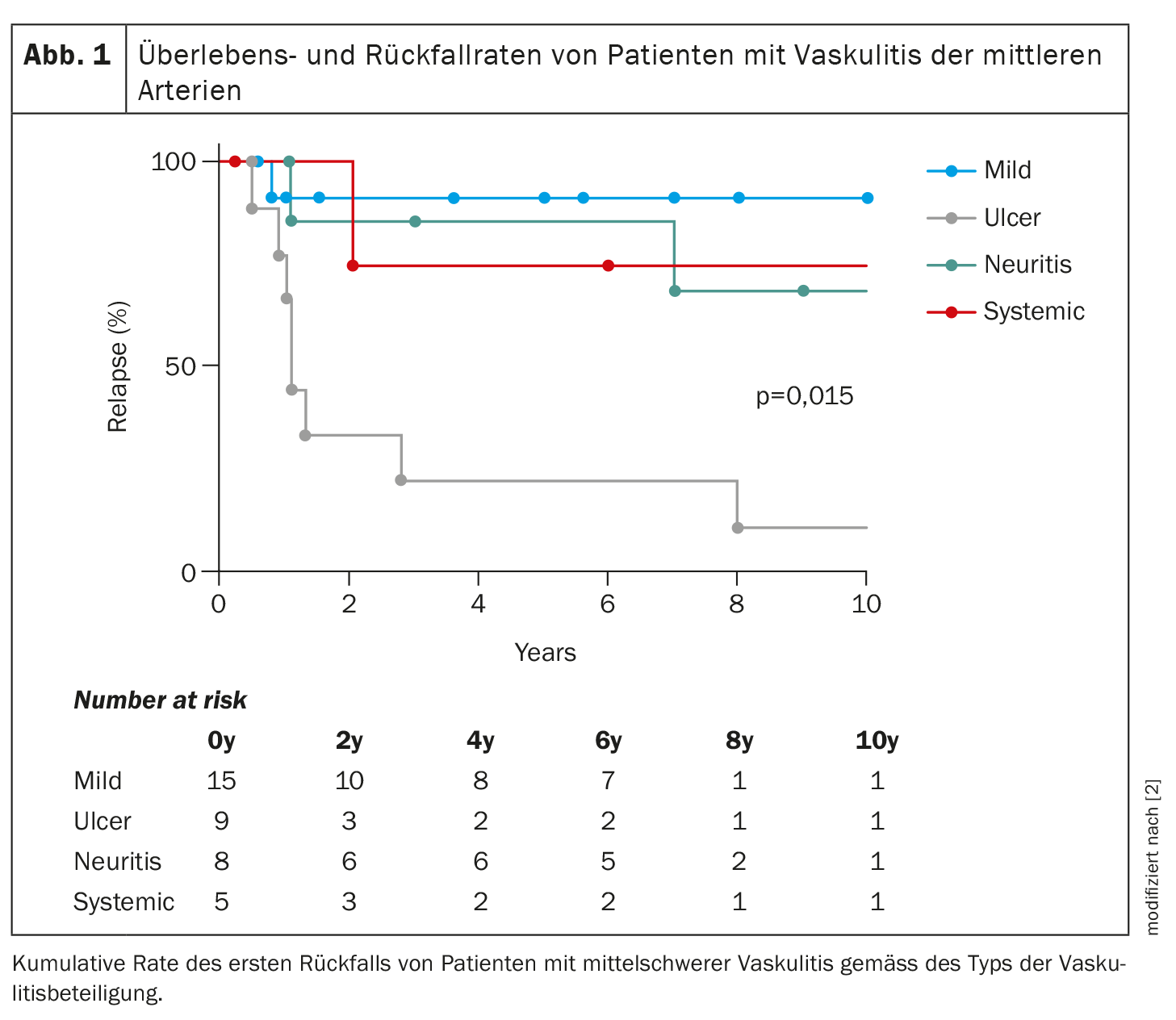
In terms of long-term survival, systemic PAN has the worst values, “but what is exciting is that the most frequent recurrences with ulcers occur in severe cutaneous PAN,” said the expert (Fig. 1). This means that there are fewer recurrences with systemic PAN than with severe cutaneous PAN.
The pathogenesis is based on environmental triggers. In addition, there are comorbidities such as chronic myelomonocytic leukemia (CMML). An immunogenetic predisposition is also suspected. However, according to Prof. Kötter, in contrast to other vasculitides, this has not yet been properly defined and investigated in the case of PAN.
Diagnostics and therapy
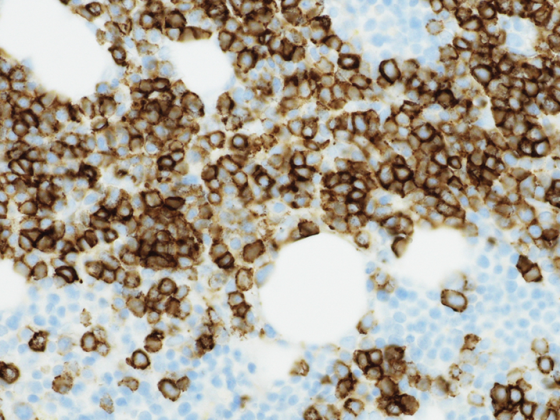
Not every PAN patient must be affected on the skin. In addition to the skin biopsy, other diagnostic methods are available: MRI and ultrasound are available for muscular PAN. There, hypo- and hyperechogenicities become visible, which then correlate with the inflammation in the MRI. A recent study from France examined 10 patients, all of whom had myalgias, arthralgias and systemic symptoms and in whom PAN had already been confirmed by skin biopsy. In all of them, accumulations were found on PET-CT, either in the muscle, linear or focal, and in 4 out of 10 also in the large vessels.
In contrast to the diagnostic criteria, there are recommendations from the American College of Rheumatology (ACR) for the treatment of PAN. In the case of active disease, intravenous cyclophosphamide plus methylprednisolone is recommended. Cyclophosphamide should be maintained until remission, followed by a switch to another immunosuppressant, preferably MTX, AZA or MMF. If there is no severe organ involvement, the immunosuppressants are used directly plus glucocorticoids. If refractory, escalation to the aforementioned therapy is recommended.
“What is not included in the ACR recommendations is DADA2 deficiency – this is treated directly with a TNF inhibitor.” Prof. Kötter questioned whether PAN, which is limited to the skin, can only be treated with hydroxychloroquine, “and this must also be an important consideration: What do we do if cyclophosphamide doesn’t help?” In this case, she referred to a retrospective study from France in which biologics were compared with each other, albeit only in a small cohort of between 10 and 18 patients.
In the comparison of rituximab vs. TNF blockers vs. tocilizumab, tocilizumab helped to achieve the remissions, but also caused the most side effects, including intestinal perforations in some cases. The BVAS as an activity score even dropped to 0 with tocilizumab after 12 months, and the drug also appeared to be superior to the other substances in the Kaplan-Meier curve.
An Indian study on JAK inhibitors included four cases with cutaneous PAN and showed improvements. This could perhaps be another promising therapeutic principle, the speaker concluded.
Source:
- Kötter I: Vortrag «Seltene Vaskulitiden»; Deutscher Rheumatologiekongress 2023, Leipzig, 31.08.2023.
- Shirai T, Shirota Y, Fujii H, et al.: Four distinct clinical phenotypes of vasculitis affecting medium-sized arteries. Scandinavian Journal of Rheumatology 2019; 48: 308-314; doi: 10.1080/03009742.2018.1551965.
InFo RHEUMATOLOGIE 2023; 5(2):26–27