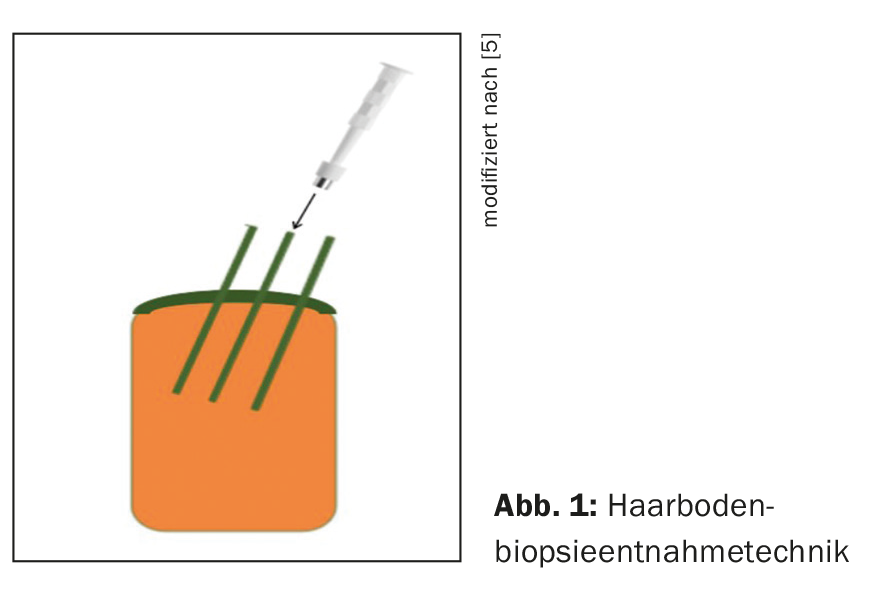
If alopecia cannot be clearly diagnosed on the basis of clinical assessment, a specimen biopsy may be informative. If non-scarring alopecia is suspected, collection of two specimens for vertical and horizontal sections is recommended. When scarring alopecia is suspected, additional direct immunofluorescence examination is very helpful in making the correct diagnosis. The hair base biopsy should ideally be taken from the periphery of an alopecic focus in the direction of hair growth.
A patient with hair loss is always a challenge for the treating physician and a hair follicle biopsy to clarify alopecia for the (dermato)pathologist. Above all, it becomes difficult for the clinician if the light scalp areas cannot be assigned to any distribution pattern. In this case, one hopes for resolution from a histologic examination.
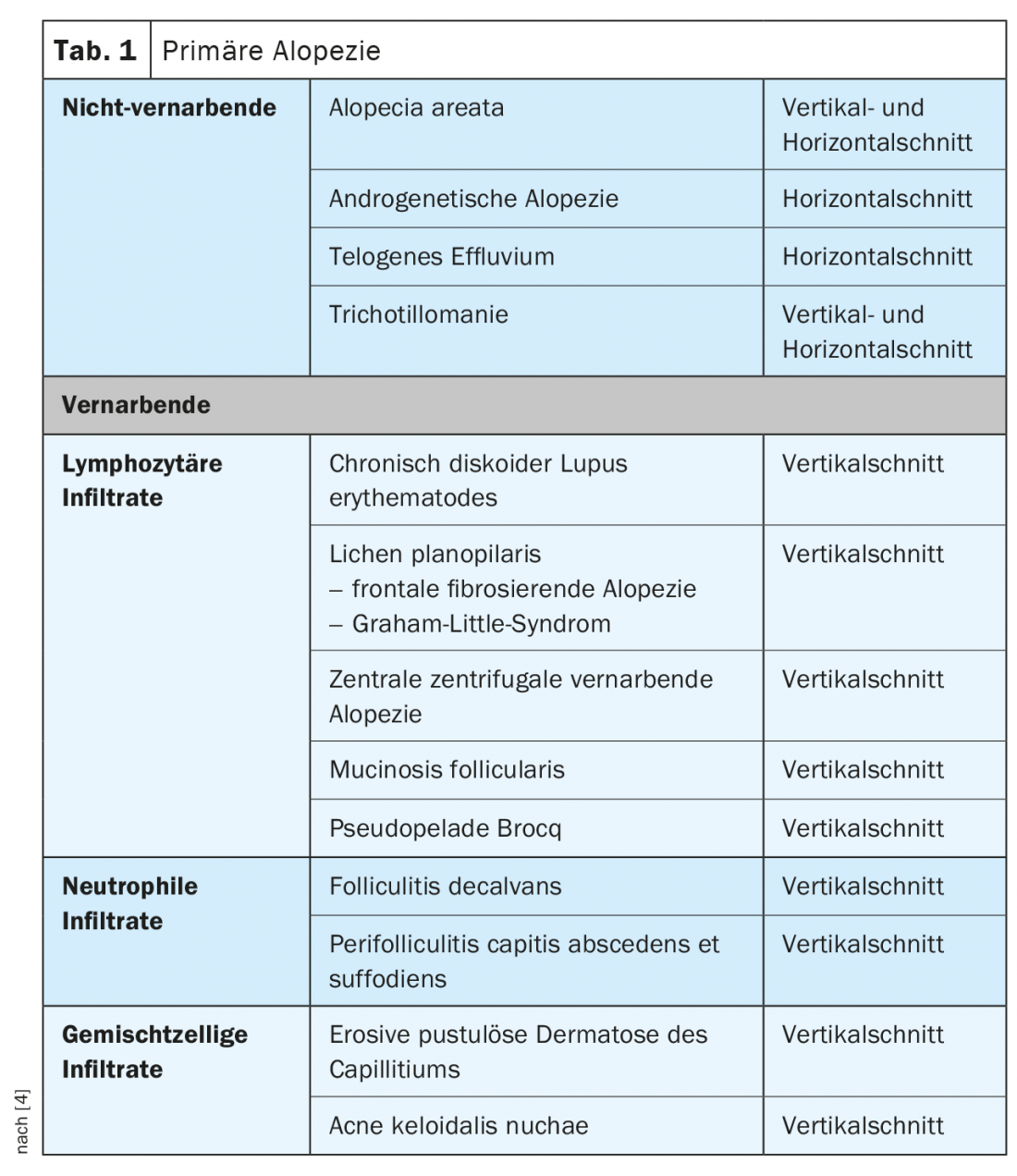
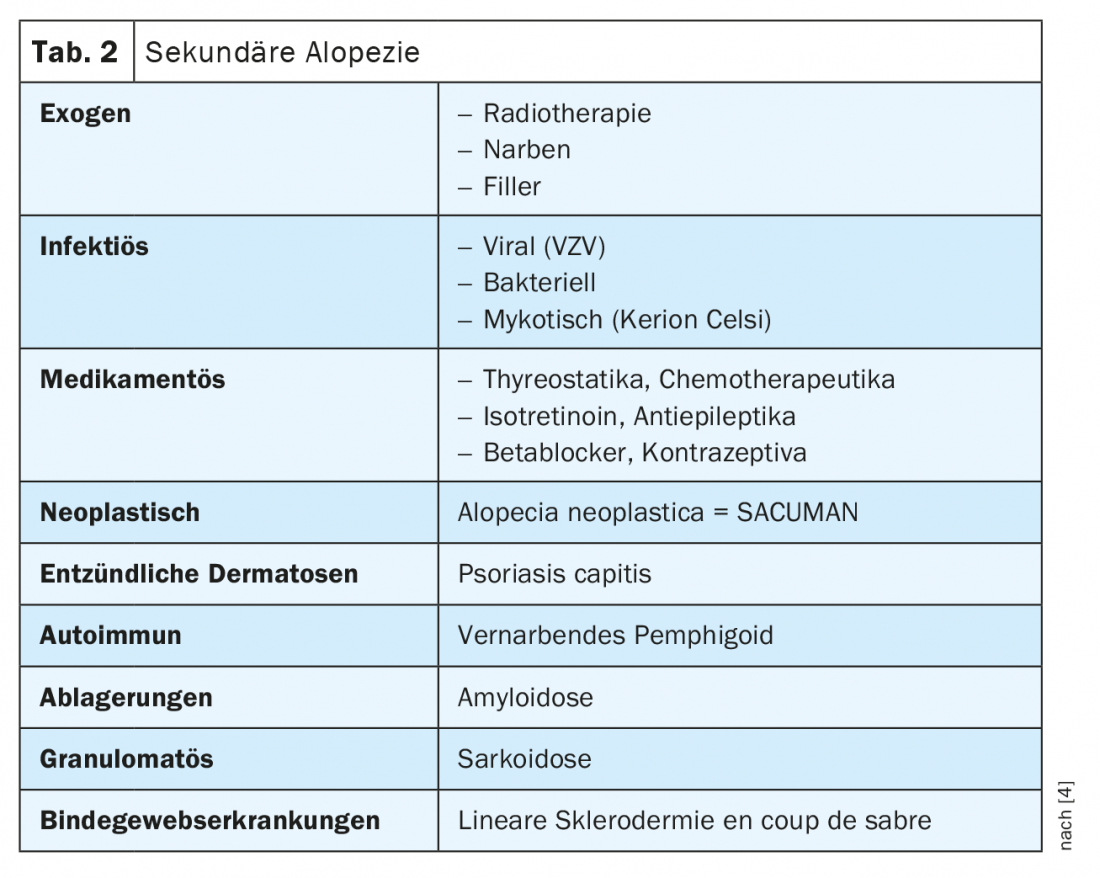
Alopecia is divided into primary non-scarring and scarring (Table 1) and secondary non-scarring and scarring (Table 2) . Histologically, in non-scarring alopecia, the hair follicles are preserved, accompanied by a low-grade inflammatory infiltrate. The scarring form is characterized by irreversible destruction of the hair follicles and an inflammatory process.
- For optimal histologic evaluation, a 4-6-mm punch, carefully taken in the direction of terminal hairs (not perpendicular!) from the periphery of an alopecic focus with hairs still preserved, with abundant subcutaneous adipose tissue, without squeezing, is best suited, as well as accurate clinical information on the submission form and possibly a clinical photograph (Fig. 1). For direct immunofluorescence examination, one third of the punch from the same site can be additionally recut and sent in Michel’s solution.
- Apart from a HE cut, special dyes such as PAS, Alcian blue and Elastika are made.
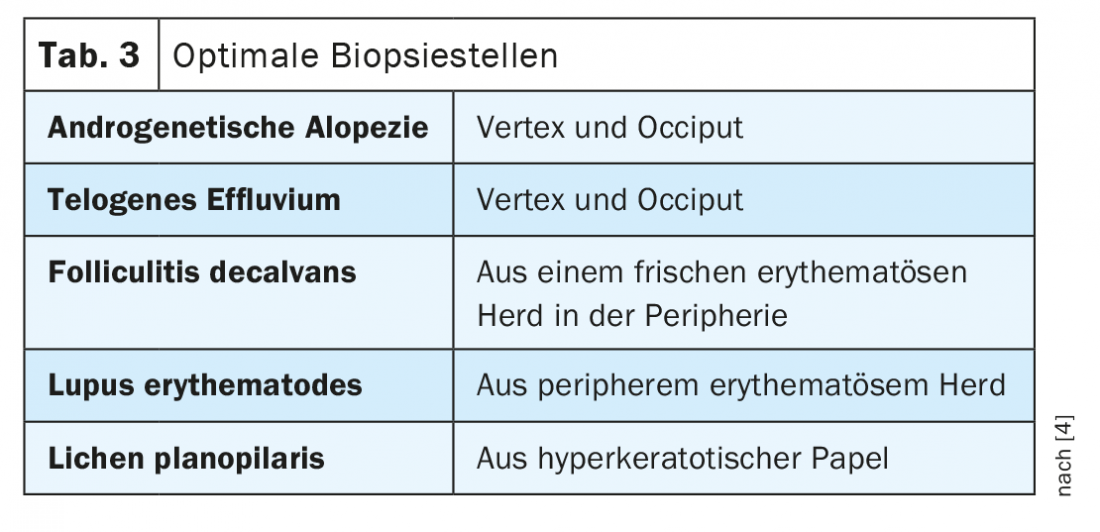
- For non-scarring alopecia, a horizontal section is still considered the gold standard for diagnosis. Two 4-mm punches or one 4-6-mm punch are taken for this purpose.
- For the horizontal section, the punch is cut 1-2 mm below the dermoepidermal junction zone (Fig. 2).
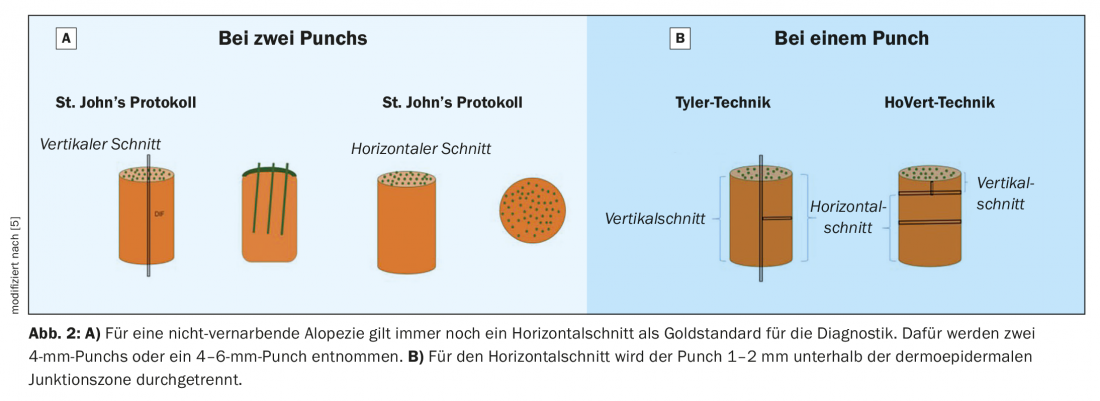
A horizontal section provides the diagnostician with a complete number, stages of development, density and ratio of all hair follicles in the biopsy taken (Tab. 3) . For this reason, this technique is suitable for the diagnosis of non-scarring, low-inflammatory alopecia such as telogen effluvium, androgenetic alopecia and alopecia areata.
Because of the visualization of morphologic changes at all levels, the vertical section alone is almost always sufficient for diagnosis in scarring alopecia. There has long been a dispute in the literature about the redundancy of the horizontal section, which was first described by Headington in 1984 [1]. A horizontal section usually causes a headache for the routine (dermato)pathologist already because of the recognition and assignment of hair cycle stages on different skin levels. According to Böer [2] and Du [3], optimal histological diagnosis is possible exclusively on a vertical section.
Non-scarring alopecia
Alopecia areata
Alopecia areata is a T-cell-mediated autoimmune disease that can affect both the scalp and the rest of the integument and most commonly occurs in adults around the age of 30. A special variant of the entity, alopecia areata incognita, can easily be confused with telogen effluvium.
Histologic:
Early stage
- Catagen/Telogen phase increased
- Dilatation in the infundibulum (“Swiss cheese”-like pattern)
- peri/supraperibulbar swarm-like (Fig. 3) lymphocytic infiltrates (single eosinophils).
- Pigment scholes in the bulb and in the fibrous steles
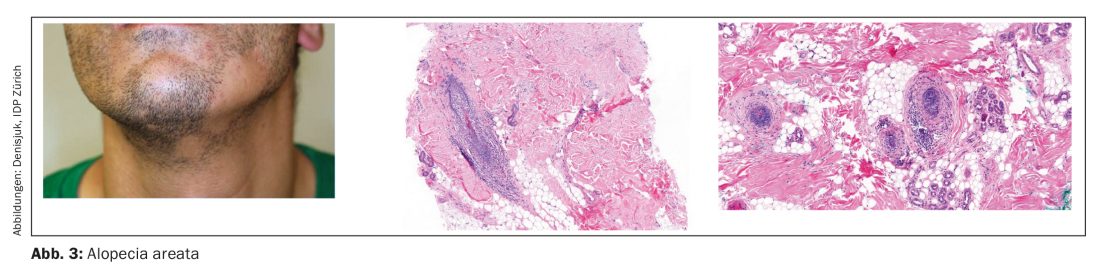
Late stage
- Miniaturized follicles in the upper and middle corium
- Numerous telogen hairs
- Absence of inflammation in deep corium/subcutis
- Fibrous stelae with melanin pigment and lymphocytes
Scarring lymphocytic alopecia
Lupus erythematosus (LE)
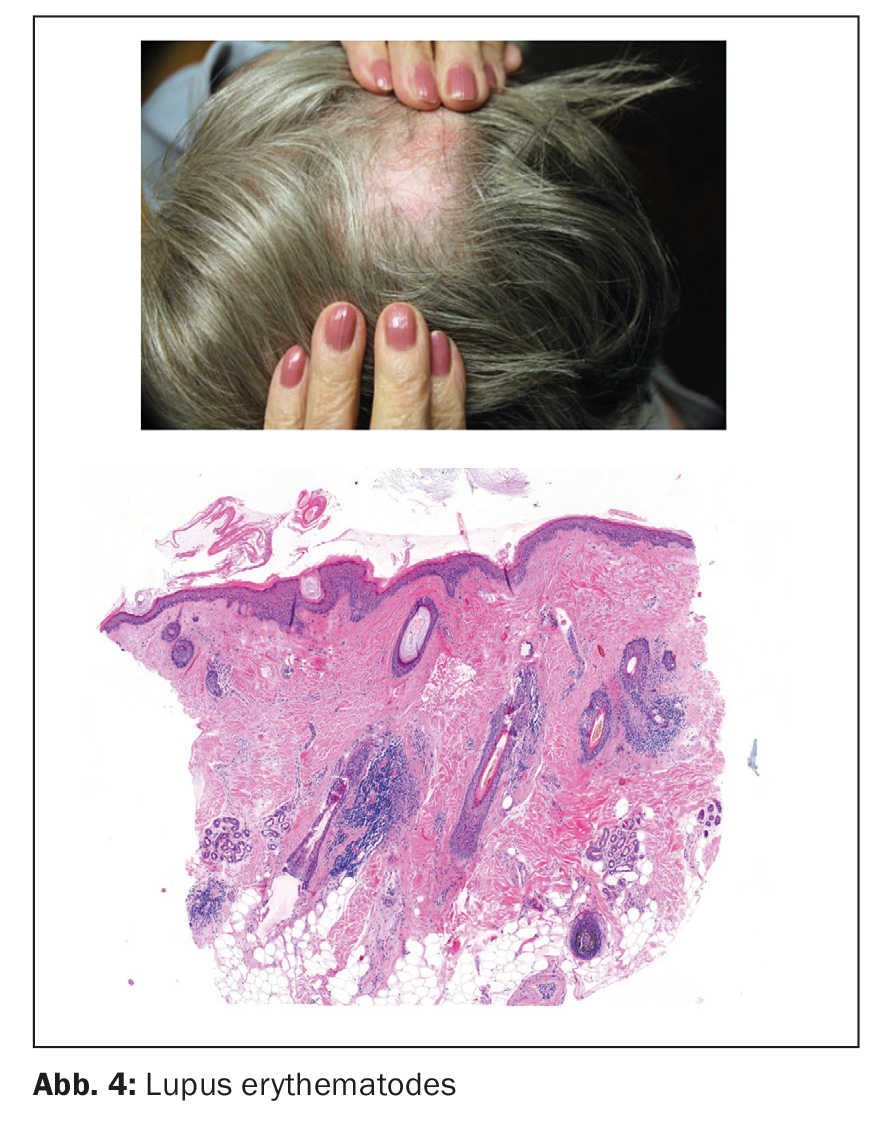
Chronic discoid lupus erythematosus most commonly occurs in middle-aged women in the form of peripherally hyperkeratotic, centrally atrophic, hairless plaques with follicular horny plugs, so-called “red dots.”
Histologic:
- Interfacial dermatitis in the area of the follicular epithelium and the epidermis
- Including deep perivascular, perifollicular, and peri-ecrine lymphoplasmacytic infiltrates with plasma cells and CD123+ plasmocytoid dendritic cells (Fig. 4).
- subcutaneous lymphoid follicles
- PAS+ Widening of the basement membrane
- deep mucin deposits
- Foreign body granulomas around hair shafts
- In direct immunofluorescence examination (DIF) IgG+, C3+, IgA+, IgM+ “Lupus band”.
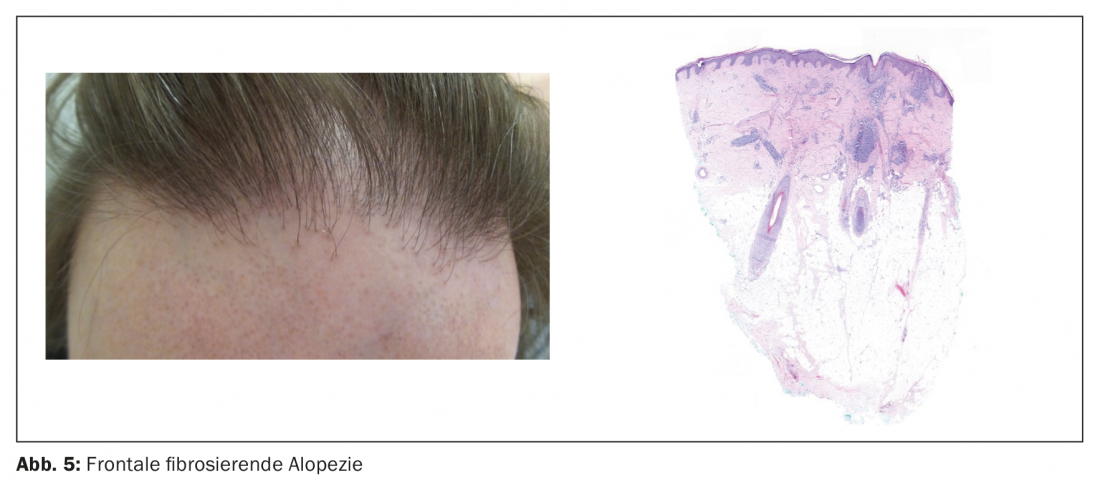
Lichen planopilaris (LPP)
Lichen planopilaris most commonly affects women over the age of 50. The clinical picture includes perifollicular papules, hyperkeratosis, atrophic scars, polytrichia without evidence of “red dots”. Differentiation from CDLE is often difficult both clinically and histologically.
Histologic:
Early stage
- lichenoid reaction in the follicular epithelial region at the level of the infundibulum/isthmus (bulbar stem cell region)
Late stage
- concentric perifollicular fibrosis (Fig. 5)
- wedge-shaped loss of elastic fibers around infundibulum
- fibrotic steles
- Polytrichy
- In DIF: IgG+ and IgM+ colloid bodies, ribbon-like fibrin deposits on the basement membrane.
Scarring neutrophilic alopecia
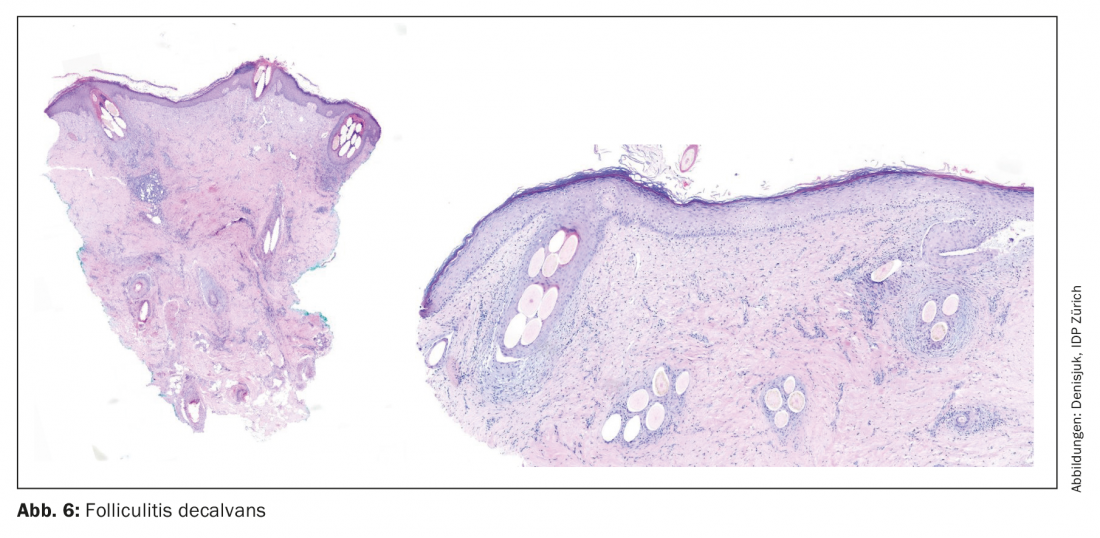
Folliculitis decalvans (FD)
S. aureus appears to play a role in the development of this disease in middle-aged adults primarily on the vertex in the form of papules, pustules, and tufts of hair.
Histologic:
Early stage
- Perifollicular neutrophil-rich infiltrates
Late stage
- Follicle rupture
- Dense peri- and intrafollicular plasma cell-rich infiltrates.
- wedge-shaped loss of elastic fibers around infundibulum
- fibrotic steles
- Polytrichy (Fig. 6)
Scarring mixed alopecia
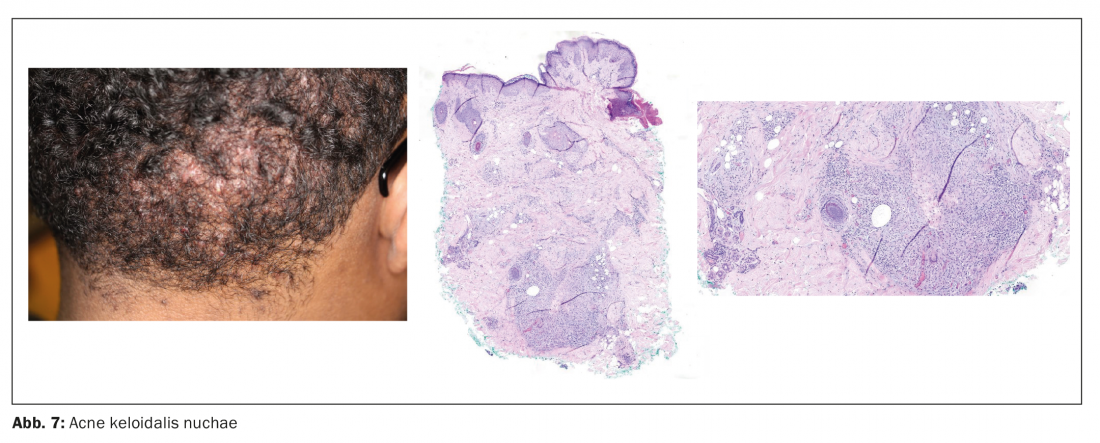
Acne keloidalis nuchae
- Acne keloidalis nuchae is mainly suffered by young men with dark skin type and frizzy hair. Papules, pustules later develop into scars and keloids on the neck and back of the head.
Histologic:
Early stage
- dilated follicles surrounded by neutrophilic infiltrate
Late stage
- ruptured hair follicles with exposed hair shafts surrounded by granulomatous and plasmocellular infiltrates and fibrosis (Fig. 7)
- Complete absence of sebaceous glands
Secondary alopecia
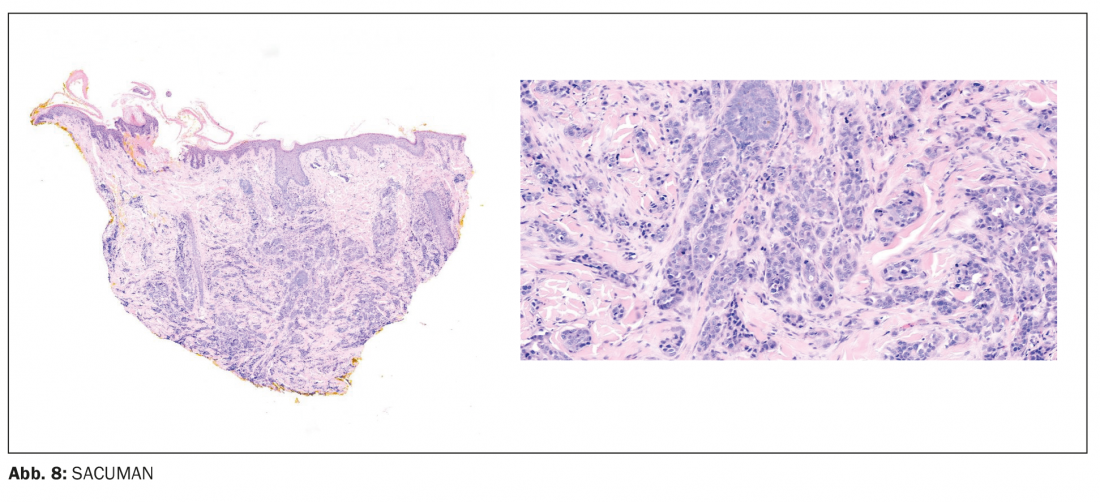
SACUMAN
- SACUMAN = scalp alopecia due to a clinically unapparent or minimally apparent neoplasm
- Hair loss without or with minor changes of the skin surface in the area of local benign (e.g. nevus sebaceus) and malignant neoplasms (e.g. Sézary syndrome) as well as in distant metastatic tumors (mostly in mamma ca., Fig. 8).
Take-Home Messages
- A hair base biopsy should ideally be taken from the periphery of an alopecic focus with preserved hair, in the direction of hair growth, with sufficient fat tissue, without squeezing.
- In the presence of non-scarring alopecia, collection of 2 specimens for vertical and horizontal section is still recommended.
- In case of suspicion of scarring alopecia, especially LE, LPP or FD, an additional direct immunofluorescence examination is very helpful for the correct diagnosis.
- In case of an atypical clinical picture of alopecia, sampling is always recommended, especially for alopecia neoplastica or SACUMAN.
Literature:
- Headington JT: Transverse microscopic anatomy of the human scalp. A basis for a morphometric approach to disorders of the hair follicle. Arch Dermatol 1984; 120(4): 449-456.
- Böer A, Hoene K: Transverse sections for diagnosis of alopecia? Am J Dermatopathol 2005; 27(4): 348-352.
- Du X, Li Z, Xu W, et al: Diagnostic value of horizontal versus vertical sections for scarring and non-scarring alopecia: a systematic review and meta-analysis. Eur J Dermatol 2016; 26(4): 361-369.
- Olsen EA, Bergfeld WF, Cotsarelis G, et al: Summary of North American Hair Research Society (NAHRS)-sponsored Workshop on Cicatricial Alopecia, Duke University Medical Center, February 10 and 11, 2001. J. Am. Acad. Dermatol 2003; 48: 103-110.
- Elston DM, Ferringer T, Dalton S, et al: A comparison of vertical versus transverse sections in the evaluation of alopecia biopsy specimens. J Am Acad Dermatol 2005; 53: 267-272.
Further reading:
- Palo S, Biligi DS: Utility of horizontal and vertical sections of scalp biopsies in various forms of primary alopecias. J Lab Physicians 2018; 10(1): 95-100.
- Scheinfeld N: Review of scalp alopecia due to a clinically unapparent or minimally apparent neoplasm (SACUMAN). Acta Derm Venereol 2006; 86(5): 387-392.
- Stefanato CM: Histopathology of alopecia: a clinicopathological approach to diagnosis. Histopathology 2010; 56(1): 24-38.
DERMATOLOGIE PRAXIS 2022; 32(1): 4-8