Behind therapy-resistant tendon overloads, there are often incorrect postures and muscular imbalances with dysfunctional movement patterns that have not been taken into account. Apart from the local examination, a brief orientational, static and dynamic examination is important. This does not take much time and provides valuable information for a targeted, holistic therapy. The more risk factors present, the more important multimodal therapy is, including local measures, ergonomics, posture and quality of movement. This increases the chances for a sustainable improvement. Using “Bio-Tensegrity”, increased awareness of healthy posture and tension can be taught. When patients understand this principle, they find it easier to make lifestyle changes and have the patience needed for treatment.
Tendon overload is one of the most common musculoskeletal complaints. Majority are the result of cumulative microtrauma that occurs with poor movement execution, and/or when repetitive motion or duration of holding activities in awkward positions exceeds tissue loading capacity.
Bad posture and imbalances
Bad posture and muscular imbalances with compensatory movement patterns creep in over years or have their origin in an injury. It takes time for this to lead to health problems. Tendon overload is strongly related to lifestyle [1]. The body shapes itself according to use, reflecting the postures and movements that are most often performed. In today’s world, there is increasing postural damage due to prolonged sitting, and recently even chronic smartphone use! Poor posture is associated not only with poorer physical health, but also with poorer emotional health.
Tendon overloads in practice
Typical examples of tendon overload in practice involve the extensor tendon plate of the forearm in tennis elbow, the rotator cuff tendon plate of the shoulder, or the tendon/fascia complex of the Achilles tendon and plantar aponeurosis. In athletes, for example, runner’s knee with tendinopathy of the iliotibial tract (“iliotibial band syndrome”, ITBS) is a frequent reason for consultation.
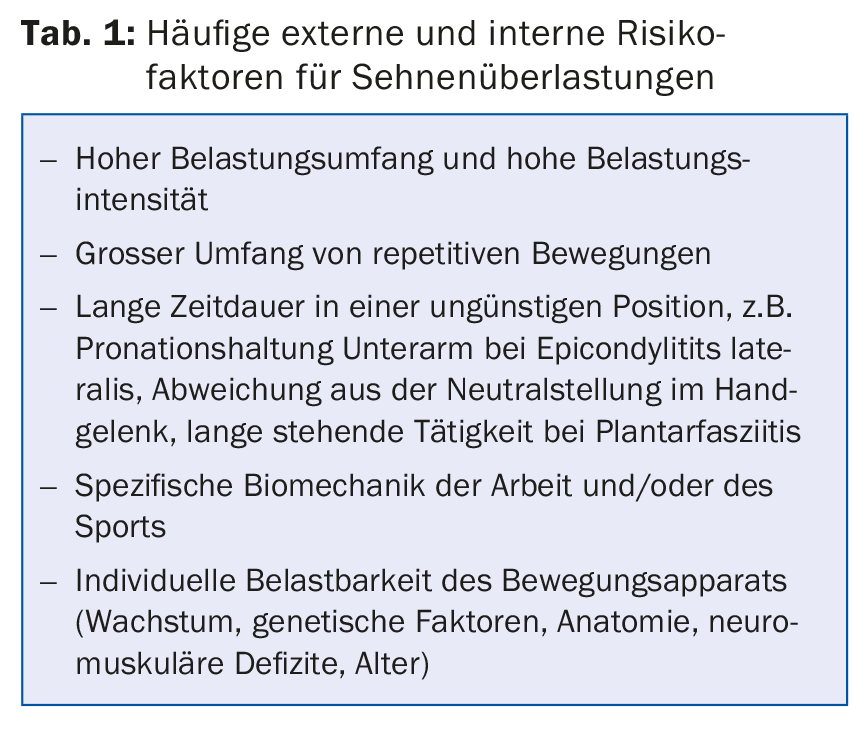
Correct structural diagnosis is usually not a problem if the clinic is typical. In the medical history, we look for common causes of tendon overload (Tab. 1) . In studies, it is usually only a combination of these factors that seems to increase the risk, e.g. of epicondylitis lateralis [2]. Only a somewhat extended examination of statics and dynamics provides additional clues for malpositions or movement disorders that are involved in the problem.
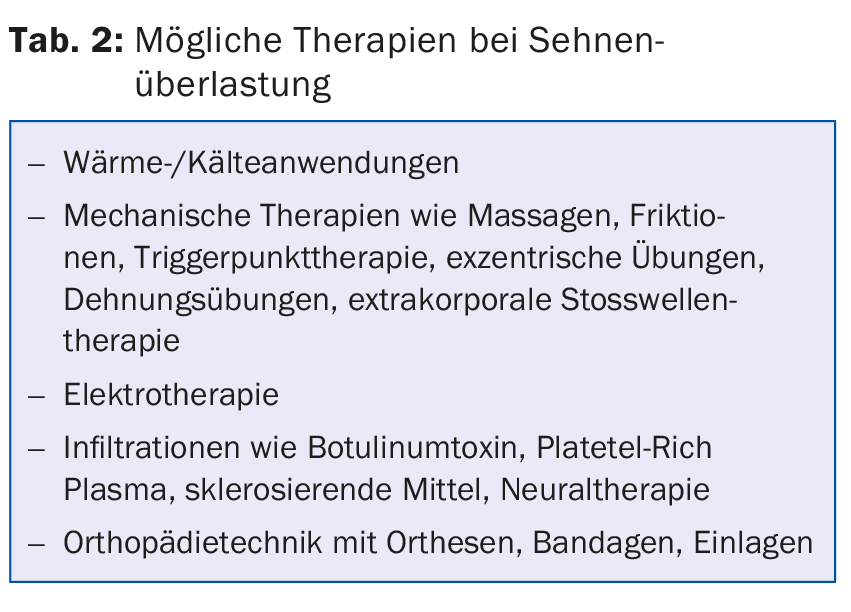
With regard to therapy, current studies focus on local therapy measures (Tab. 2). The goals are to improve blood circulation and the gliding ability of muscles, tendons and fascia, tendon regeneration and finally pain reduction and better resilience. However, one should be aware that the majority of these therapies are local symptomatic treatments. This does not treat a movement disorder or malposition involved in the tendon overload. If these factors are not taken into account in the therapy, the local therapy measure may not be effective or may not be sustainable. This leads to the question of what a physiological posture and movement execution is in the first place. “Tensegrity” and “bio-tensegrity” can provide an answer here.
Concept of kinetic chains and myofascial connections
“Tensegrity” refers to a building principle in architecture founded by Richard Buckminster Fuller in the 1960s. The term stands for “tensional integrity”. The balance of compression and tension is used to build structures. This leads to the fact that structures are lighter and stronger at the same time. An example of this construction method is the Kurilpa Bridge in Brisbane, Australia (Fig. 1) . It is the world’s largest structure based on this principle.

Tensegrity structures combine flexibility, resistance and strength with a minimum of energy and material input. The human musculoskeletal network can be considered a prime example of a “bio-tensegritiy” architecture (the term was founded by Dr. Stephen Levin). Physical stability is not based on the strength of individual tendons and muscles, but on the fact that forces are transmitted and distributed through the physical network. Physiologically, an increase in tension in a muscle/tendon unit is transmitted to the chain – provided that coordinative and neural control allow this and that transmission is not hindered by unfavorable statics or myofascial imbalances. If this principle does not work, local overload occurs.
Practical meaning
The detailed recording of external and physical risk factors for overexertion can be quite laborious. In practice, there is often not enough time for this. However, at least in the case of stubborn progressions, it is worthwhile to take a brief look at the physical statics and perform a short dynamic examination. The results help to decide whether more holistic therapeutic approaches should be initiated in addition to local measures. Gross misstatics and imbalances with unfavorable external, e.g. occupational, factors increase the risk for protracted courses.
The therapeutic technique used to modify the dysstatics and dysbalance is of secondary importance, be it classical physiotherapy, osteopathy, Rolfing or body-centered movement therapies such as yoga, Feldenkrais and Alexander Technique. The goal is to balance physical (and sometimes emotional) imbalances with improved postural and movement quality so that forces and tensions are more evenly distributed as intended by the physical network. The following two examples are intended to provide a brief overview without claiming to be exhaustive.
Tennis elbow or epicondylitis lateralis
In tennis elbow (epicondylitis lateralis or “wrist extension with forearm pronation syndrome” according to Shirley Sahrmann [1]), there is pain over the epicondylus lateralis, sometimes with radiation into the forearm. Grasping (e.g., holding a cup), repetitive grasping (playing tennis, working with pruning shears), or prolonged posture with wrist extension-forearm pronation-elbow flexion (working at a computer keyboard) are particularly painful. The 30- to 50-year-old age group is more frequently affected than younger and older people [2]. The course is usually self-limiting (18-24 months).
Pathophysiology: Anatomically-histologically, the overload mostly affects the extensor carpi radialis longus and brevis. Functionally, the extensors are overused and the biceps brachii and supinator are underused. Very often the scapula is at the center of the imbalance, so it should always be examined! Four major muscles stabilize and center the scapula, allowing efficient transmission of force from the spine to the hand (the scapula is also called the greater sesamoid bone). If this kinetic chain is disturbed, local overloads occur, typically in the shoulder, elbow or wrist.
Inspection and dynamics: finger and wrist extensors are better developed than the biceps brachii. Typically, there is a thoracic hyperkyphosis, shoulder and head protraction, and a malposition of the scapula.
- Have the patient abduct and lower the arms in slow motion: insufficient stabilization and dyskinesia of the scapula is evident.
- Have the patient perform a grasping motion: It shows too early rotation of the humerus when the forearm pronates.
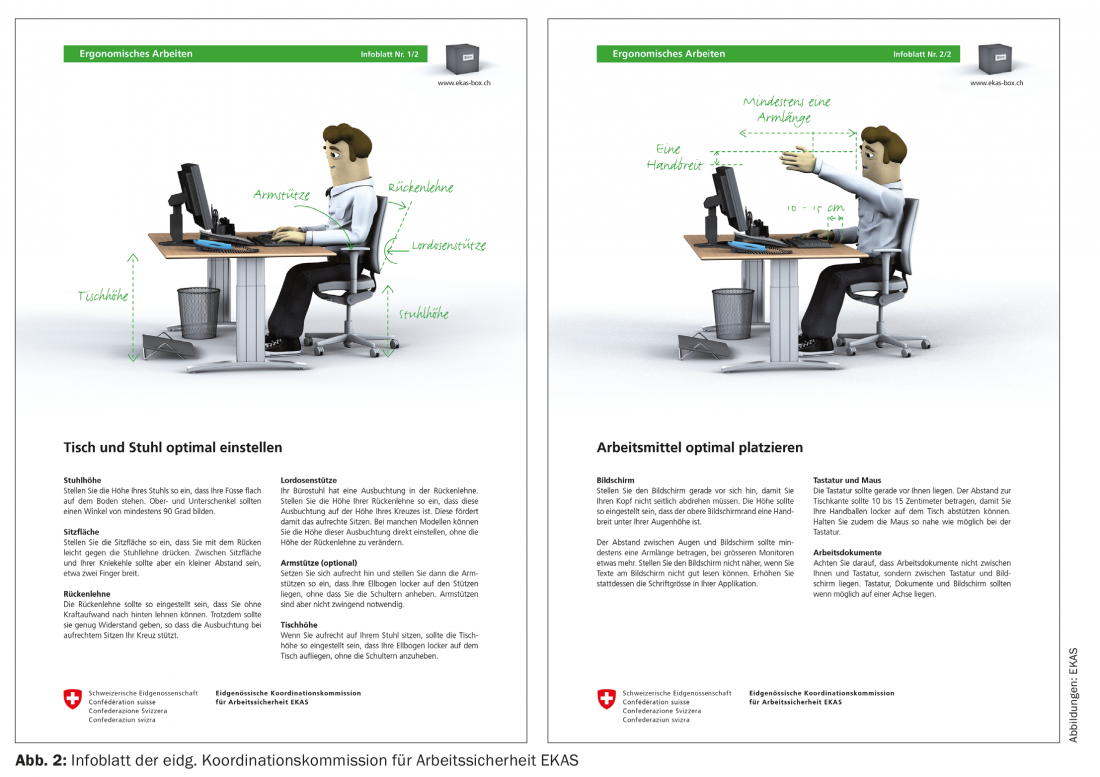
- Have the patient demonstrate his working posture, e.g., at an office desk: The typical malposition with thoracic spine hyperkyphosis, shoulder/head protraction, wrist extension, forearm pronation, and elbow flexion can be seen.
Therapy: Therapy is intended to modify unfavorable posture and movement patterns so that the stress on the damaged tissue decreases. Accordingly, the patient must be informed about the underlying problem and instructed about ergonomics (Fig. 2) . Implementation in everyday life requires a great deal of commitment on the part of the patient. This is only possible if he understands the bigger picture.
Plantar fasciitis
In plantar fasciitis (“pronation/supination or insufficient talocrural dorsiflexion syndrome” according to Shirley Sahrmann [1]), there is pain at the medial tuber calcanei. The pain occurs under stress and rarely radiates to the plantar fascia. Plantar fasciitis is more common in people with sedentary jobs than in athletes. The course is usually self-limiting (6-18 months). A heel spur is more commonly found with plantar heel pain.
Pathophysiology: The pathophysiology is quite complex. In addition to faulty statics and muscular imbalances, factors we still know little about probably play a role. Mechanical loading alone does not adequately explain degenerative tendon changes. Predisposing factors are discussed such as neuromuscular deficits of the intrinsic foot musculature leading to overload of the plantar aponeurosis and genetic factors such that normal loads are not tolerated and accelerated degeneration of the plantar aponeurosis is favored. Combined with extrinsic factors such as excessive or unaccustomed stress/sport, mostly standing activity or inadequate footwear, the stress capacity is finally exceeded, so that tissue changes are initiated and pain develops. Unfavorable intrinsic aggravating factors such as arch type, limited dorsiflexion in the ankle, poor cushioning properties of the heel fat pad, obesity, and age also play a role. However, these may have nothing to do with the development, but more influence the pain intensity [3].
Statics and dynamics: Shirley Sahrmann distinguishes three different syndromes that can affect the plantar fascia [1]: The pronation type with a yielding, weak medial arch in the sense of an articulated foot, the supination type with a rather high, rigid arch and poor shock absorption, and the type with limited dorsiflexion in the upper ankle joint (OSG) due to shortening of the foot flexors, often associated with Achilles tendinopathy. In addition to these three foot types, look for evidence of increased tone of the dorsal myofascial chain, such as lumbar spine hyperlordosis and/or shortening of hamstrings and calf muscles. Single-leg squats and jumps, as well as single-leg toe stands, show limited mobility in the OSG, deviation of the leg axis and the dynamics of the arch of the foot, and, at most, a lack of physiological hindfoot inversion in the toe stand. Grasping a cloth from the floor with the toes shows deficits of the intrinsic foot muscles.
Therapy: In addition to any local measures, therapy has the task of modifying imbalances. Factors that have an unfavorable effect on pain intensity should also be taken into account and treated, e.g. with supportive insoles in pronation/ankle foot or arch support and heel cushioning in hollow foot to increase the bearing surface and improve shock absorption of the heel. It is also important to reduce weight if you are overweight. Further measures are instructed stretching exercises and massages of the plantar fascia with a tennis ball in the evening before sleeping and in the morning before getting up.
Literature:
- Sahrmann S, et al: Movement System Impairment Syndromes of the extremities, cervical and thoracic spine. Elsevier 2011.
- Fan ZJ, et al:. The association between combination of hand force and forearm posture and incidence of lateral epicondylitis in a working population. Human Factors 2014; 56(1): 151-165.
- Waering S: Chapter 5.9, Anatomy of the plantar fascia. From: Schleip R, et al. Fascia, the tensional network of the human body. Churchill Livingstone 2012.
HAUSARZT PRAXIS 2016; 11(4): 20-23