It is clear that coordinated exchange between hospitals and primary care physicians is fundamental to the functionality of the health care system. But how can the interfaces between the two areas be better coordinated? Which communication channels are most effective? PD Dr. med. Manuel Fischler, head of the medical clinic at the Waid City Hospital, Zurich, and Dr. med. Gerhard Schilling, specialist in general medicine, Stein am Rhein, presented various options at the KHM Congress in Lucerne.
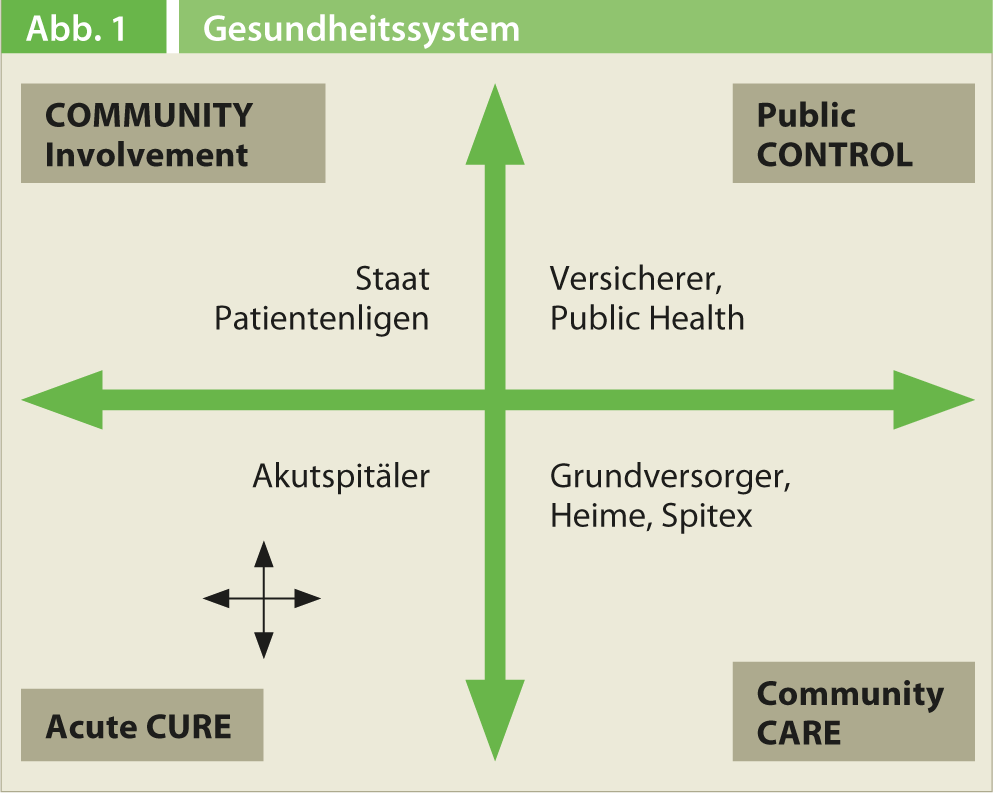
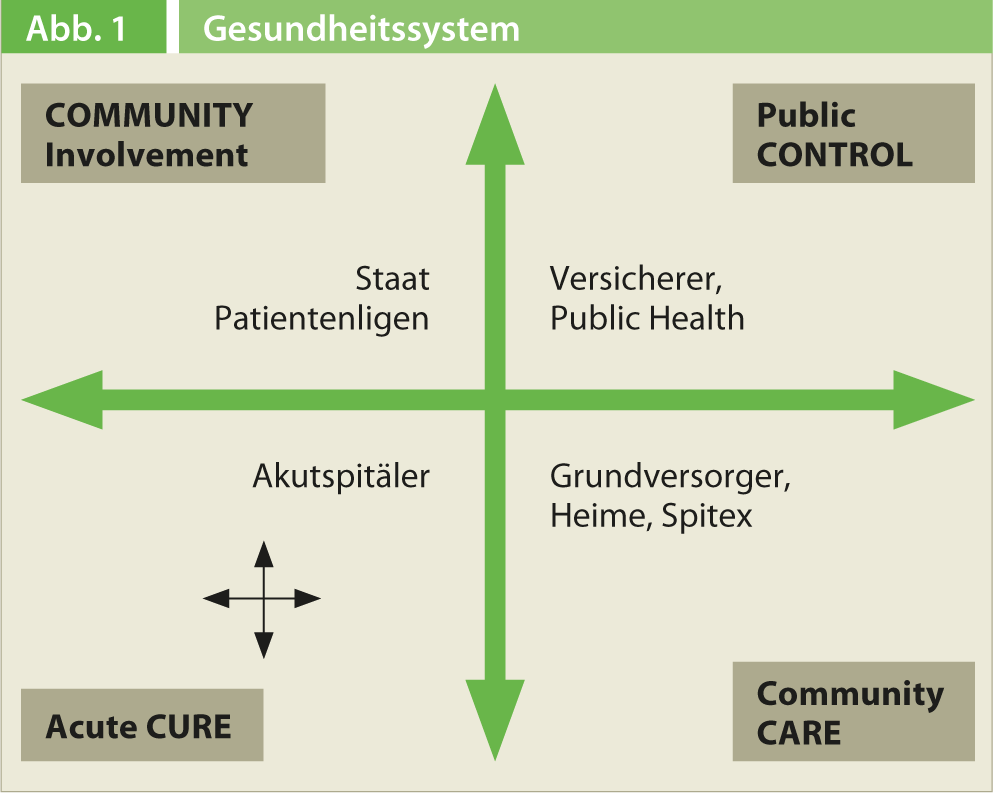
PD Dr. med. Manuel Fischler, Chief Physician of the Medical Clinic at the Waid City Hospital, Zurich, first addressed the question of where interfaces between hospitals and primary care providers exist at all. In model terms, the medical profession includes two components: Cure and Care. The physicians of a hospital are more likely to be in the Cure area, while the nurses take over the Care processes. In the higher-level health care system, the two areas of responsibility also exist. Hospitals and primary care providers both perform acute Cure processes. Family physicians are also more active in the community care sector than hospitals: The phases of patient care are significantly extended.
The fields of activity cannot be clearly separated from each other, because the tasks of the hospital and the primary care providers overlap(Fig. 1). Therefore, ways must be found to optimize and coordinate communication at the interfaces.
This seems to be exactly a problem: recent studies for Switzerland show that coordination problems occur in 32% of patients with two or more chronic diseases. Specifically, this refers to the following situations: the primary care physician does not have the test results available at the time of the consultation, receives conflicting information from different specialists, or orders a test that has already been performed. In 2011, the Organization for Economic Co-operation and Development (OECD) therefore concluded that although the Swiss healthcare system functions very successfully in many respects, reforms are needed to establish the coordination of the various medical services in a stable manner over the long term.
Three dimensions
According to Dr. Fischler, the interfaces between outpatient and inpatient care can be looked at from three points of view:
- First, smooth continuity in the therapeutic treatment chain must be achieved. Information exchange (especially exit/referral reports) must not falter.
- Secondly, the same continuity is needed in the transition to nursing follow-up and care by Spitex. The hospital should involve Spitex services early in the consultation.
- Thirdly, the financial and social framework is of great importance.
Forms of exchange
Dr. Fischler sees many advantages in an intensified exchange between general practitioners and hospitals: “This is necessary because chronic diseases and thus changes from outpatient to inpatient therapy are becoming more frequent. The increasing complexity of treatments calls for interprofessional cooperation. Last but not least, a more efficient exchange between family doctor and hospital makes a valuable contribution to cost containment in the healthcare system.” The basis of such efforts is the willingness of the players involved to cooperate. If it is given, it still needs the appropriate framework conditions. The implementation of e-health could serve as an important tool for data sharing. Only a stable, universally accepted communication channel enables a regulated exchange between different healthcare institutions.
The question of which tools should be used to communicate at all also occupied the workshop participants. How reliable and clear are email contacts? People often forget to upload the necessary documents to the attachment, which leads to a long delay in the exchange of information. What role does the telephone play? Many physicians are simply unavailable or have little time for phone calls. The solution would be (in the sense of e-health) a cross-cantonal electronically accessible data platform, where the billions of documents are clearly organized and can be accessed at any time.
“There are already referring portals that provide a common entry point for the flood of data,” Dr. Fischler pointed out. Patient information can be accessed and edited electronically there. In the future, downstream organizations such as care centers could also be connected. Such platforms are well received by physicians. Further efforts in this area are therefore desirable, according to Dr. Fischler and Dr. Schilling.
Source: “Exchange GP and Hospital,” workshop at the 15th Continuing Education Conference of the College of Family Medicine (KHM), June 20-21, 2013, Lucerne.