Inflammatory chronic back pain is an indication of possible axial spondyloarthritis. For primary care physicians, identifying those with axial spondyloarthritis among the many back pain patients is a major challenge. Studies show that the average latency to diagnosis is several years. This has a negative impact on a number of levels. An international steering committee has now prepared a problem analysis with the aim of improving the current situation for those affected.
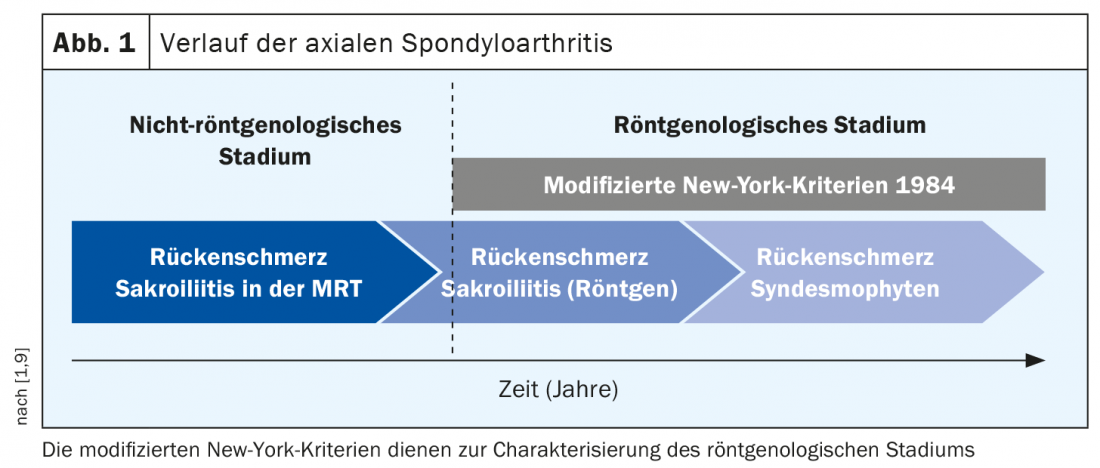
According to the 2019 update of the S3 guideline Axial spondyloarthritis (axial SpA), the median time of diagnostic latency is between 5 and 14 years [1]. One of the reasons given for this is that it is not a single symptom that points the way to a diagnosis, but rather the presence of additional disease features in patients with nonspecific low back or back pain that must be correctly classified. Chronic back pain (>3 months) is a key symptom in patients with axial SpA. In the US National Health and Nutrition Examination Survey (NHANES), the prevalence of inflammatory back pain in the general population ranged from 5-6% [2]. In a cohort of patients with inflammatory back pain that had been present for less than 2 years, 20% of patients already had structural changes in the sacroiliac joints [3].
Criteria according to ASAS (Assessment of SpondyloaArthritis International Society)
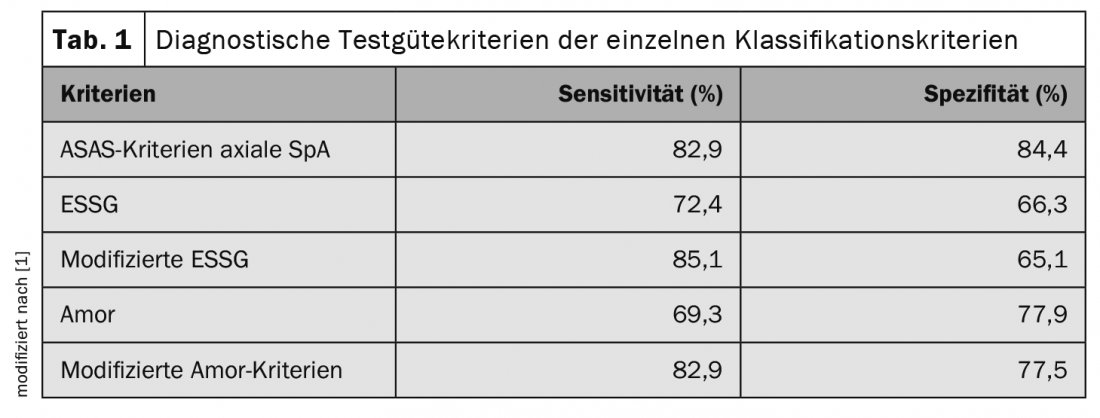
Identifying whether inflammatory chronic back pain is present and in which cases further workup is required proves to be nontrivial in clinical practice. Among other things, this is also attributed to heterogeneous classification systems. According to the Assessment of SpondyloArthritis international Society (ASAS), chronic back pain ≥3 months and age <45 years at symptom onset are criteria for further evaluation of a suspected diagnosis of axial SpA. In addition to certain features on imaging (sacroiliitis on imaging plus ≥1 other SpA criterion), laboratory diagnostic HLA-B27-positive findings plus ≥2 other SpA criteria are also diagnostic indicators of the presence of SpA. The criteria have a sensitivity of 82.9% and a specificity of 84.4% when the entire set is tested. If only the diagnostic imaging bundle was tested, the sensitivity is 66.2% and the specificity is 97.3% before [4,5].
The specificity is thus better for the ASAS classification criteria than for the Amor and ESSG criteria (Table 1). In a longitudinal study, the positive predictive value of the ASAS criteria for axial SpA was 93.3% [6,7]. The ASAS classification criteria refer to the entire group of patients with axial SpA, that is, both patients without and those with structural changes in the sacroiliac joints. The former is referred to as nonradiographic axial SpA (nr-axSpA).
“Delay to Diagnosis” Report – International Appeal
The Axial Spondyloarthritis International Federation has produced a comprehensive evidence-based review with an analysis of possible reasons for diagnostic latency in axial SpA. Formerly known as the International Map of Axial Spondyloarthritis, the organization’s goal is to highlight the negative effects of a diagnostic delay and develop proposed solutions. At the EULAR Annual Meeting 2021, Dr. Dale Webb and colleagues reported their findings and appealed to health system leaders in various countries to address this issue with a view to improving the situation for those affected [8]. A total of 92 stakeholders from 23 countries on five continents participated in the EULAR Congress events.
The “Delay to Diagnosis” report provides, among others, the following explanations for the current international average estimated diagnosis latency of 7 years:
- insufficient “awareness” of axial SpA in persons with corresponding symptoms
- lack of recognition of the symptomatology in the general population
- incorrect diagnosis at low-threshold medical contact points
- unclearly defined criteria for referral to specialists
According to the S3 guideline, the goal of early diagnosis in patients with axial SpA is to ensure the best possible treatment in a timely manner and to avoid unnecessary diagnostic investigations and non-indicated therapies. The overriding goal is to prevent structural damage, avoid loss of function and the associated negative effects for those affected [1].
Congress: EULAR Annual Meeting 2021
Literature:
- Kiltz U, et al: Long version of the S3 guideline Axial spondyloarthritis including ankylosing spondylitis and early forms, update 2019. Z Rheumatol 2019; 78: 3-64.
- Weisman MH, Witter JP, Reveille JD: The prevalence of inflammatory back pain: population-based estimates from the US National Health and Nutrition Examination Survey, 2009-10. Ann Rheum Dis 2013; 72(3): 369-373.
- Heuft-Dorenbosch L, et al: Performance of various criteria sets in patients with inflammatory back pain of short duration; the Maastricht early spondyloarthritis clinic. Ann Rheum Dis 2007; 66(1): 92-98.
- Rudwaleit M, et al: The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 2009; 68(6): 777-783.
- Aydin SZ, et al: Validation of the ASAS criteria and definition of a positive MRI of the sacroiliac joint in an inception cohort of axial spondyloarthritis followed up for 8 years. Ann Rheum Dis 2012; 71(1): 56-60.
- Sepriano A, et al: Predictive validity of the ASAS classification criteria for axial and peripheral spondyloarthritis after follow-up in the ASAS cohort: a final analysis. Ann Rheum Dis 2016; 75(6): 1034-1042.
- Molto A, et al: Performances of the Assessment of SpondyloArthritis International Society axial spondyloarthritis criteria for diagnostic and classification purposes in patients visiting a rheumatologist because of chronic back pain: results from a multicenter, cross-sectional study. Arthritis Care Res (hoboken) 2013; 65(9): 1472-1481.
- “There is an Unacceptable Delay to Diagnosis in Axial Spondyloarthritis,” EULAR Annual Meeting, 04/06/2021.
- Rudwaleit M, et al: The challenge of diagnosis and classification in early ankylosing spondylitis: do we need new criteria? Arthritis Rheum 2005; 52(4): 1000-1008.
HAUSARZT PRAXIS 2021; 16(7): 18-19 (published 6/28-21, ahead of print).