In antihypertensive therapy in the 80-plus age group, it is important to weigh risk and benefit individually and not to treat strictly according to target values. Frailty (“frailness”) is an important concept in clinical practice. Particularly in those over 80 years of age with hypertension and comorbid conditions, blood pressure reduction is guided by general health, including any comorbidities and polypharmacy. In addition to empirical findings, physician clinical experience and patient opinion must also be considered.
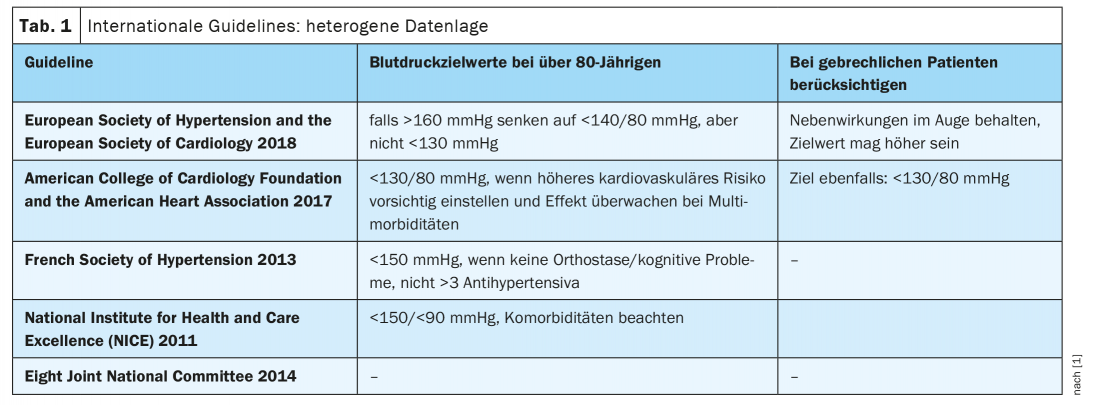
Very elderly frail people with multimorbidity are often excluded from large randomized-controlled trials. “If these patients are missing from studies, they are also missing from the guidelines,” explains Prof. Dr. med. phil. Sven Streit, Head of Interprofessional Primary Care, Bern Institute of Family Medicine, on the occasion of this year’s Virtual Medical Congress Arosa [1]. A comparison of hypertension treatment guidelines from different countries shows that recommendations of blood pressure targets for people over 80 years of age are inconsistent and not all guidelines take this age group into account (tab. 1) . Experience shows that patient-centered blood pressure therapy has proven effective in this subpopulation of hypertensives, according to Prof. Streit.
Consider not only biological age, but also general condition
Large randomized trials of the effect of blood pressure reduction in the very elderly are only partially transferable to a “real world” setting. For example, the SPRINT trial included 2636 patients over 75 years of age, but diabetes, heart failure, orthostasis, and history of stroke were among the exclusion criteria [2]. However, these are patient characteristics that are associated with a higher risk of side effects, making it particularly important to weigh the benefits and risks of antihypertensive therapy. In this respect, the results of this study, which state that a target systolic value <120 mm Hg* compared with a target systolic value <140 mm Hg** resulted in a 33% reduction in all-cause mortality, should be viewed critically. This is also true for the results of the HYVET study, which investigated blood pressure therapy in patients over 80 years of age. However, due to the exclusion criteria, the sample incompletely represents the “frailty” concept relevant to patients in this age group treated in family practice [3].
* effectively achieved target value = 123 mmHg
** Effective target value achieved = 135 mm Hg
Cohort studies as an important data source
Population-based cohort studies, which include a sample more representative of the overall population, are therefore an important source of data. One such cohort is the Leiden 85-plus cohort, which included 570 over 85-year-old residents of Leiden (NL) [5]. Data analyses revealed, among other things, that a systolic blood pressure in the range of 120 mmHg achieved by antihypertensives was associated with a higher risk of falls compared with a systolic value around 140 mmHg. It was also shown that the risk of memory impairment (Mini-Mental Status Examination, MMSE) was increased when taking antihypertensives [5]. While randomized-controlled trials are subject to selection bias due to inclusion/exclusion criteria, the lack of randomization must be considered when interpreting results from cohort studies.
“Frailty” and comorbidities are relevant for blood pressure target
In the daily practice of family physicians, a variety of factors must be considered when treating hypertension in the elderly, including advanced atherosclerotic vascular disease, impaired renal function, increased tendency to orthostatic hypotension, as well as frailty and polypharmacy. Close monitoring in the practice is advisable, especially at the beginning of therapy. According to Prof. Streit [6], visual diagnosis or gut feeling or assessment procedures such as the “up-and-go test” have proven effective in assessing the frailty of patients.
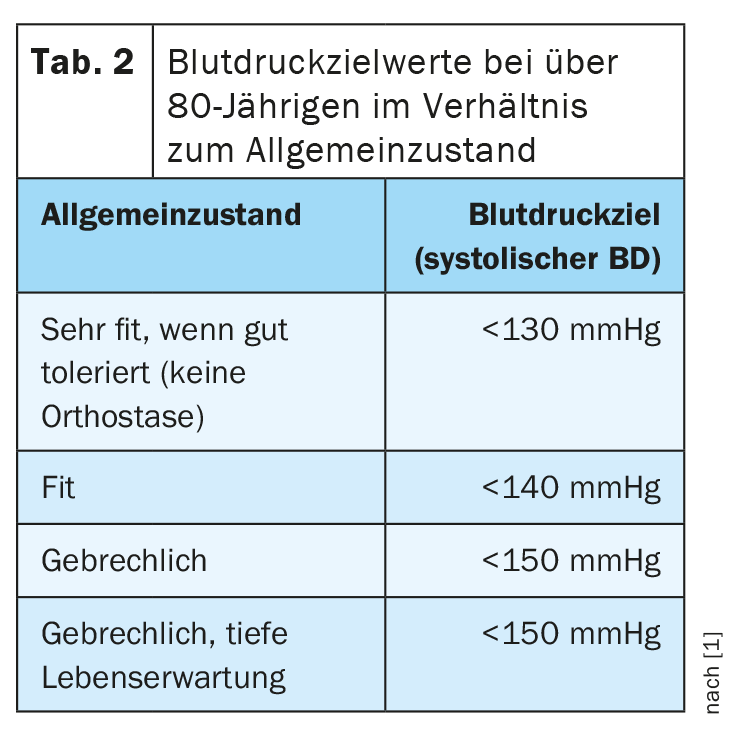
Table 2 presents indications for target systolic values in people older than 80 years, taking into account general health. These data are based on an integration of clinical experience and empiricism. Accordingly, for a very fit patient from this age group, a blood pressure reduction to a value of <130 mmHg tends to be reasonable, whereas for a frail patient from the same age group, a target value of <150 mmHg may be sufficient. The speaker used case studies to illustrate individualized blood pressure therapy. Whereas in an 82-year-old frail male patient with various comorbidities (type 2 diabetes mellitus, obesity, limitations of cognition), a target systolic value in the range of 141-150 mmHg, a target value in the range 131-140 mmHg would be more appropriate for an 82-year-old frail patient who, in addition to obesity and cognitive impairment, had suffered a stroke two years ago. mmHg should be aimed for, the speaker explains.
Literature:
- Dispute S: Is deeper always better? Hypertension treatment in elderly patients, Prof. Dr. Sven Streit, Ärztekongress Arosa, 26.03.2021
- Williamson JD, et al: Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged >75 years: a randomized clinical trial. JAMA 2016; 315: 2673-2682. doi: 10.1001/jama.2016.7050.
- Warwick J, et al: No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled trial of antihypertensives in people with hypertension aged 80 and over. BMC Med 2015; 13; 78.
- Streit S, et al: Variation in GP decisions on antihypertensive treatment in oldest-old and frail individuals across 29 countries. BMC Geriatr 2017; 17(1): 93.
- Streit S, et al: Lower blood pressure during antihypertensive treatment is associated with higher all-cause mortality and accelerated cognitive decline in the oldest-old. Data from the Leiden 85-plus Study, Age and Ageing 2018; 47(4): 545-550.
- Pangilinan J, et al: The Timed Up and Go Test as a Measure of Frailty in Urologic Practice. Urology 2017; 106: 32-38.
- European Society of Cardiology: 2018 ESC/ESH Clinical Practice Guidelines for the Management of Arterial Hypertension, www.escardio.org/Guidelines (last accessed 04/23/2021).
- Reeve E, et al: Withdrawal of antihypertensive drugs in older people. Cochrane Database of Systematic Reviews 2020, Issue 6. art. No.: CD012572.
HAUSARZT PRAXIS 2021; 16(5): 26-27 (published 5/5/21, ahead of print).











