In recent years, numerous new glucose-lowering agents have been developed. SGLT-2 inhibitors and GLP-1 receptor agonists have demonstrated cardiovascular and nephroprotective effects in large clinical endpoint studies. The variety of available antidiabetic drugs represents a major advance in therapeutic options, but also makes the selection of the individually appropriate drug increasingly challenging. Evidence-based recommendations are provided by the ADA/EASD guidelines, among others.
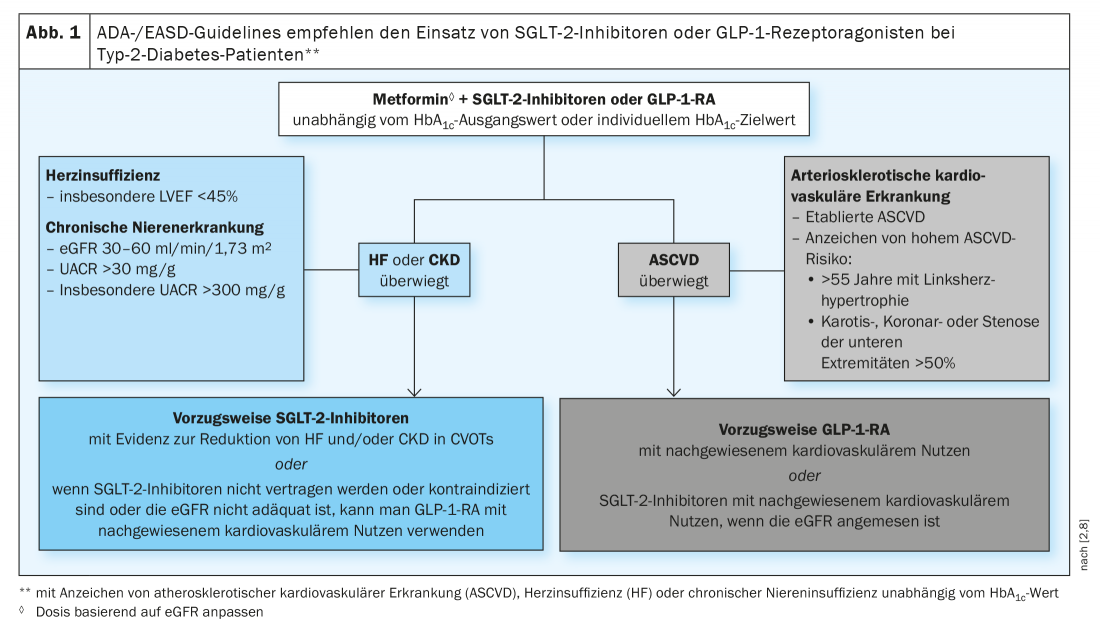
The different cardio- and nephroprotection profiles of SGLT-2 inhibitors and GLP-1 receptor agonists (GLP-1-RA) have already been incorporated into many current guidelines for the treatment of T2DM by citing specific patient characteristics for which one or the other class of compounds is most appropriate [1]. Thus, based on the results of the large cardiovascular outcomes trials (CVOTs), the following three changes were incorporated into the latest revision of the ADA/EASD treatment recommendations [1–3] (Fig. 1) :
- In patients at high cardiovascular risk, treatment with a GLP-1 RA or an SGLT-2 inhibitor should be considered, regardless of baseline HbA1c or individual HbA1c target, to reduce the risk of major adverse cardiovascular events (MACE), hospitalization for heart failure (hHF), cardiovascular death, or chronic renal failure (CKD). In other words, due to the properties of these agents, the goal of pharmacological therapy is not only to provide individualized glycemic control but also to address organ damage more directly [4], as recommended with great emphasis in the most recent guidelines for diabetes, prediabetes, and cardiovascular disease of the European Society of Cardiology (ESC) [5].
- Furthermore, the ADA/EASD consensus report suggests that GLP-1-RA should also be considered in patients with type 2 diabetes without established cardiovascular disease who have specific factors for high cardiovascular risk [2].
- Finally, SGLT-2 inhibitors are recommended in T2DM patients with heart failure, particularly HFrEF, to reduce the risk of mortality due to hHF, MACE, and CVD, and for type 2 patients with chronic renal failure* to reduce both the progression of chronic kidney disease and the risk of hHF, MACE, and cardiovascular death.
* estimated GFR 30 to ≤60 mL/min/1.73 m2 or albumin-creatinine ratio in urine >30 mg/g, resp. especially if >300 mg/g
All these indications are based on the additional benefits of these substance classes, which have been demonstrated in the CVOTs. However, there are other possible aspects that may help to identify factors to optimally adapt the treatment strategy to the respective T2DM patients. This requires a better understanding of the mechanisms of action of SGLT2 inhibitors and GLP1-RA in relation to specific pathophysiological mechanisms [1].
Mechanisms of action of SGLT-2- inhibitors and GLP1 receptor agonists.
SGLT-2 inhibitors lower blood glucose levels via increased glucose excretion in the urine. Insulin requirements are reduced and long-term blood glucose (HbA1c) is reduced [6]. In addition, these preparations also protect the cardiovascular system and kidneys. Kidney withdrawal of glucose and sodium has a diuretic effect. As with other diuretic medications, this is associated with a reduction in blood pressure. Due to the antihypertensive effect and the drainage of the body, a relief of the heart is also brought about and the filtration pressure in the renal corpuscles is reduced. This nephroprotective effect counteracts the development of diabetic nephropathy. If albuminuria is noted, which is the first indication of renal impairment in diabetes, it is reasonable to consider the use of an SGLT-2 inhibitor. SGLT-2 inhibitors can delay the onset of diabetes-related renal impairment and slow the progression of existing renal disease [6]. If diabetic kidney damage is not recognized and treated in time, the risk of progressive renal function loss increases, which can lead to renal insufficiency requiring dialysis. Sparing the kidneys and reducing protein loss in the urine are also associated with a reduced risk of cardiovascular diseases such as myocardial infarction and stroke [6].
GLP-1 receptor agonists (GLP-1-RA) have been an integral part of the treatment of type 2 diabetes for years due to their multifactorial mode of action. Like the natural peptide hormone GLP-1, they bind to the GLP-1 receptor, promote insulin secretion and inhibit glucagon release. These blood glucose-lowering agents have also been shown to have additional cardiovascular benefits, among others. They are associated with a reduction in the risk of cardiovascular events and may lead to improvements in left ventricular ejection fraction as well as myocardial contractility, coronary blood flow, and endothelial function [7]. Other functions of GLP-1 include increased glucose uptake in muscle, decreased glucose production in the liver, and a more rapid feeling of satiety as a result of direct action on the hypothalamus. Therefore, this substance class is also suitable for weight reduction in overweight patients. Other known effects include a reduction in systolic and diastolic blood pressure and cholesterol levels [7].
Literature:
- Dardano A, et al: Invited review. Series: Implications of the recent CVOTs in type 2 diabetes. Which patients for GLP-1RA or SGLT-2 inhibitor? Editorial, Diabetes Research & Clinical Practice 2020; 162: 108112, April 1, 2020, www.diabetesresearchclinicalpractice.com
- Buse JB, et al: 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2020; 43(2): 487-493. doi: 10.2337/dci19-0066.
- Davies MJ, et al: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018; 41(12): 2669-2701.
- Avogaro A, et al: Continued efforts to translate diabetes cardiovascular outcome trials into clinical practice. Cardiovasc Diabetol. 2016; 15: 111, https://doi.org/10.1186/s12933-016-0431-4
- Cosentino F, et al; ESC Scientific Document Group. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 2020; 41(2): 255-323. doi: 10.1093/eurheartj/ehz486
- d-journal: SGLT2 inhibitors: more than just lowering blood glucose, www.d-journal.ch/diabetes-aktuell/sglt2-hemmer-mehr-als-nur-blutzuckersenkung
- Collins L, Costello RA: Glucagon-like Peptide-1 Receptor Agonists, StatPearls [Internet], www.ncbi.nlm.nih.gov/books/NBK551568
- Mohebbi N: New options for the treatment of diabetic nephropathy – “the new kid on the block”, PD Nilufar Mohebbi MD, FomF (WebUp), 8/27/2020.
HAUSARZT PRAXIS 2020; 15(12): 18-20











