In cases of chronic genital symptoms and exclusion of infectious causes, early biopsies should be taken to exclude genital precancerous lesions. Lichen sclerosus should be considered a facultative precancerous condition. In HPV-induced carcinoma in situ, other sexually transmitted infections should be considered, as should partner testing.
Genital precancerous lesions often present as nonspecific findings and are a diagnostic challenge. They can be difficult to distinguish from benign lesions. Late presentation with a history of independent frustrated attempts at therapy over an extended period of time may mean that invasive carcinoma is already present at diagnosis.
Risk factors
Diverse behavioral patterns and anatomical conditions result in an increased individual risk for the formation of genital precancerous lesions. These are the presence of a prepuce, phimosis, lack of hygiene, older age, smoking, chronic inflammation and promiscuity. However, the most important risk factor for genital precancerous lesions is infection with different types of human papilloma virus (HPV).
Division
The genital precancerous lesions can be broadly divided into HPV-associated genital precancerous lesions and non-HPV-associated genital precancerous lesions.
With the exception of Paget’s disease, the non-HPV-associated genital precancerous lesions are chronic inflammatory conditions that do not primarily involve dysplastic cells but can only lead secondarily to changes in the overlying epithelium and thus to squamous cell carcinoma.
Among HPV-associated genital precancerous lesions, Condylomata gigantea Buschke Löwenstein is primarily associated with low-risk HPV types 6 and 11, whereas erythroplasia Queyrat, Bowen’s disease, and Bowenoid papulosis are associated with high-risk HPV types 16 and 18.
Furthermore, a classification can be made into precancerous lesions in the narrower sense and those in the broader sense. The precancerous lesions in the narrower sense are characterized by a histological tissue picture with epithelial dysplasia of varying degrees up to carcinoma in situ. Naming is based on the location of the intraepithelial dysplastic changes. Analogous to vulvar intraepithelial neoplasia (VIN), the terms penile intraepithelial neoplasia (PeIN) and anal intraepithelial neoplasia (AIN) are also used. These are squamous dysplasias in the sense of carcinomata in situ, usually caused by HPV infections. Precancerous lesions in the broader sense are chronic inflammatory dermatoses that may be followed by secondary dysplastic changes of the epithelium.
Non-HPV-associated genital precancerous lesions.
Lichen sclerosus: Manifests primarily on the glans penis, prepuce, or around the introitus vaginae, is one of the non-HPV-associated genital precancerous lesions. If left untreated, invasive carcinomas can occur in approximately 10% of patients within one to eight years.
In men, lichen sclerosus often manifests between the ages of 30 and 40, while in women it shows two age peaks. On the one hand, in prepuberty as a child, with spontaneous remitting at puberty; the second peak of manifestation is around the age of 60. Lichen sclerosus initially presents with nonspecific symptoms such as itching or pain. Later, the typical picture of sclerosed areas and hemorrhages appears (Fig. 1).

Therapeutically, high-potency local steroids are primarily used. Clobetasol propionate, mometasone furoate, and pimecrolimus are the most likely to be recommended based on current data. Since lichen sclerosus is a facultative precancerous condition, regular follow-up should be performed with regard to possible squamous cell carcinoma. Patients should consult the physician for persistent keratoses or nodules.
Paget’s disease: The clinical picture of extramammary Paget’s disease is very close to Bowen’s disease, but the latter is much more common than Paget’s disease. Differentiation is possible histologically in every case. It should be noted the coincidence of Paget’s disease with other carcinomas, such as those of the vaginal cavity, cervix, rectum and mamma, which, according to statistics, amounts to a frequency of 20%, including the association of Paget’s disease of the nipple with that of the vulva. The neoplastic cells of Paget’s disease are mucin-producing adenocarcinoma cells. A classification into apocrine or eccrine gland duct structure cannot be given for Paget cells.
HPV-associated genital precancerous lesions.
Bowen’s disease, erythroplasia Queyrat, VIN, PIN, AIN: Erythroplasia Queyrat is the manifestation of Bowen’s disease at the glans penis and is found at the non-keratinizing squamous epithelium and is thus located at the glans penis or in the inner preputial leaflet in men. In women, erythroplasia queyrate is much less common and is found in the vagina. Most commonly, this presents as an indolent, sharply demarcated erythematous macula to plaque formation, with or without erosions. Bowen’s disease is the manifestation of the same carcinoma in situ on keratinizing squamous epithelium and is thus located on the penile shaft, vulvar or perianal. This clinical picture also presents as a sharply demarcated erythematous plaque, often scaling due to horn formation. Invasive transformation is reported in 5-30% (Fig. 2) . In principle, Bowen’s disease can occur on the entire integument, especially on areas exposed to light. Both manifestations are more common in patients over 50 years of age. Balanoposthitis chronica circumscripta plasmacellularis Zoon represents the most important differential diagnosis of erythroplasia queyrat.

Early histologic confirmation and therapy are important to prevent progression to invasive penile carcinoma. In VIN and PIN, the clinical spectrum ranges from macular changes as the most common manifestation to ulcers and warty changes.
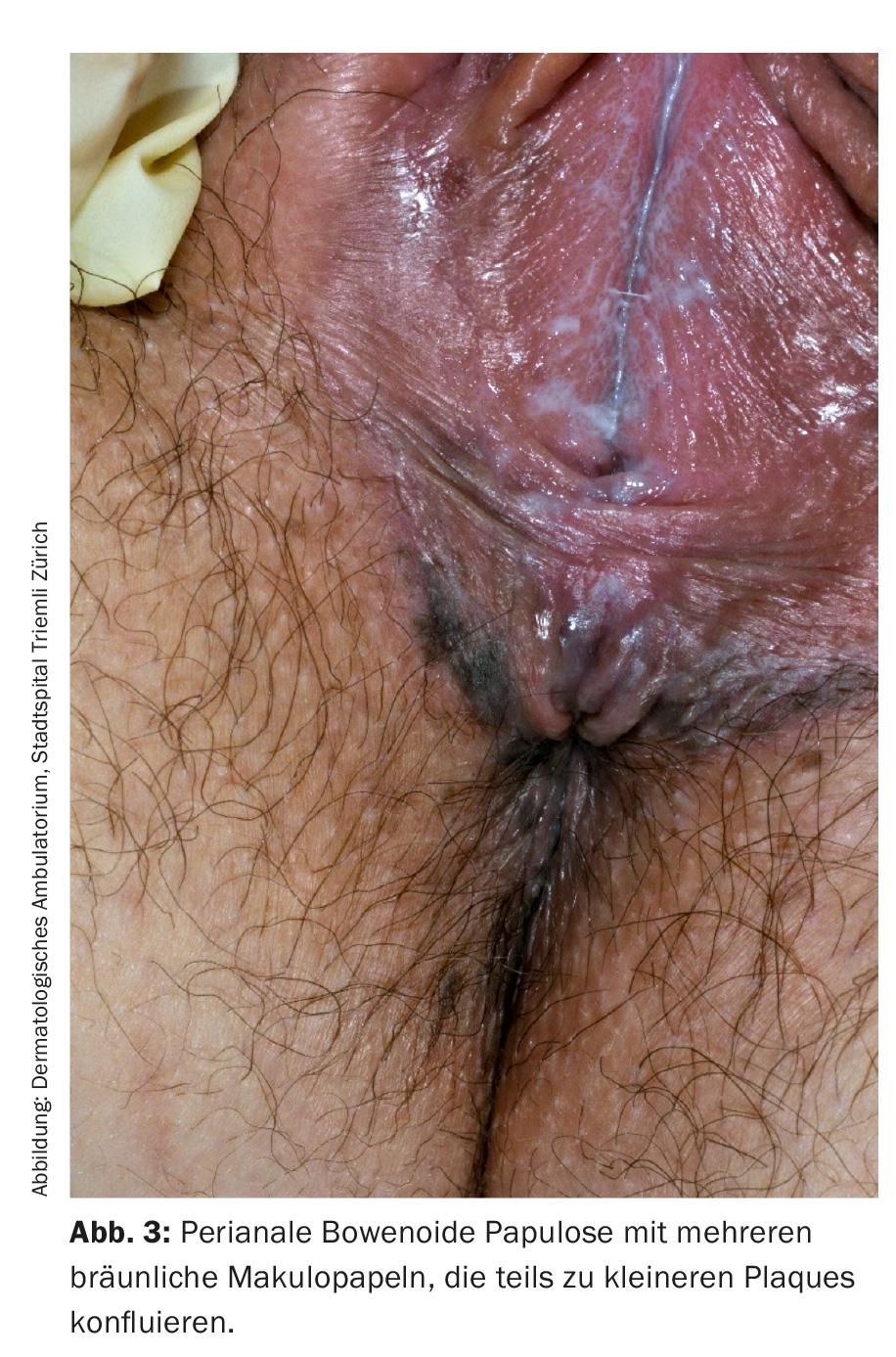
Bowenoid papulosis: It mainly affects sexually active people at a younger age. Bowenoid papulosis primarily presents on the shaft of the penis or labja majora, but may occur throughout the genitals and anally. Multiple small erythematous or brownish papules appear, some of which confluence to form smaller plaques (Fig. 3).
Bowenoid papulosis, like Bowen’s disease or erythroplasia Queyrat, is mainly associated with HPV 16, but biologically shows a completely different activity. While Bowen’s disease and erythroplasia Queyrat are considered carcinoma in situ and show no spontaneous remission, Bowenoid papulosis often shows a benign course with spontaneous remission and less than 1% transformation to invasive carcinoma.
Condylomata gigantea: This is a wart-like exophytic tumor that can occur in all anogenital skin areas in males or females. Condylomata gigantea show transformation to invasive squamous cell carcinoma in 30-56%. Mainly HPV6 and 11 can be detected.
Therapy in general
Therapeutic options after biopsy exclusion of invasive carcinoma include topical application of 5-fluorouracil 5% cream and Imiquimod 5% cream, cryotherapy, photodynamic therapy, LASER ablation, and radiotherapy, depending on the extent of the cancer. Higher-grade intrapepithelial neoplasms are also excised with advantage.
In case of HPV-associated precancerous lesions, screening of other sexually transmitted infections (HIV, syphilis, gonococci, chlamydia) is recommended, as well as partner examination.
Although individual case reports show a longer remission time with quadrivalent HPV vaccination after local therapy, therapeutic vaccination cannot currently be recommended.
Follow up
Due to frequent recurrences, six-monthly follow-up visits for five years are indicated. In the case of conspicuous skin changes, the indication for biopsy should be generous. If free of recurrence, annual check-ups are recommended thereafter for life.
Further reading:
- Çuburu N, et al: Moving forward with human papillomavirus immunotherapies. Hum Vaccin Immunother. 2016; 7: 1-6.
- Hill-Daniel J, et al: Genital Cancers in Women: Vulvar Cancer. 2015; 438: 31-43.
- Köhn FM: Dermatological diseases of the male genital tract. Dermatologist. 2016 Sep 2. [Epub ahead of print].
- Renaud-Vilmer C, et al: Analysis of alterations adjacent to invasive squa-mous cell carcinoma of the penis and their
- relationship with associated carcinoma. J Am Acad Dermatol. 2010; 62: 284-90.
- Edwards SK, et al: 2014 UK national guideline on the management of vulval conditions. Int J STD AIDS 2015; 26: 611-624.
- Arlette JP: Treatment of Bowen’s disease and erythroplasia of Queyrat. Br. J Dermatol 2003; 146: 43-9.
- Borelli S, Lautenschlager S: Differential diagnosis and management of balanitis. Dermatologist 2015; 66: 6-11.
- Teichmann JM, et al: Noninfectious penile lesions. Am Fam Physician. 2010; 81: 167-74.
DERMATOLOGIE PRAXIS 2016; 26(6): 14-16











