In contrast to competitive athletes, there are no generally applicable recommendations for amateur athletes regarding risk stratification for cardiovascular events. An algorithm proposed by the European Society for Cardiac Rehabilitation is based on the pre-existing fitness level as well as the intensity of the targeted exercise activity. A general survey of the cardiovascular risk profile (e.g., using the SCORE tool of the ESC) seems useful. For patients at risk, an exercise ECG is recommended. With patient exercise often unattainable, cardiac imaging would be the next step. Here, cardiac MRI allows radiation-free evaluation of morphology, function, and perfusion. For exclusion or suspicion of coronary anomaly, CCTA is considered the reference method. Furthermore, it allows assessment of coronary morphology with respect to the presence of plaques.
Several studies have demonstrated the positive effect of regular physical training in reducing all-cause mortality, with particular emphasis on reducing cardiovascular risk by modifying “classic” risk factors such as obesity, arterial hypertension, hyperlipidemia, and impaired glucose tolerance [1–5].
The definite benefit of already moderate exercise (20-30 min 3×/week) must be contrasted with the potential risk of cardiovascular events, including the maximum variant of sudden cardiac death, during exercise. The causes vary according to age, with hereditary causes and often unrecognized cases of myocarditis dominating in younger years and being increasingly replaced by coronary artery disease from the age of 30 to 35 (Table 1) [6].
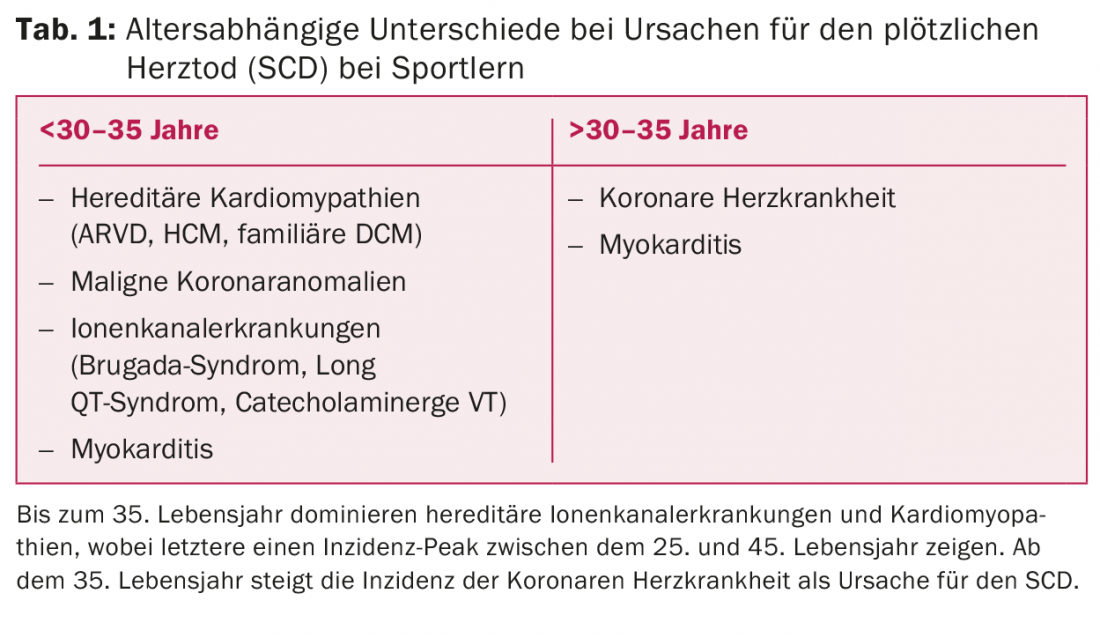
National registry data from Germany [7] and Switzerland [8] even suggest that coronary artery disease or immediate coronary plaque rupture is already much more common in athletes of younger age than previously thought. For young athletes in the field of competitive sports, screening programs [9–13] are already in place in several countries to detect cardiac pathologies (especially congenital coronary anomalies, cardiomyopathies and ion channel diseases) at an early stage. In contrast to this and also in distinction to patients with manifest heart disease [14,15], there are hardly any evidence-based recommendations for action regarding the risk-benefit assessment in amateur athletes with no previous cardiac history. Because acute plaque rupture is the most common cause of sudden cardiac death during exercise in patients 30 to 35 years of age and older, it is particularly important to rule out subclinical CHD in this population before initiating intensified physical training. Especially in high-risk patients (pos. family history, i.e., myocardial infarction or sudden cardiac death in 1st-degree relatives before 50 years of age, diabetes mellitus, and/or significant hypercholesterolemia), early risk stratification is recommended [16].
An algorithm proposed by the European Society for Cardiovascular Prevention and Rehabilitation. [17] for the assessment of the individual training risk before the start of regular sporting activity in people from middle age (defined there as from the age of 35) is based on the existing fitness level and the desired intensity of the hobby sport in order to determine the diagnostic measures indicated in each case. The measure of physical activity used here is the quantification of metabolic equivalents (METs), where 1 MET reflects the metabolic turnover of an average person and can be expressed as 1 kcal/kg/hr.
For people with a low pre-existing activity level (<2 MET-hours/week, which is max. walking), a medical consultation is recommended before starting moderate sports activities (from a MET level of 3, which includes almost all forms of recreational sports such as Nordic walking or cycling). physical examination and a resting ECG as well as a detailed medical history with special attention to the determination of the cardiovascular risk profile (with the help of the SCORE risk calculator of the ESC [18]). In the case of pathological examination results (high-risk constellation according to SCORE, abnormalities in the resting ECG or in the physical examination, or subjectively described cardiac symptoms), further clarification is recommended, as is also usual in everyday clinical practice. In this case, the recommendation provides for a stress ECG as part of a sports medicine evaluation, which should be performed up to the maximum workload (Fig. 1).

In the case of a better baseline fitness level, the possibility of “self-assessment” is cited for individuals with targeted moderate exercise (3-6 METs). For example, standardized questionnaires can be used to determine the presence of cardiac risk factors or corresponding warning symptoms. Only if the test result is abnormal would a medical presentation be indicated for these individuals.
Before starting intensive physical training (>6 METs/h, e.g. regular running training or participation in sports events such as triathlons, etc.), a basic medical check-up is recommended in any case. Again, in the case of abnormal medical examination findings, a stress ECG should be obtained up to the point of exercise (Fig. 2).

However, a problem that has been proven by many studies [19,20] and is well known from clinical practice arises from the often clearly limited informative value of the stress ECG. Especially in asymptomatic patients, the rate of false-positive and false-negative test results is comparatively high, and especially in women, the test must be considered significantly less sensitive and specific.
The exercise ECG implemented in screening programs developed for competitive athletes may therefore be suitable for individuals with a certain pre-existing “basic fitness” to reliably clarify unclear, potentially cardiac symptoms or ECG changes in case of doubt. However, the demographic composition of the population of willing amateur athletes encountered in clinical practice may correspond more closely to that of the patient population represented, for example, in the current ESC guidelines for the evaluation of possible CHD [21]. Here, in view of the often reduced informative value of the diagnostic modality, reference is made to the existing alternatives in terms of cardiac imaging with pharmacological exposure if necessary. In everyday life, patients with a non-feasible or inconclusive stress ECG, or in the case of a conspicuous finding, can be referred for further, non-invasive diagnostics in order to ensure their suitability for sports activities.
Transthoracic echocardiography (TTE)
As a cost-effective and readily available imaging modality, transthoracic echocardiography has a high value in basic cardiology diagnostics, as it allows rapid assessment of global pump function, kinetic disturbances, cardiac dimensions, and valve status. In younger patients, early detection of hypertrophic cardiomyopathy (HCM) in particular is a domain of TTE, although the problematic differentiation between “physiological” hypertrophy, i.e. induced by regular exercise per se, and pathological thickening of the myocardium should be pointed out here [22]. Differentiation from “athlete’s heart” can also be difficult when diagnosing other cardiomyopathies (ARVC, non-compaction CMP) [23,24], so that connected alternative imaging (especially CMR) may be required [6]. Another area of application for TTE is the suspected diagnosis of myocarditis, especially in younger patients, although the changes that may occur in this clinical picture, such as a pericardial effusion, regional kinetic disturbances or reduced pump function, should be regarded as non-specific. In addition, especially in very well-trained patients, the latter findings may also exist as a normal variant and, in case of doubt, may be difficult to differentiate from dilated cardiomyopathy without further imaging [25]. Newer echocardiographic techniques such as strain analysis or 3D echo may be useful in the diagnosis of myocarditis, but their clinical value currently remains questionable in this setting and has been evaluated primarily only in the context of case reports [26,27].
For the evaluation of the valvular apparatus, TTE remains an indispensable tool and allows rapid detection of vitiation in any age group. In the case of relevant CAD, the presence of wall motion abnormalities and their localization may indicate an existing perfusion problem or more recent coronary events. Furthermore, rapid quantification of pump function is an essential element of routine cardiac diagnostics and allows initial risk stratification with respect to the likelihood of sudden cardiac death [28].
Coronary CT angiography (CCTA)
Thanks to the technical development of CCTA in the last decade, it is now possible to perform high-resolution coronary CT with very low radiation dose (usually below 5mSv, in most cases below 2mSv) and high sensitivity as well as excellent negative predictive value with respect to the detection and exclusion of stenosing CAD by means of the latest generation of (at least) 64-line scanners. [29,30,31]. In the case of a pure determination of the coronary calcium load, the radiation exposure can be further reduced and the administration of contrast medium can even be dispensed with, so that, for example, according to current NICE guidelines [32] in patients with a low pretest probability of CHD (10-29%), initial calcium scoring and subsequent CCTA is even recommended as first-line diagnostics (instead of an exercise ECG) for the clarification of chest pain. However, the limiting factor here is the definition of an “increased” calcium load, which will only be undercut by absolute low-risk patients.
Despite the proven high benefit of CCTA as an “exclusion test” with regard to relevant CHD, according to current guidelines of the relevant professional societies, there is only one recommendation for patients with intermediate cardiovascular risk [21]but not for an asymptomatic low-risk population, as frequently encountered in the context of sports medicine screening examinations, since here the risk-benefit ratio is not considered to be sufficiently balanced, taking into account the (albeit low) radiation dose and contrast agent exposure.
Furthermore, with regard to the risk of potentially lethal plaque rupture, the diagnostic dilemma of identifying and presenting the “vulnerable plaque” arises, since it is well known that even mild to moderate coronary stenoses can be the cause of sudden cardiac death in the event of acute plaque rupture. Although CCTA is limited by its spatial resolution compared with invasive examination methods such as intravascular ultrasound or optical coherence tomography with regard to more precise characterization of the structure of any plaques that may be present, it can nevertheless provide valuable information with regard to the differentiation of very lipid-rich to more fibrous-calcified lesions and thus contribute to risk stratification [33,34].
Apart from the visualization of atherosclerotic plaques and stenoses, CCTA also offers the possibility of diagnosing coronary anomalies, which should be considered as a possible cause of sudden cardiac death during exercise, especially in very young athletes. CCTA is considered the reference standard for the diagnosis of coronary anomalies due to its ability to simultaneously image not only the affected vessel but also the surrounding anatomical structures (Fig. 3).

Cardiac magnetic resonance imaging (CMR)
MR examinations of the heart offer the possibility of an integrative diagnosis of cardiac morphology and function, whereby a variety of pathologies can be detected with high diagnostic accuracy. For the determination of cardiac dimensions, volumes, and right or left ventricular function, CMR imaging is already the gold standard and, compared with echocardiography, is convincing with its high degree of reproducibility and low inter-observer variability [35]. Especially for younger patients, this low-stress, radiation-free diagnostic modality is now an indispensable tool for the evaluation of hereditary cardiomyopathies (such as arrhythmogenic right ventricular dysplasia (ARVD) or HCM (Fig. 4) as a possible cause of sudden cardiac death. The administration of contrast agent allows the acquisition of late gadolinium enhancement (LGE) images, which allows a differentiated characterization of various myocardial structural abnormalities as they can be observed in cardiomyopathies, but also inflammatory and not least, ischemic disease patterns.

Regarding the latter point, performing a CMR perfusion study using adenosine or dobutamine as a pharmacological stressor allows reliable, noninvasive detection of relevant myocardial ischemia with high sensitivity and specificity [36–39].
In addition, CMR also allows the diagnosis of coronary [40] or other vascular abnormalities for the purpose of completing the morphologic findings.
Thus, cardiac MR imaging, like no other non-invasive diagnostic tool, allows a comprehensive assessment of possible cardiac pathologies, which may represent a relevant risk in the context of sporting activity both in younger athletes without a cardiac risk profile (cardiomyopathies, coronary anomalies) and in amateur athletes from middle age onwards with corresponding lifestyle factors and increasing risk of relevant CHD if not detected.
Summary
In contrast to existing recommendations for sports medicine evaluation of competitive athletes, there are hardly any uniform guidelines for basic cardiac diagnostics in amateur athletes, taking into account the limited data available. For clinical practice, it is recommended to orient the patient’s existing fitness level, the intensity of the intended sporting activity and a survey of the cardiac risk profile, which can also be carried out in “self-assessment” if necessary. A clarification with resting and possibly even stress ECG should be reserved for patients at risk or persons with intended intensive physical stress. Because of the frequently reduced validity of the stress ECG, a noninvasive imaging modality should be chosen as the initial measure in questionable cases. Because plaque ruptures are the most common cause of sports-associated SCD in >30- to 35-year-olds, CCTA is recommended to assess coronary morphology, especially in high-risk patients with a distinct cardiovascular risk profile. Alternatively, CMR as a whole appears to be the method of choice for comprehensive cardiac diagnosis beyond the spectrum of CHD due to its lack of radiation exposure as well as its comprehensive diagnostic capabilities for a variety of issues in a wide range of age groups.
Literature:
- Paffenbarger Jr RS, et al: The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. The New England Journal of Medicine 1993; 328: 538-545.
- Blair SN, et al: Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA 1996; 276: 205-210.
- Talbot LA, et al: Changes in leisure time physical activity and risk of all-cause mortality in men and women: the baltimore longitudinal study of aging. Prev Med 2007; 45: 169-176.
- Sofi F, et al: Physical activity during leisure time and primary prevention of coronary heart disease: An updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil 2008; 15: 247-257.
- Nocon M, et al: Association of physical activity with all-cause and cardiovascular mortality: A systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 2008; 15: 239-246.
- La Gerche A, et al: Cardiac imaging and stress testing asymptomatic athletes to identify those at risk of sudden cardiac death. JACC Cardiovasc Imaging 2013; 6: 993-1007.
- Bohm P, Scharhag J, Meyer T: Data from a nationwide registry on sports-related sudden cardiac deaths in Germany. Eur J Prev Cardiol 2016; 23: 649-656.
- Grani C, et al: Sports-related sudden cardiac death in Switzerland classified by static and dynamic components of exercise. Eur J Prev Cardiol 2016; 23: 1228-1236.
- Maron BJ, et al: Cardiovascular preparticipation screening of competitive athletes. A statement for health professionals from the sudden death committee (clinical cardiology) and congenital cardiac defects committee (cardiovascular disease in the young), American Heart Association. Circulation 1996; 94: 850-856.
- Maron BJ, et al: Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: A scientific statement from the American Heart Association council on nutrition, physical activity, and metabolism: Endorsed by the American College of Cardiology foundation. Circulation 2007; 115: 1643-1655.
- Pelliccia A, et al.: Bethesda conference no. 36 and the European Society of Cardiology consensus recommendations revisited. A comparison of U.S. and European criteria for eligibility and disqualification of competitive athletes with cardiovascular abnormalities. Journal of the American College of Cardiology 2008; 52: 1990-1996.
- Corrado D, et al.: Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: Proposal for a common European protocol. Consensus statement of the study group of sport cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the European Society of Cardiology. European Heart Journal 2005; 26: 516-524.
- Corrado D, et al: Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 2006; 296: 1593-1601.
- Börjesson M, et al: Esc study group of sports cardiology: Recommendations for participation in leisure-time physical activity and competitive sports for patients with ischaemic heart disease. Eur J Cardiovasc Prev Rehabil 2006; 13: 137-149.
- Heidbüchel H, et al: Recommendations for participation in leisure-time physical activity and competitive sports of patients with arrhythmias and potentially arrhythmogenic conditions. Part ii: Ventricular arrhythmias, channelopathies and implantable defibrillators. Eur J Cardiovasc Prev Rehabil 2006; 13: 676-686.
- Chugh SS, et al: Sudden cardiac death in the older athlete. Journal of the American College of Cardiology 2015; 65: 493-502.
- Börjesson M, et al: Cardiovascular evaluation of middle-aged/senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular prevention and rehabilitation. Eur J Cardiovasc Prev Rehabil 2011; 18: 446-458.
- Piepoli MF, et al: 2016 European guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). European Heart Journal 2016; 37: 2315-2381.
- Gianrossi R, et al: Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation 1989; 80: 87-98.
- Josephson RA, et al: Can serial exercise testing improve the prediction of coronary events in asymptomatic individuals? Circulation 1990; 81: 20-24.
- Montalescot G, et al: 2013 esc guidelines on the management of stable coronary artery disease: The task force on the management of stable coronary artery disease of the European society of cardiology. European Heart Journal 2013; 34: 2949-3003.
- Lauschke J, Maisch B: Athlete’s heart or hypertrophic cardiomyopathy? Clin Res Cardiol 2009; 98: 80-88.
- La Gerche A, et al: Exercise-induced right ventricular dysfunction and structural remodeling in endurance athletes. European Heart Journal 2012; 33: 998-1006.
- Caselli S, et al: Prominent left ventricular trabeculations in competitive athletes: A proposal for risk stratification and management. International Journal of Cardiology 2016; 223: 590-595.
- Abergel E, et al: Serial left ventricular adaptations in world-class professional cyclists: implications for disease screening and follow-up. Journal of the American College of Cardiology. 2004; 44: 144-149.
- Jeserich M, et al: Non-invasive imaging in the diagnosis of acute viral myocarditis. Clin Res Cardiol 2009; 98: 753-763.
- Afonso L, et al: Acute myocarditis: Can novel echocardiographic techniques assist with diagnosis? Eur J Echocardiogr 2010; 11: E5.
- Konety SH, et al: Echocardiographic predictors of sudden cardiac death: the atherosclerosis risk in communities study and cardiovascular health study. Circ Cardiovasc Imaging 2016; 9(8). doi: 10.1161/CIRCIMAGING.115.004431.
- Min JK, et al: Noninvasive diagnostic and prognostic assessment of individuals with suspected coronary artery disease: coronary computed tomographic angiography perspective. Circ Cardiovasc Imaging 2008; 1: 270-281; discussion 281.
- Hamon M, et al: Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: A meta-analysis. Journal of the American College of Cardiology 2006; 48: 1896-1910.
- Gordic S, et al: High-pitch coronary ct angiography with third generation dual-source ct: limits of heart rate. Int J Cardiovasc Imaging 2014; 30: 1173-1179.
- Chest pain of recent onset: Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. London; 2010.
- Saremi F, et al: Coronary plaque characterization using ct. AJR Am J Roentgenol 2015; 204: W249-260.
- Arbab-Zadeh A, et al: The myth of the “vulnerable plaque”: Transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. Journal of the American College of Cardiology 2015; 65: 846-855.
- Hundley WG, et al: Accf/acr/aha/nasci/scmr 2010 expert consensus document on cardiovascular magnetic resonance: A report of the American College of Cardiology foundation task force on expert consensus documents. Circulation 2010; 121: 2462-2508.
- Gotschy A, et al: Cardiovascular magnetic resonance for the assessment of coronary artery disease. International Journal of Cardiology 2015; 193: 84-92.
- Manka R, et al: Head-to-head comparison of first-pass mr perfusion imaging during adenosine and high-dose dobutamine/atropine stress. Int J Cardiovasc Imaging 2011; 27: 995-1002.
- Jahnke C, et al: Prognostic value of cardiac magnetic resonance stress tests: adenosine stress perfusion and dobutamine stress wall motion imaging. Circulation 2007; 115: 1769-1776.
- Paetsch I, et al: Comparison of dobutamine stress magnetic resonance, adenosine stress magnetic resonance, and adenosine stress magnetic resonance perfusion. Circulation 2004; 110: 835-842.
- Prakken NH, et al: Screening for proximal coronary artery anomalies with 3-dimensional mr coronary angiography. Int J Cardiovasc Imaging 2010; 26: 701-710.
Further reading:
- Börjesson M, et al: Cardiovascular evaluation of middle-aged/senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European association of cardiovascular prevention and rehabilitation. Eur J Cardiovasc Prev Rehabil 2011; 18: 446-458.
- Nocon M, et al: Association of physical activity with all-cause and cardiovascular mortality: A systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil 2008; 15: 239-246.
- Piepoli MF, et al: 2016 European guidelines on cardiovascular disease prevention in clinical practice: The sixth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). European Heart Journal 2016; 37: 2315-2381.
- Montalescot G, et al: 2013 esc guidelines on the management of stable coronary artery disease: The task force on the management of stable coronary artery disease of the European Society of Cardiology. European Heart Journal 2013; 34: 2949-3003.
- Gotschy A, et al: Cardiovascular magnetic resonance for the assessment of coronary artery disease. International Journal of Cardiology 2015; 193: 84-92.
- Min JK, Shaw LJ: Noninvasive diagnostic and prognostic assessment of individuals with suspected coronary artery disease: coronary computed tomographic angiography perspective. Circ Cardiovasc Imaging 2008; 1: 270-281; discussion 281.
- Corrado D, et al.: Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: Proposal for a common European protocol. Consensus statement of the study group of sport cardiology of the working group of cardiac rehabilitation and exercise physiology and the working group of myocardial and pericardial diseases of the European Society of Cardiology. European Heart Journal 2005; 26: 516-524.
- Börjesson M, et al: Esc study group of sports cardiology: Recommendations for participation in leisure-time physical activity and competitive sports for patients with ischaemic heart disease. Eur J Cardiovasc Prev Rehabil 2006; 13: 137-149.
- Chugh SS, et al: Sudden cardiac death in the older athlete. Journal of the American College of Cardiology 2015; 65: 493-502.
- Grani C, et al: Sports-related sudden cardiac death in Switzerland classified by static and dynamic components of exercise. Eur J Prev Cardiol 2016; 23: 1228-1236.
CARDIOVASC 2016; 15(6): 25-32











