The medical steps involved in physical gender reassignment (transition) have become well established in Switzerland in recent years. As a prerequisite for a medical measure, a so-called letter of indication is required from the endocrinological and surgical side. In this report, the supervising specialist (psychiatrist or psychotherapist with experience in transgender medicine) writes a detailed assessment according to the age and life situation of the person concerned, describing the diagnosis, mental condition, capacity for judgment as well as the expected course.
The medical steps involved in physical gender reassignment (transition) have become well established in Switzerland in recent years. As a prerequisite for a medical measure, a so-called letter of indication is required from the endocrinological and surgical side. In this report, the attending professional (psychiatrist or psychotherapist with experience in transgender medicine) writes a detailed assessment according to the age and life situation of the person concerned, describing the diagnosis, mental condition, ability to judge and the expected course.
Earlier concepts with everyday tests, waiting periods and prescribed number of psychotherapy hours are now considered outdated in Switzerland and are no longer a prerequisite, neither for hormonal nor for surgical gender reassignment. Rather, attention is given to the personal needs of the individual transperson and the focus is on the patient’s individual treatment plan. To date, there are no medical guidelines in Switzerland and also the jurisdiction, in contrast to Germany, does not have a so-called “transsexual law”. For this reason, Swiss counseling and treatment recommendations by trans-experienced professionals were published for the first time in 2014 [1]. Like all recommendations, these are not binding, but are generally accepted throughout Switzerland. Based on these recommendations as well as the WPATH Standards of Care Vs. 7 (SOC 7) of the World Professional Association for Transgender Health (WPATH) [2] and the Guidelines of the American Endocrine Society [3], any physician in Switzerland is allowed to prescribe sex hormones for gender reassignment.
The costs of body-modifying treatments such as hormone therapy, plastic surgery as well as epilation and voice training are covered by the health insurance companies in accordance with the KVG in the basic insurance. Due to the significant increase in the number of people undergoing medical gender reassignment in recent years, trans people will be seen more often as patients in practices in the future. This inevitably leads to new aspects and questions with which the family doctor is confronted.
In what follows, I will now discuss the various aspects of transgender medicine in everyday practice.
Family practice as primary point of contact
As a trusted person, the family doctor or a trusted specialist (gynecologist) is often the first person sought out by those seeking advice. For the patient, this revelation of the innermost feelings is an emotionally difficult situation and it takes a great deal of effort for someone to report their discomfort with their own birth sex. Therefore, it is important to adopt an appreciative and open-ended attitude. There is no need for immediate solutions, it is sufficient if the transperson feels picked up and understood in his, perhaps still disordered or unclear thoughts.
Not every person who feels uncomfortable in their gender is considered transgender and requires physical gender reassignment. It does mean, however, that this person may need psychotherapeutic support in self-discovery and self-definition. As a next step, referral to an appropriate therapist may be appropriate. Corresponding addresses in the immediate vicinity can be requested via trans-specific online portals [4].
Co-supervision during gender reassignment hormone therapy (GHT).
Unfortunately, the resources of endocrinology professionals who are knowledgeable in gender reassignment are limited in Switzerland. As a result, many patients have to travel long distances to find a suitable specialist with free capacity. While we are eager to further expand capacity at larger hospitals, time constraints often dictate that care be provided locally through family practice. A common model has proven to be that after detailed assessment and clinical examination, the endocrinologist:initiates GHT and further care can then be provided in the primary care physician’s office. This applies in particular to the dispensing and administration of hormone preparations and regular laboratory checks. In close cooperation with the hormone specialists, these patients can usually be cared for without any problems.
It is important to note when caring for trans people in family practice that exceedingly the most common complaints of trans patients have nothing to do with transition and GHT or gender reassignment surgery will rarely play a role in this setting.
Consequences of long-term GHT
The discovery and synthesization of sex hormones made it possible to perform sex reassignment hormone treatments in the late 1940s. The first systematic studies of medical gender reassignment date back to the early 1990s. This means that we now have at least 80 years of clinical experience and 30 years of scientific experience in this field. The evidence to date suggests that the therapy is safe and sound.
Unfortunately, the study results are of limited value. The studies conducted include small numbers of subjects and the data have mostly been collected retrospectively. A further complicating factor is that hardly any research funds are available and universities, probably for reasons of prestige, rarely want to deal with this field of research. All hormone preparations are used in so-called “off label use”, as there are no products on the market that are specifically approved for the treatment of trans people.
On the other hand, sex hormone therapy is a well-researched and inexpensive preparation that has been used successfully and with low risk in other medical contexts for many years. Consider, for example, sex hormone preparations in the treatment of postmenopausal symptoms in women [5].
Consequences of long-term estrogen therapy in transwomen.
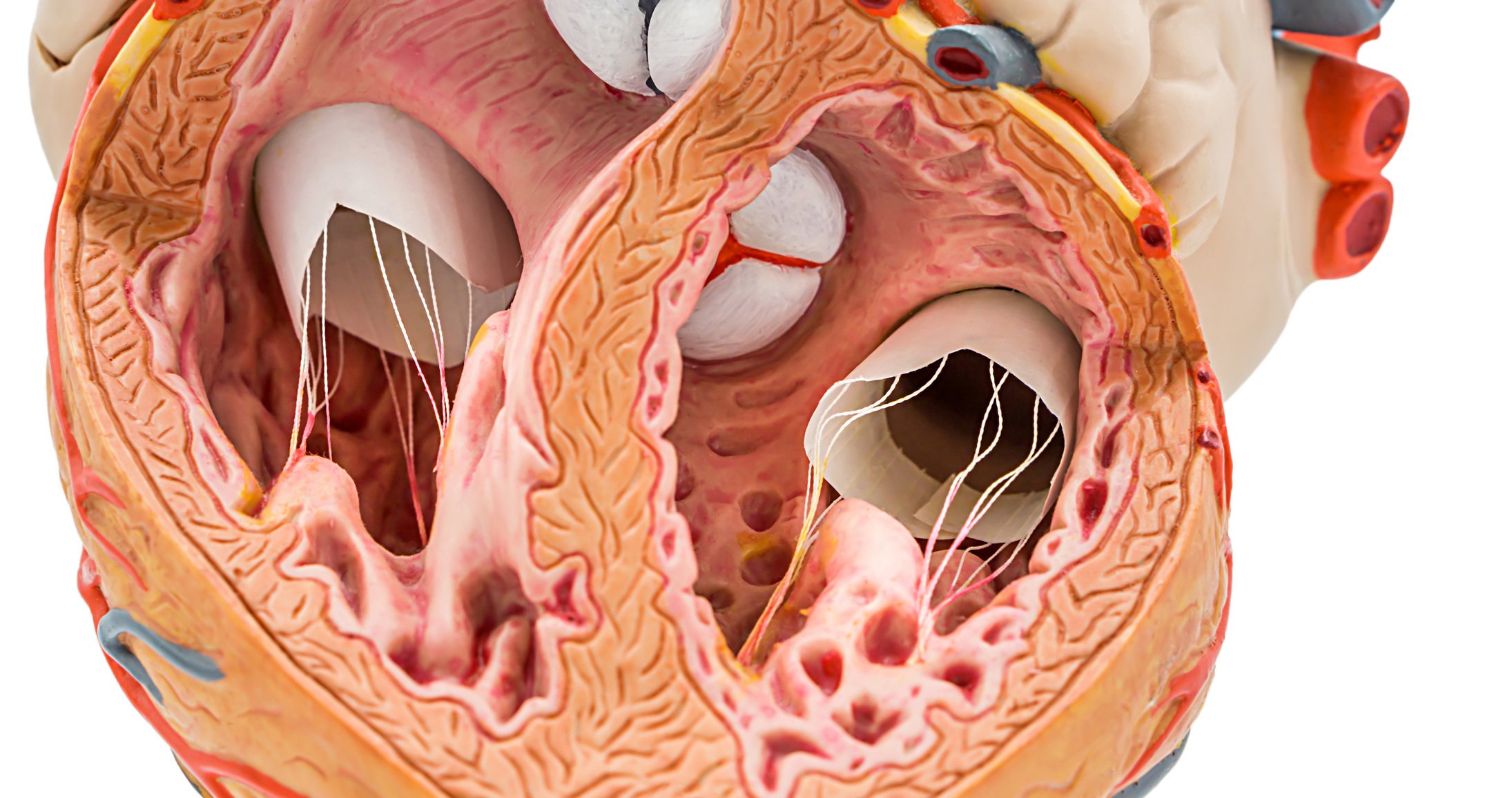
Large studies in ciswomen have shown that estradiol substitution in postmenopause has a beneficial effect on lipid profile, glucose metabolism, and endothelial function [6]. A protective cardiovascular effect of female hormones has also been demonstrated [7]. No such effect was found in studies with transwomen [8]. However, it must be emphasized that the quality and significance of these studies are rather weak. This may be because, as noted above, the majority of these studies have been retrospective and do not provide insight into how sex hormones alter vascular physiology in trans women. In addition, dosages and type of hormone therapy are heterogeneous and no clear statements on target hormone levels are found. Similarly, it is difficult to determine the extent to which nicotine abuse, drug use, minority stress, and other lifestyle effects contributed additionally to cardiovascular risk in the transgender population. Also, no consensus could be reached on whether transgender individuals in studies should be compared with populations from their birth sex or their assumed sex.
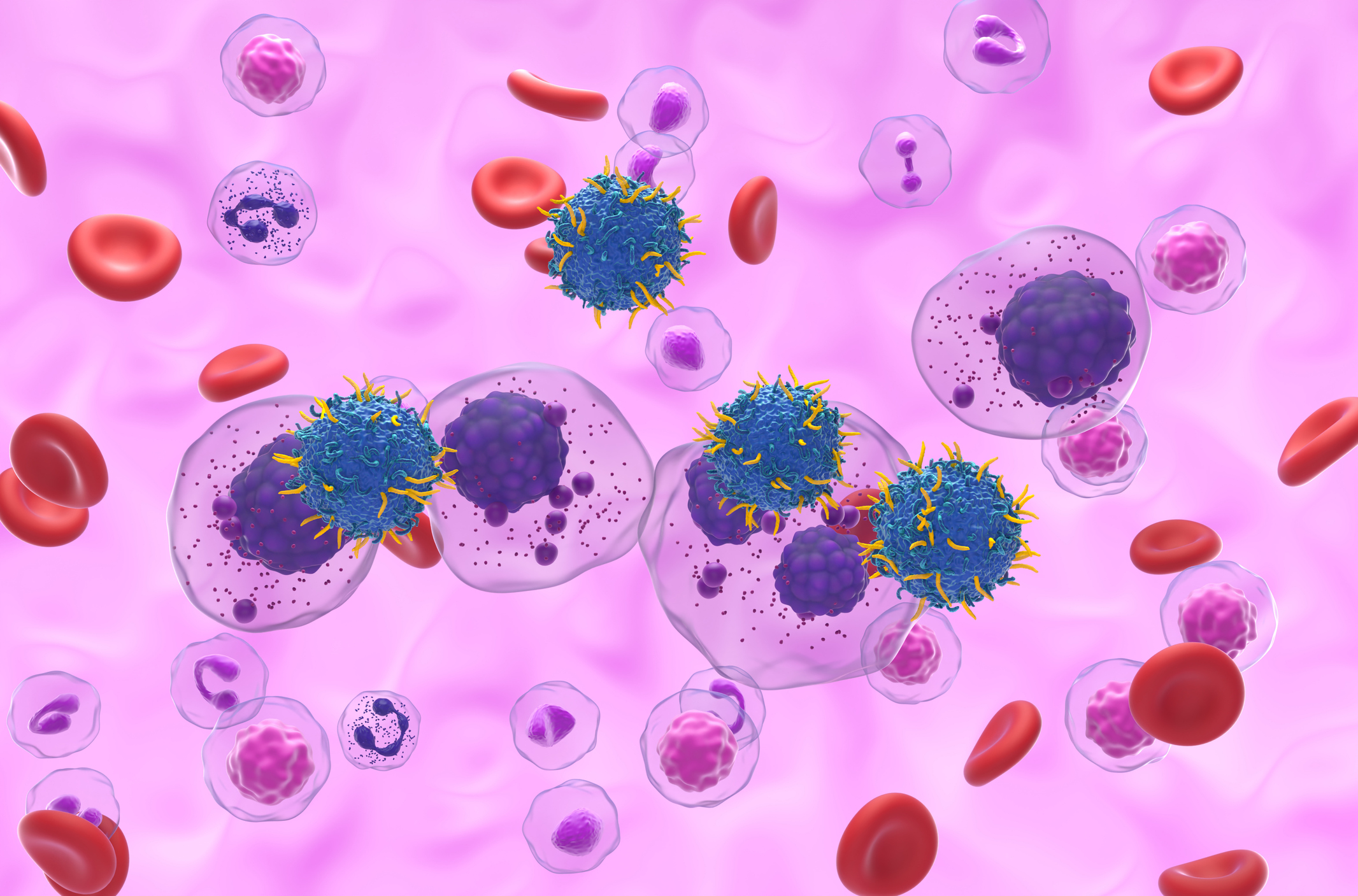
Current evidence suggests that the use of estrogen in hormonal treatment of transwomen carries an increased risk of myocardial infarction and ischemic stroke. Whether this is a consequence of GHT or a consequence of original birth sex remains unclear, as not all studies show an increased risk compared to cismen [9].
On the other hand, studies have shown that the risk of thromboembolic events due to feminizing hormone therapy has decreased significantly over the last 20 years. The reason for this is probably the avoidance of ethinylestradiol-containing preparations, which carry a greatly increased risk of thromboembolism [10]. The favored transdermal or parenteral application of sex hormones also reduces this risk [11–13].
According to these findings, value should be placed on parenteral application of sex hormones wherever possible: Hormone patches, gel or depot injections. This relieves the enterohepatic circulation and minimizes thrombogenic influences. The use of ethinylestradiol (often a component of hormonal anticonception) in the context of gender reassignment is obsolete because the thromboembolic risk is far too high.
Consequences of long-term testosterone therapy in trans men.
The data for trans men undergoing gender reassignment hormone therapy present a contradictory picture. There is evidence that under testosterone therapy, blood pressure levels often increase, serum lipid profile worsens. Total cholesterol increases, triglycerides also increase, and the HDL/LDL ratio is less favorable [9,14,15]. In the absence of prospective studies with cardiovascular complications as end points, nothing can be said about the influence of these risk factors. A 2011 Dutch study found no negative impact in terms of morbidity and mortality from testosterone replacement in trans men compared to the average population over several decades [10]. A similar picture emerged from a 2018 Spanish review study [16]. However, a recent study from the USA, based on regular population health surveys, was able to show with a large number of cases that the risk of myocardial infarction appears to increase by up to 4-fold in trans men compared to the cis male population [17]. This study is based on the “Behavioral Risk Factor Surveillance System” in the form of regular telephone interviews in the American population with which the health status and risk behavior is recorded. In my opinion, this form of data collection significantly relativizes the significance of the study.
Here, further and preferably prospective studies with clinically collected data on cardiovascular risks and diseases in trans people would be urgently needed to enable better medical care and to create evidence-based guidelines.
A serious side effect of testosterone therapy is polyglobulia or erythrocytosis. This adverse effect may affect up to 11% of trans men during the course of treatment [18]. Nevertheless, in this study, there were no thromboembolic events in transmen with high hematocrit levels of >54%. It is interesting to note that the greatest increase in hematocrit in all treated transmen occurred in the first 12 months of treatment, but the risk of polyglobulia, although rare, may persist after 20 years.
It was also shown that nicotine use and obesity increased the likelihood of higher hematocrit levels. From my personal experience, arterial hypertension and high testosterone plasma levels also seem to promote polyglobulia.
The incidence of this side effect in the study was similar to that seen in cismale patients treated for hypogonadism with exogenous testosterone. However, further literature searches on the subject of polyglobulia and arterial circulatory disorders revealed no evidence of acute life-threatening complications even with hematocrit levels of 55% and hemoglobin levels as high as 200 g/l. Exceptions are found in cases of abusive overdose with anabolic steroids, for example in the context of bodybuilding or doping [19–21].
It is recommended to perform regular hematocrit determinations under GHT with testosterone (cf. see the guidelines of the Endocrine Society [3]). In case of a strong increase, the hormone dosage should be reduced (extend interval or reduce injection dose) or switch to another preparation with a shorter half-life. Nicotine stop, weight regulation and correct blood pressure setting goes without saying. Occasionally, bloodletting may be useful. If there is additional risk, prophylactic treatment with ASA or blood thinning should be considered.
And what do we know about the liver?
In the package insert of all preparations containing sexual hormones, we find references to liver damage: pathological changes in liver function values, jaundice, cholelithiasis, liver tumors, etc. Thus, guidelines also often refer to these serious risks of liver damage, which can be potentially fatal.
An Amsterdam study from 2021 investigated exactly this question and showed the following: 1933 trans persons (889 trans women and 1044 trans men) were prospectively observed for more than 10 years and regularly monitored by laboratory chemistry. The risk of liver damage, defined as a 2-3-fold increase in liver enzymes in the blood, was 0.1% in transwomen and a maximum of 0.6% in transmen. Symptomatic liver disease did not occur [22]. This is also in line with my personal experience in working with trans patients for over 10 years. The incidence for severe liver injury with properly performed GHT is very low.
Osteoporosis
In the clinical setting, there are often concerns about the safety of gender reassignment hormone therapy (GHT) for bone health. This is probably related to the fact that previous studies have found lower bone density in transwomen under long-term GHT compared to cismen. At the same time, there was concern that testosterone therapy in trans men would lower serum estradiol levels, which could have negative effects on bone density.
However, the results of a 2018 study suggest that sex reassignment therapy with sex hormones does not show negative effects on bone density. However, it has been shown that a high percentage of low bone density could be measured in transwomen even before the start of physical transition, i.e. before the administration of estrogen preparations and testosterone blockers [23]. Causes for this are unclear. In my practice, however, I find many transwomen with vitamin D levels that are clearly too low, which can probably be explained by social phobia and intensive activity at the computer. This circumstance, combined with a poor diet and lack of exercise, may be at least partially responsible for low bone mass.
According to the conclusions of this study, it makes sense to perform bone densitometry only if there are risk factors for osteoporosis, especially if the patients have stopped their GHT for a long time after gonadectomy. Monitoring of bone density under correctly administered hormone therapy is not necessary. However, the effect of GHT on fracture risk is not known and should be the subject of further research.
Summary
Gender reassignment hormone therapy (GHT) under medical supervision is considered low risk and is comparable to other hormone therapy used in medicine (hormone replacement in postmenopause, hormonal anticonception, sex hormones in male hypogonadism). In recent years, there has been a significant increase in the number of patient:s seeking hormonal and physical sex reassignment surgery. Thus, the possibility of encountering trans people in general practice is also increasing. In the most common situations, these are general health problems unrelated to medical transition. Nevertheless, when problems related to physical alignment do occur, they are primarily cardiovascular events. However, the extent to which these occur more frequently than in the average population is not clear from the studies to date. It certainly makes sense to monitor trans people under GHT regularly, at least every one to two years, focusing here on the classic risk factors for cardiovascular disease.
Take-Home Messages
- A GHT in the context of physical transition is safe and easy to perform.
- Long-term consequences are rarely expected and primarily affect the cardiovascular system.
- The pathologization of non-congruent gender identities is obsolete and will also be formally abolished when ICD-11 comes into effect in 2022.
- Before starting hormone treatment, there should be an indication by psychiatry and/or psychotherapy – according to the treatment recommendations.
- The primary care physician or family practitioner plays an increasingly important role in the care of trans people. An affirmative and open-ended climate of discussion can be very helpful.
Literature:
- Nuñez DG, Gross P, Baeriswyl M, et al. (Ed.): From Transsexuality to Gender Dysphoria – Counseling and Treatment Recommendations for TransPersons; available at www.guidelines.fmh.ch.
- Coleman E, et al: Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. International Journal of Transgender Health 2022; 23 (sup1): 1-259.
- Hembree WC, Cohen-Kettenis PT, Gooren L, et al: Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2017; 102(11): 3869-3903; doi: 10.1210/jc.2017-01658. erratum in: J Clin Endocrinol Metab 2018; 103(2): 699. erratum in: J Clin Endocrinol Metab 2018; 103(7): 2758-2759.
- E.g., www.tgns.ch; www.fachgruppetrans.ch.
- Manson JE, Aragaki AK, Rossouw JE, et al: Menopausal hormone therapy and long-term all-cause and cause-specific mortality: the Women’s Health Initiative Randomized Trials. JAMA 2017; 318(10): 927-938; doi:10.1001/jama.2017.11217.
- Mendelsohn ME, Karas RH: The protective effects of estrogen on the cardiovascular system. N Engl J Med 1999; 340(23): 1801-1811.
- Boardman HMP, et al: Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database of Systematic Reviews 2015, Art. No.: CD00229; doi: 10.1002/14651858.CD002229.pub4.
- Streed Cg Jr, et al: Cardiovascular disease Among transgender adults receiving hormone therapy: A narrative review. Ann Intern Med 2017; 167(4): 256-267; doi: 10.7326/M17-0577.
- Nota Nienke M, Wiepjes CM, de Blok C, et al: Ocurrence of Acute Cardiovascular Events in Transgender Individuals Receiving Hormone Therapy. Circulation 2019; 139(11): 1461-1462; doi: 10.1016/j.endinu.2018.11.004.
- Asscheman H, Giltay E, Megens J, et al: A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol 2011; 164: 635-642.
- Toorians AW, et al: Venous thrombosis and changes of hemostatic variables during cross-sex hormone treatment in transsexual people. J Clin Endocrinol Metab 2003; 88(12): 5723-5729.
- Ott J, et al: incidence of thrombophilia and venous thrombosis in transsexuals under cross-sex hormone therapy. Fertil Steril 2010; 93(4): 1267-1272; doi: 10.1016/j.fertnstert.2008.12.017.
- Asscheman H, et al: Venous thrombo-embolism as a complication of cross-sex hormone treatment of male-to-female transsexual subjects: a review. Andrologia 2014; 46(7): 791-795; doi: 10.1111/and.12150.
- Quirós C, et al.: Effect of cross-sex hormone treatment on cardiovascular risk factors in transsexual individuals. Experience in a specialized unit in Catalonia. Endocrinol nutr 2015; 62(5): 210-216; doi: 10.1016/j.endonu.2015.02.001.
- Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, et al: Sex Steroids and Cardiovascular Outcomes in Transgender Individuals: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab 2017; 102(11): 3914-3923; doi: 10.1210/jc.2017-01643.
- Elamin MB, et al: Effect of sex steroid use on cardiovascular risk in transsexual individuals: a systematic review and meta-analyses. Clin Endocrinol (oxf) 2010; 72(1): 1-10; doi: 10.1111/j.1365-2265.2009.03632.x.
- Alzahrani T, Nguyen T, Ryan A, et al: Cardiovascular Disease Risk Factors and Myocardial Infarction in the Transgender Population. Circ Cardiovasc Qual Outcomes 2019; 12(4): e005597; doi: 10.1161/CIRCOUTCOMES.119.005597.
- Madsen MC, van Dijk D, Wiepjes CM, et al: Erythrocytosis in a Large Cohort of Trans Men Using Testosterone: A Long-Term Follow-Up Study on Prevalence, Determinants, and Exposure Years. J Clin Endocrinol Metab 2021; 106(6): 1710-1717; doi: 10.1210/clinem/dgab089.
- Ederveen EGT, van Hunsel FPAM, Wondergem MJ, van Puijenbroek EP.: Severe Secondary Polycythemia in a Female-to-Male Transgender Patient While Using Lifelong Hormonal Therapy: A Patient’s Perspective. Drug Saf Case Rep 2018; 5(1): 6; doi: 10.1007/s40800-018-0075-2.
- Osterberg EC, Bernie AM, Ramasamy R: Risks of testosterone replacement therapy in men. Indian J Urol 2014; 30(1): 2-7; doi: 10.4103/0970-1591.124197.
- Calof OM, Singh AB, Lee ML, et al: Adverse events associated with testosterone replacement in middle-aged and older men: a meta-analysis of randomized, placebo-controlled trials. J Gerontol A Biol Sci Med Sci 2005; 60(11): 1451-1457; doi: 10.1093/gerona/60.11.1451.
- Stangl TA, Wiepjes CM, Defreyne J, et al: Is there a need for liver enzyme monitoring in people using gender-affirming hormone therapy? Eur J Endocrinol 2021; 184(4): 513-520; doi: 10.1530/EJE-20-1064.
- Wiepjes CM, de Jongh RT, de Blok CJ, et al: Bone Safety During the First Ten Years of Gender-Affirming Hormonal Treatment in Transwomen and Transmen. J Bone Miner Res 2019; 34(3): 447-454; doi: 10.1002/jbmr.3612.
HAUSARZT PRAXIS 2022; 17(11): 6-9