Immediate-type allergies to drugs can cause severe reactions up to and including anaphylaxis. The provocation test is still the “gold standard”, but carries the risk of a renewed allergic reaction. The basophil activation test (BAT) can be helpful here as a complementary laboratory test and an alternative to the provocation test.
In the clinic, it is often difficult to diagnose IgE-mediated drug allergy based on history, skin tests (and specific IgE where present) alone. Often the prick/intradermal test solutions are not available and the preparation of dilutions for skin testing is laborious. In addition, there are few serological tests (IgE) for drugs.
While a positive result can often be considered relevant and conclusive, a negative result is not sufficient to exclude allergy with certainty due to the limited sensitivity. Therefore, provocation with the triggering drug (or with a structurally related preparation as an alternative) is still the “gold standard” for unequivocal diagnosis of immediate-type drug allergy. A certain risk of triggering the allergy again must be accepted. If a number of medications are possible triggers, testing can be complex and expensive and is also not practical in all cases. An in vitro test such as the basophil activation test (BAT) can be helpful here as a complementary laboratory test and an alternative to the provocation test.
Basophilic granulocytes
Basophilic granulocytes (basophils) account for about 1% of leukocytes in peripheral blood. Basophils and mast cells, which are found in tissues and are similar to basophils in function, are the crucial cells for acute allergic reactions. Mast cells as well as basophils can be activated by IgE-dependent and IgE-independent pathways. In this article, we will limit our discussion to IgE-dependent drug allergies.
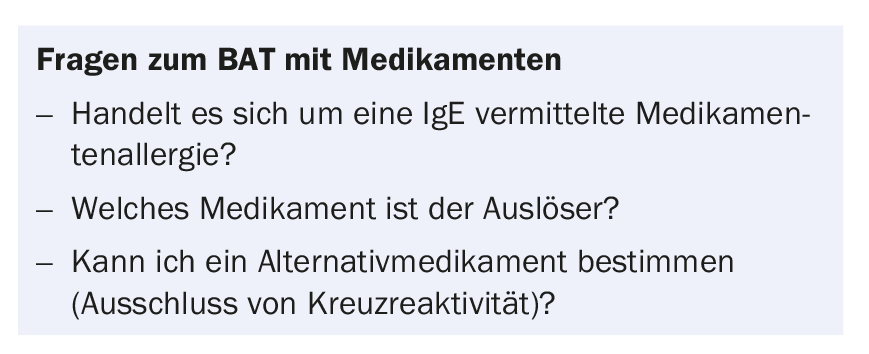
The IgE antibodies bind to the high-affinity IgE receptor (FcεRI) on the surface of basophils and mast cells. Small-molecule drugs often bind to an endogenous protein (e.g., albumin) to form a “new” antigen. This can lead to the formation of specific IgE antibodies via antigen-presenting cells (so-called sensitization). If the drug-specific IgEs at the cell surface are bridged (cross-linked) by binding of the drug-protein complex, the basophils/mast cells are activated and release the mediators stored in their granules, e.g. histamine and heparin, by degranulation (Fig.1A). This leads to the classic symptoms on the skin (flush, urticaria) in case of strong stimulation also bronchospasm, drop in blood pressure up to anaphylactic shock.
Basophil Activation Test (BAT)
The first publications on the analysis of basophil activation by flow cytometry date back to the early 1990s [1]. Meanwhile, the method is routinely offered in various laboratories to diagnose immediate type allergies to drugs. The sensitivity of the BAT for the analysis of drug allergies depends on the drug and is mostly between 50-60%, the specificity is about 80% [2–7]. A positive result therefore strongly points to the drug as the allergen, while a negative result cannot definitively rule out an allergy. Here, the other test results (skin tests, possibly provocation) must also be taken into account.
In BAT, the reaction occurring in the body is “recreated” in the laboratory. The blood is incubated with the presumed triggering drug in pure substance and in increasing concentration , whereby the basophils present in the blood are activated in case of sensitization. In addition to the release of mediators (histamine, heparin), various activation markers (CD63 and CD203c) are also expressed on the surface of basophils, which can be quantified by flow cytometry.
The test is complex and relies on living cells, which requires rapid sample transport (<24h) and protection from cold outside temperatures in the winter months. As a positive control and for internal quality control, the cells are also stimulated with anti-IgE (reactivity) and a bacterial product (fMLP, vitality control) (Fig. 1A, 1B). In addition, 10-15% individuals are IgE nonresponders, thus the basophils cannot be activated via the FcεRI and no statement regarding sensitization with the BAT is possible.
The BAT should be used when there is a reasonable suspicion of drug allergy. The following group of drugs has proven to be particularly suitable: Penicillins, cephalosporins, muscle relaxants, proton pump inhibitors, fluoroquinolones, and various disinfectants (Table 1). If other drugs are tested, the test must still be classified as experimental. In addition, one can use the BAT to analyze cross-reactivities. If, for example, a cephalosporin allergy exists, an initial analysis can be performed with regard to cross-reactivity to penicillins (frequently amoxicillin). However, the tolerability would still have to be tested in re-exposure trials by specialists experienced with this.
Outlook: Indirect basophil activation assay.
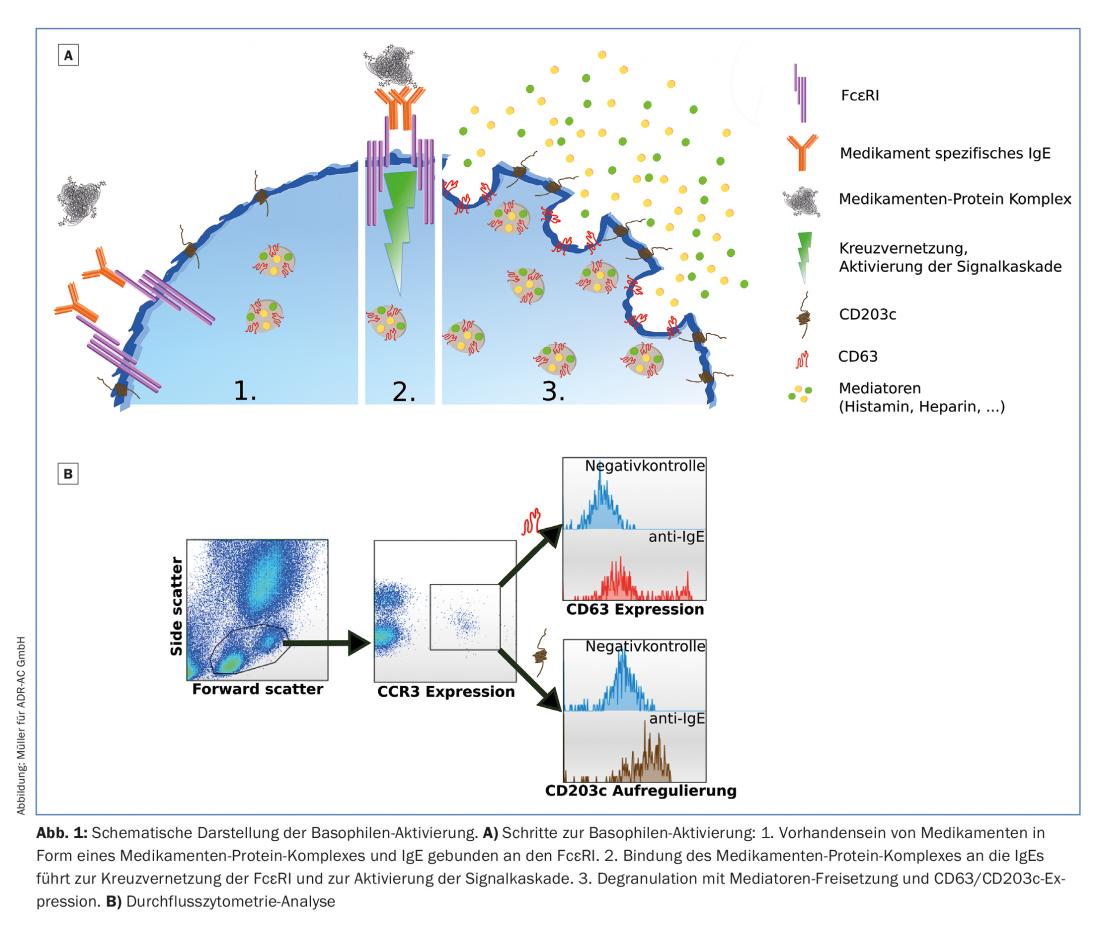
In order to simplify sample transport and allow pooled analysis while addressing the problem of IgE nonresponders, work is currently underway to develop and establish indirect BAT. This involves isolating peripheral blood mononuclear cells (PBMCs), which also contain basophils, from well-characterized donors. Lactic acid treatment is used to reduce the pH until the donor IgEs detach from the basophils (IgE stripping). The “naked” cells are then incubated with the allergy serum, allowing the IgEs contained therein to bind to the donor basophils.
The donor basophils thus re-sensitized can now be stimulated and activated with the controls and drugs as in the usual BAT. Basophil activation is again measured by quantifying CD63 expression using a flow cytometer (Fig. 2).
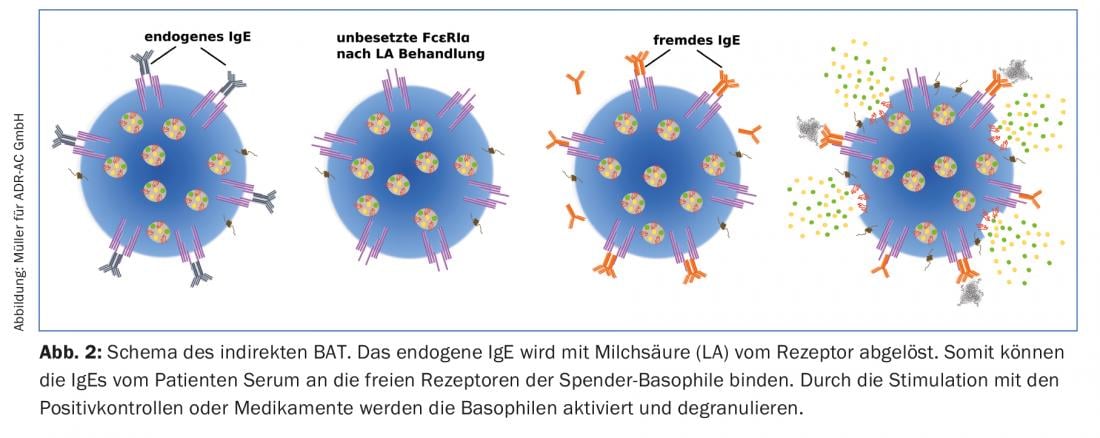
The main advantage of indirect BAT compared to direct BAT is certainly that only serum and not living cells have to be shipped. However, according to initial analysis, the indirect BAT is somewhat less sensitive (about 10%) than the direct BAT. Until now, indirect BAT has only been used for research purposes. To date, the following drugs have tested positive in indirect BAT: Penicillin G, amoxicillin, cefaclor, cefuroxime, ceftriaxone, ceftazidime, cefotaxime, clavulanic acid, carboxymethylcellulose, ibuprofen, chlorhexidine, octenidine, and proguanil (Table 1).
Application of the BAT in the clinic
Clarifications of drug allergies are challenging because different mechanisms and multiple drugs may be involved. Skin testing requires some experience in handling the various drug groups, the appropriate test solutions are often not available, and the test, like the provocation test, carries some risk of recurrence of allergic symptoms. Therefore, clarifications are more and more centralized and, if possible, performed in vitro.
The direct BAT (cell dispatch!) and in the future probably also the indirect BAT (serum dispatch!) can be helpful in this difficult area for a safe diagnosis of drug allergies. Unfortunately, not all drug groups could be evaluated in the BAT yet (Tab. 1) , but the main triggers of drug-induced anaphylaxis have been recorded. Since the test is complex and relatively expensive, it should only be used in cases of well-founded suspicion (Fig. 3), in particular:
- if skin testing is not possible or if the skin test seems too dangerous due to the severity of the initial reaction.
- In case of reactions to different drugs (e.g. perioperative anaphylaxis), or detection or exclusion of cross-reactions (e.g. ceftriaxone allergy) and important indication of possible tolerated drugs (e.g. other beta-lactams).
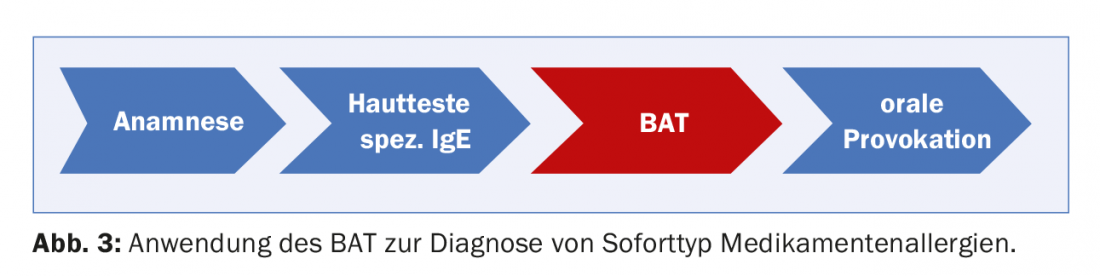
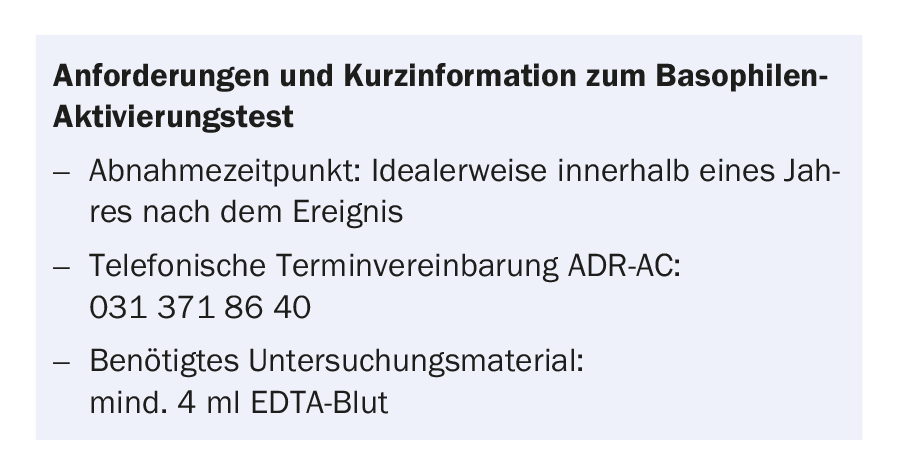
As with the skin test, the sensitivity of the BAT decreases with time interval from the event [8–10]. Ideally, the BAT is performed within one year of the event.
Compared to the provocation test, the BAT is less expensive and there is no further inconvenience for the patient apart from a blood sample. Several drugs can be tested simultaneously in a BAT, so that possible alternatives can also be tested and cross-reactivities can be analyzed in vitro.
Take-Home Messages
- Immediate-type allergies to drugs can cause severe reactions up to and including anaphylaxis.
- Diagnosis is based on history, skin testing, and specific IgE determinations when available.
- The provocation test is still the “gold standard”, but it carries with it
- the risk of a renewed allergic reaction.
- The basophil activation test (BAT) can be helpful here as a complementary laboratory test and an alternative to the provocation test.
Literature:
- Knol EF, et al: Monitoring human basophil activation via CD63 monoclonal antibody 435. The Journal of Allergy and Clinical Immunology 1991; 88: 328-38.
- Aranda A, et al: In Vitro Evaluation of IgE-Mediated Hypersensitivity Reactions to Quinolones. Allergy 2011; 66(2): 247-254.
- Ben Said B, et al: Usefulness of Basophil Activation Tests for the Diagnosis of IgE-Mediated Allergy to Quinolones. Allergy 2010; 65(4): 535-536.
- De Weck AL, et al: Nonsteroidal Anti-Inflammatory Drug Hypersensitivity Syndrome. A Multicenter Study. I. Clinical Findings and in Vitro Diagnosis. Journal of investigational Allergology and Clinical Immunology 2009; 19(5): 355-369.
- Gamboa PM, et al: Basophil Activation and Sulfidoleukotriene Production in Patients with Immediate Allergy to Betalactam Antibiotics and Negative Skin Tests. Journal of Investigational Allergology and Clinical Immunology 2004; 14(4): 278-283.
- Gamboa PM, et al: CD63 Expression by Flow Cytometry in the in Vitro Diagnosis of Allergy to Omeprazole. Allergy: European Journal of Allergy and Clinical Immunology 2003; 58(6): 538-539.
- Gamboa PM, et al: Use of CD63 Expression as a Marker of in Vitro Basophil Activation and Leukotriene Determination in Metamizole Allergic Patients. Allergy: European Journal of Allergy and Clinical Immunology 2003; 58(4): 312-317.
- Blanca M, et al: Natural Evolution of Skin Test Sensitivity in Patients Allergic to Beta-Lactam Antibiotics. J Allergy Clin Immunol 1999; 103: 918-924.
- Romano A, et al: Natural Evolution of Skin-Test Sensitivity in Patients with IgE-Mediated Hypersensitivity to Cephalosporins. Allergy: European Journal of Allergy and Clinical Immunology 2014; 69(6): 806-809.
- Fernández TD, et al: Negativization Rates of IgE Radioimmunoassay and Basophil Activation Test in Immediate Reactions to Penicillins. Allergy 2009; 64(2): 242-248.
DERMATOLOGIE PRAXIS 2018; 28(2): 18-22











