Back and neck pain is a common and distressing health condition. When chronic pain does not respond adequately to either conservative therapy or conventional drug treatment, the use of interventional pain medicine methods may be considered. These are used as part of a multimodal therapy with the goal of reducing pain and improving quality of life.
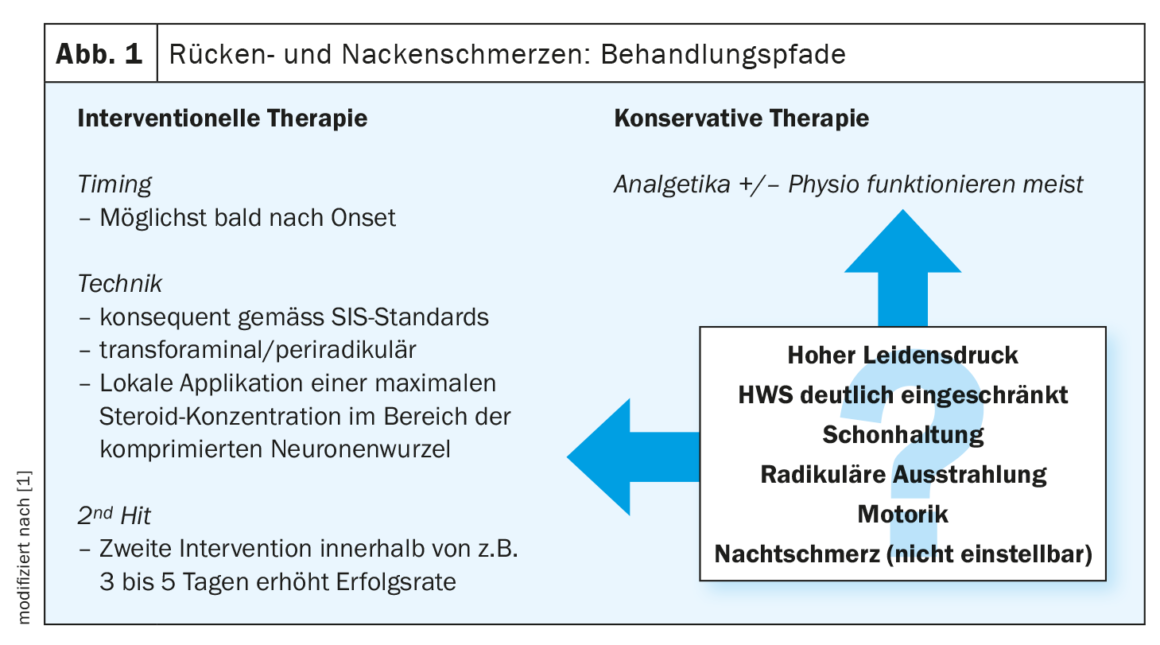
Pain problems are common in the general population. “About 70% of pain patients are treated by primary care physicians,” reported PD Konrad Maurer, MD, Institute for Interventional Pain Medicine, University Hospital Zurich [1]. The frequency of the type of back pain varies depending on the age group, among other factors. While discogenic back pain is most common in young patients, the facet joints or sacroiliac joint are more likely to be the triggers in older patients. “Radicular pain is easiest to diagnose clinically when it is typically also dermatome-specific in presentation and detectable on imaging,” said the speaker [1]. Although back pain usually disappears under conservative therapy (e.g., physiotherapy) or appropriate pain medication, in some cases back pain problems prove to be very persistent (Fig. 1).
Within the framework of a bio-psycho-social concept, the focus is on the following questions: 1. where does the pain signal originate? What kind of pain mechanism is it?, 2. how to tailor therapy to the pain mechanism…, 3. how does the patient cope with the pain in everyday life and how can he be cared for in the respective system?
Deciphering the pain mechanism
What is very central: “We want to find out what the mechanism is that leads to the sensation of pain,” Dr. Maurer emphasized [1].
Nowadays, the following four pain mechanisms are distinguished:
- Nociceptive pain: this is a response to a nociceptive stimulus. This is the “normal” pain, which is necessary to protect physical integrity.
- Nociceptive-inflammatory pain: when an inflammatory component is involved, peripheral nociceptors are activated. The speaker gives the example of a sunburn; when the sunburn is over, the pain also disappears.
- Neuropathic pain: it is a pain phenomenon discrepant to the external impression. A case in point: a patient complains of pain after lung surgery. The scar in the thoracic area looks nice, but anamnestically there is hypersensitivity of the thoracic wall.
- Nociplastic pain: this is the most complex mechanism, there is no nociceptive stimulus, neuronal damage or inflammation, but patients suffer pain sensations. How can this be explained? According to the speaker, “As soon as a pain signal comes from the periphery to the central nervous system, it is transmitted and switched until pain sensation or pain experience can occur in the cortex” [1]. At all these stages, where a switch occurs from one neuron to another, a signal is amplified or attenuated by the nervous system. This is described in the concept of centralized awareness. Thus, 1 pain signal from the periphery may arrive in the central nervous system in the form of 10 pain signals. It can go so far that a stimulus that was not actually a pain stimulus is represented in the central nervous system as a pain sensation.
In ICD-11, chronic pain is officially defined as a disease [2]. This also applies, for example, to fibromyalgia, where the main symptom is pain, but there is no clear explanation for this and no biomarkers are found in the periphery – so a nociplastic pain mechanism is assumed.
Transforaminal steroid infiltration.
The fact that steroid infiltration can achieve rapid relief of symptoms is illustrated by the example of a 34-year-old patient who suffered from severe neck/interscapular pain radiating to the left scapula. The pain also occurred at night, so the patient had sleep problems [1]. His mobility was massively limited and physiotherapy was not possible. Treatment with various medications was unsuccessful. MRI findings revealed a C5/6 left disc herniation (acute radiculopathy). It was decided to perform a transforaminal steroid infiltration and already about one month later the patient could start physiotherapy and resume work.
Radiofrequency therapy and epidural spinal cord stimulation
Another interventional treatment method that can be used to treat hyperexcitable nerve roots is pulsed radiofrequency therapy. This actually involves a neuromodulatory mechanism of action: by treating the neurons with electricity, they become less excitable. For example, in the case of radicular pain problems, a good pain reduction can be achieved by pulsed radiofrequency therapy.
Also a treatment technique from the field of neuromodulation is epidural spinal cord stimulation. Dr. Maurer described the successful use of this treatment method with the help of another case study [1]. A 53-year-old female patient suffered from chronic back pain after several back surgeries (erectile spondylosis with disc replacement, L4 -S1). She reported localized, banded, position- and strain-dependent pain with radiation to both legs. Motor function was unremarkable, hypesthesia was present in the area of the left L5 dermatome. The diagnoses were failed back surgery syndrome (FBSS) and chronic primary musculoskeletal pain (MG 30.02). Treatment attempts using facet joint infiltration, radiofrequency ablation, and pulsed radiofrequency therapy achieved only short-term, unsatisfactory success. The case was discussed in the context of the USZ- Neuromodulation Board. It was agreed that neuromodulatory methods would be used to try to control the pain. Specifically, posterior cord stim ulation (spinal cord stimulation) was performed. Nowadays, this is a minimally invasive reversible procedure that leaves the integrity of the neural structures intact. “We don’t do anything to the structures; it’s purely a functional treatment,” the speaker explained [1]. In the meantime, more than 30 years of experience have been gained with this method [3]. “The neuromodulation technique works well for back pain with a radicular component,” Dr. Maurer explained [1]. In contrast, this method is less suitable for purely spondylogenic, nociceptive pain.
“Anterior Lumbar Interbody Fusion.”
In another case – a 35-year-old female patient suffering from lumbar, non-radiating back pain – an intervention involving screw fixation of the vertebral bodies by means of disc replacement (anterior lumbar interbody fusion) proved to be effective. The provocation test (discography) performed in cooperation with the spinal orthopedics department was positive, whereupon it was jointly decided to perform the anterior lumbar interbody fusion. Regarding discography, Dr. Maurer pointed out that although it is an unpleasant method for patients, it can be used to reliably diagnose discogenic pain [1]. In this patient, the whole procedure had gone well, and the therapy proved to be effective. “Within 2-3 weeks, she was better,” according to the speaker [1]. Opioids were significantly reduced to 30 mg/d morphine equivalent. The patient was then significantly more active in everyday life again and her quality of life improved.
Intravenously administered ketamine
Increasingly, ketamine (i.v.) is being used in low doses in interventional pain medicine. “Ketamine is actually an anesthetic,” Dr. Maurer explained [1]. The active ingredient, which was developed in the 1960s, has an extremely strong analgesic effect. “You can do anesthesia without losing reflexes”. Nowadays, ketamine is also used in rescue medicine and veterinary medicine, for example. Over time, it was found that ketamine had a different effect at low doses. “We call it an anti-hyperalgesic effect,” Dr. Maurer reported [1]. For example, ketamine not only suppresses the pain signal when it arises – i.e., it has an analgesic effect – but it can also be used to treat hyperalgesia very well when administered intravenously, which is an important additional benefit for some patients.
Congress: SGAIM Spring Congress
Literature:
- “Interventional pain medicine as part of a multimodal treatment plan, how and when,” PD Konrad Maurer, MD, SGAIM Spring Congress May 10-12, 2023.
- Maurer K: Chronic pain as an independent disease new in ICD-11. Schweiz Ärzteztg 2020; 101(3334): 977-978.
- Suffer(ing) Threads for Pain Patients, www.mit-schmerzen-leben.de/wp-content/uploads/2020/01/Leidfaden_MitSchmerzenLeben_1019_OT.pdf,
(last call 06/21/2023)
HAUSARZT PRAXIS 2023; 18(7): 34-35