Folliculitis can be distinguished from each other by subtle nuances. The approach is simple: look for the follicular attachment, decide and investigate whether it is infectious or sterile folliculitis; it is important to switch between bacterial, mycotic and viral folliculitis based on clinical signs, microscopy, culture and histopathology for treatment. And not only this; at best, there are more far-reaching consequences with regard to causal research: immunosuppression, for example, poorly controlled diabetes mellitus, atopy, and the necessary remediation of latent systemic infections. Besides, folliculitis is a possible evocation of a more serious skin disease such as pyoderma gangrenosum or acne inversa or lymphoma.
Skin diseases of the hair follicles are their many; and when the hair follicles are accompanied by inflammation, this is by definition folliculitis. Most folliculitides are infectious in nature, so this paper is primarily concerned with them; although sterile follicular dermatoses are also mentioned.
Thus, we must first strive for accurate diagnosis and look for follicular attachment in pustules; this is best done with a dermoscope. There are many non-follicular pustules, especially in acne, accompanied by comedones (except in steroid acne) or in rosacea, Sneddon’s subcorneal pustulosis, seborrheic dermatitis, pustular psoriasis and acute generalized exanthematous pustulosis (a special form of drug allergy). After that, it is about the distinction between infectious and non-infectious folliculitis.
The Pseudomonas folliculitis
Pseudomonas folliculitis is often a disease that reflects leisure time. It occurs with heavy perspiration and with whirlpools contaminated with bacteria. The trunk and lower extremities are often affected, with single, highly inflamed, crusty nodules (Fig. 1).

Histopathology reveals necrotizing folliculitis and microbiology reveals Pseudomonas aeruginosa. Sometimes the germs can even be detected in the sweaty bodysuit (a piece would have to be sent to microbiology). And with the whirlpool need to rethink the hygiene measures.
Therapeutic agents include local imidazoles, erythromycins, metronidazole, and internal quinolones [1].
Pseudomonas also cause a number of other skin infections such as gram-negative Duss infection with foul-smelling maceration between the toes, Pseudomonas paronychia of the nails, green Pseudomonas nail, pseudoerysipelas with lymphangitis, and sometimes tropical ulcer, a mixed infection usually brought back from distant travel.
Malassezia furfur (Pityrrosporon ovale et orbiculare)
Often unrecognized for a long time is a further recreational folliculitis caused by Malassezia Furfur on the trunk, which comes into play in mainly seborrheic skin types (southerners) as well as in cases of increased sweating. Non-productive pustules and some itching are characteristic [2]. The distribution is typically in the sweat ducts, but also often on the shoulders (Fig. 2). The most difficult differential diagnosis is to distinguish it from staphylococcal folliculitis, which produces more pus but may have the same distribution. Also, staphylococci can be found on top in the microscopic examination of malasseziafolliculitis . The Malassezia are then found microscopically in the yeast form and not as pseudomycelia; however, microscopically the double wall is characteristic of yeast as well as the formation of cone figures and clubs. But actually the proof is to be provided by the histological examination, in which the germs should be detectable outside the follicle in the inflammatory infiltrate. A modified agar or Faergemann medium would have to be used for culturing; Malassezia furfur would not grow in routine mycology diagnostics.

Treatment can be attempted with topical selenium disulfite, imidazoles, and zinc pyrithione in shampoo form, but experience suggests that treatment with itraconazole for two weeks is necessary, followed by local prophylaxis.
Other skin diseases dependent on Malassezia include atopic dermatitis in the head and neck region and possibly other regions with appropriate sensitization to Malassezia sympoidalis and other species.
Staphylococcal folliculitis
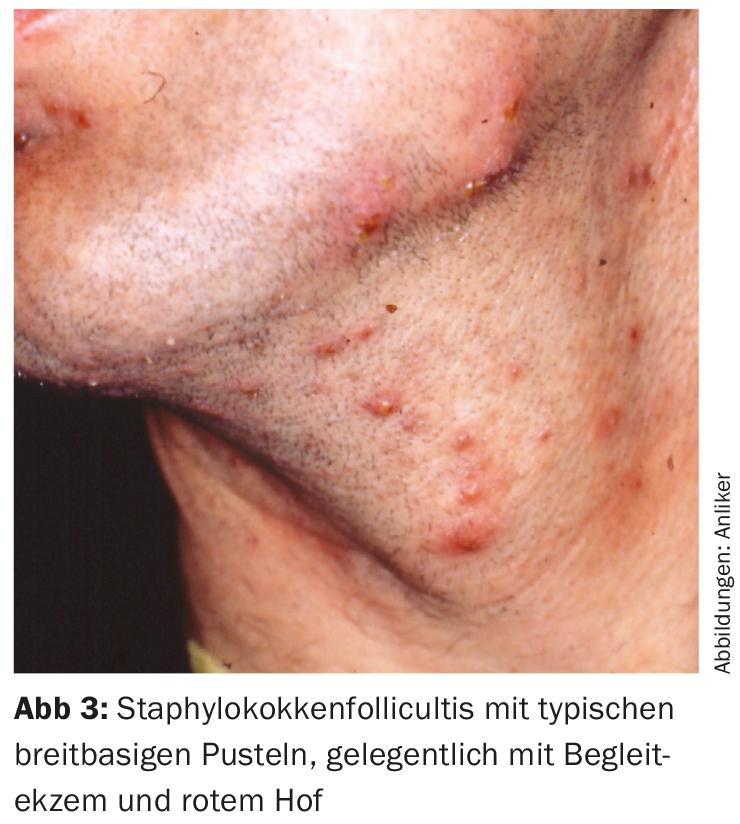
Staphylococcal folliculitis is the frontrunner among hair follicle infections and is very common. Atopics are predisposed to staphylococcal colonization of the skin, but non-atopics are equally affected; however, they will have a less eczematous accompanying component. The pustules in staphylococcal folliculitis are productive and often have a broad-based pustule, a small lake of pus, so to speak, with a hair sticking out (called impetigo Bockhardt) with variable accompanying inflammation and itching (Fig 3). Clues to aetiopathologic germs include superficial abrasion of the skin by staphylococcal enterotoxins, yellowish crusts, and possibly a history of boils, wound healing disorders, or abscesses, which could indicate staphylococcal carriage. In the microscopic preparation, there are often clusters of cocci, whereas these should actually be found outside the follicle for diagnosis (which succeeds in histopathology).
If there is a deeper inflammation and infection, a boil is formed, and if several hair follicles are involved, a carbuncle is formed.
Treatment may be limited to local antibiotics (e.g., fucidic acid) and disinfectant soaps for circumscribed disease. In case of recurrent infections and extensive findings, systemic therapy should be considered, which immediately includes staphylococcal sanitation. This includes systemic antibiosis e.g. with fucidic acid (CAVE fucidin or methillicin resistance!) [3], topical antibiosis, disinfectant soap for showering and a five-day treatment of the inner anterior nasal segment with fucidic acid or mupirocin. The partner of the affected patient and close family members should also, even in the absence of manifestations, treat the nose and perform the disinfecting shower.
Other diseases of the skin involving staphylococci are impetigo contagiosum, bacterial paronychia (Pseudomonas aeruginosa and Candida may also play a role here), activation of atopic eczema and a scattering reaction, maculopapular and disseminated on the arms and legs externally, on the flanks, centrofacially, and dyshidrosiform hand eczema as a so-called staphid reaction.
The candidafolliculitis
Candidafolliculitits is quite rare and common due to local (steroids topical, laser treatment) or systemic immunosuppression. Clinically, small pustules are usually found on a reddened area. The diagnosis is important for the choice of therapy.
Other bacterial/mycotic pathogens
There are a number of other bacterial pathogens that have been described in association with folliculitis such as group G streptococci, Acinetobacter baumanii, and Rhodotorula mucilaginosa [4], although these are quite rare. Sometimes a mixed bacterial infection can occur analogous to the tropical ulcer, which can often be acquired during distant travel. The combination of staphylococci with Malassezia was mentioned above.
The Viral Folliculitis
Viral folliculitis should be mentioned especially in connection with atopic eczema, since an exquisite weakness of the TH1 immune response leads to a defense weakness against intracellular pathogens. Thus, we know the eczema herpeticatum, follicular molluscs, follicular condylomas and follicular warts of other HPV. Of course, other immunosuppression should be considered here, e.g., UV, drug, HIV, lymphoma, etc., if adults are involved and substantial atopy is absent. What is interesting here is that restoring the skin barrier and treating the colonization with staphylococci, and even local steroid therapy, restores the local immune response to fight off the viruses.
The herpes folliculitis
Herpes folliculitis is rare and also suggests local or global immunosuppression. The pustules here are broadly opaque and even hemorrhagic (Fig. 4) and sometimes with grouping of lesions as well as deep skin defects that remain [5]. Yellow crusting and staphylococcal superinfections occur.
Diagnosis is made by the Tschanck test, staining of the smear of the ulcer base with methylene blue, and culture or immunofluorescence detection of HS1 or 2. In the Tschanck test or histology, syncytial giant cells and inclusion bodies are prominent.

The demodicose
Demodicosis occupies a special position, which is the only folliculitis with parasites, the hair follicle mite. Mostly it occurs centrofacially with follicular, strongly reddened papules and this on the base of rosacea (Fig. 5) . The detection of hair follicle mites under the microscope helps to establish the diagnosis and opens up the possibility of therapy with 5% permethrin cream, whereas the usual rosacea therapies may fail.

Other folliculitides in the differential diagnosis
Eosinophilic folliculitis Ofuji: A rare, immunosuppression-related folliculitis that is sterile and most common in Japan to date. The small erythematous pustules occur on normal-colored skin and are conspicuously filled with eosinophil granulocytes on histopathology. Immunosuppression is actually a condition for the development of this disease so far, but we diagnosed folliculitis in a patient on an old burn scar (local immunosuppression?), which histopathologically and with sterile pustules could not be interpreted differently than eosinophilic folliculitis.
Acne inversa: Here folliculitides are almost always present and announce the activity of the disease. Although bacteria can be isolated and acne inversa responds to acne antibiotics and others, their role in disease development is not certain.
Pyoderma gangrenosum: Pyoderma gangrenosum also begins with a sterile pustular folliculitis. This starts lymphohistiocytic and then heralds severe neutrophilic inflammation with subsequential ulceration. Histopathologically, folliculitides can be instrumental in establishing the diagnosis.
Follicular dermatoses: A whole range of dermatoses are either follicular or can appear as follicular variants. In the former group, dyskeratosis follicularis Darier, pruriginous folliculitis, hemorrhagic folliculitis in vitamin C deficiency, EGFR- and TKI-associated pustulosis, mucinosis follicularis (localized T-cell lymphoma) and others more should be mentioned; in the latter, for example, follicular atopic eczema, follicular lichen ruber, etc.. However, these are not pustular except for EGFR and TKI induced folliculitis.
Conclusion
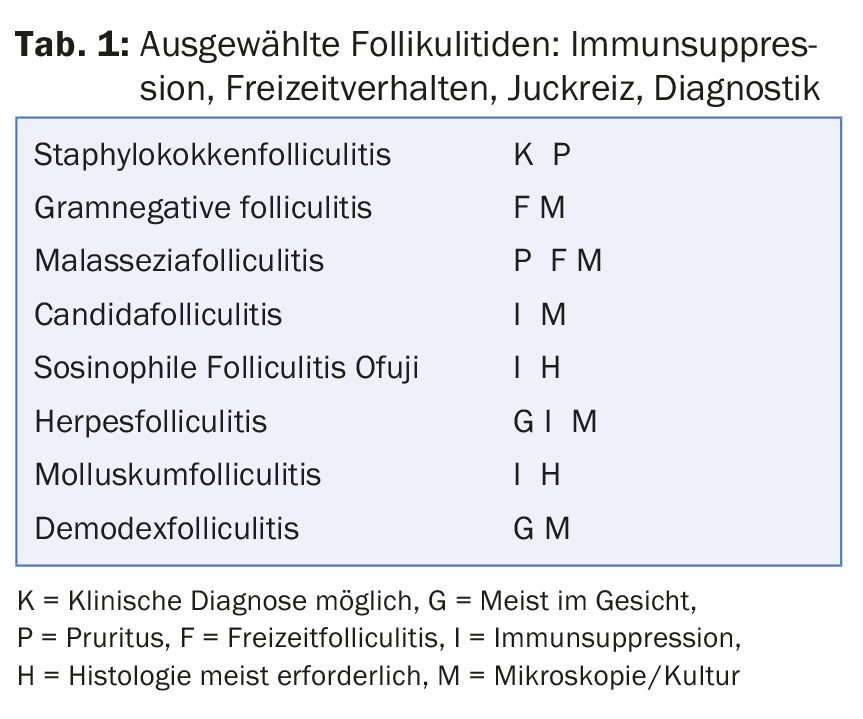
Folliculitis can be distinguished from each other by subtle nuances. If this fails clinically or if therapy does not help, microscopic examination of the pustule contents, culture, and finally histopathologic examination should be resorted to in order to establish a clear diagnosis. Attention should be paid to activities (recreation, whirlpool), immune status, and concomitant factors such as atopy, occlusion, and diabetes mellitus(Table 1). The approach is simple: look for follicular binding, decide and investigate whether it is infectious or sterile folliculitis; then the switch between bacterial, mycotic and viral folliculitis is important for treatment. Not only this; at best, there are more far-reaching consequences with regard to causal research: immunosuppression, for example, poorly controlled diabetes mellitus and the need for remediation of latent systemic infections. Besides, folliculitis is a possible evocation of a more serious skin disease such as pyoderma gangrenosum, lymphoma or acne inversa.
Literature:
- Teraki Y, et al: Rubbing skin with nylon towels as a major cause of pseudomonas folliculitis in a Japanese population. J Dermatol 2015; 42(1): 81-3.
- Del Rosso JQ, et al: When acne is not acne. Dermatol Clin 2016; 34(2): 225-8.
- Hunter C, et al: Methicillin-Restistant Staphylococcus aureus Infections: A Comprehensive Review and va Plastic Surgeons Approach to the Occult Sites, Plast Reconstr Surg 2016;138 (2): 525-23.
- Jaeger T, Andres C, Ring J, Anliker MD: Rhodutorula mucilaginosa infection in Li-Fraumeni-like syndrome: a new pathogen in folliculitis.Br J Dermatol 2011; 164(5): 1120-2.
- Anliker MD, Itin P: Herpetic folliculitis barbae. A rare cause of folliculitis. Dermatologist 2003; 54(3): 265-7.
DERMATOLOGIE PRAXIS 2017; 27(1): 5-8