Inflammatory myopathies may be idiopathic or pathogen-induced. It is also found concomitantly in collagenoses, granulomatoses, and malignant and paraneoplastic syndromes. Imaging diagnostics are primarily performed by magnetic resonance imaging, as are follow-up examinations during and after therapy.
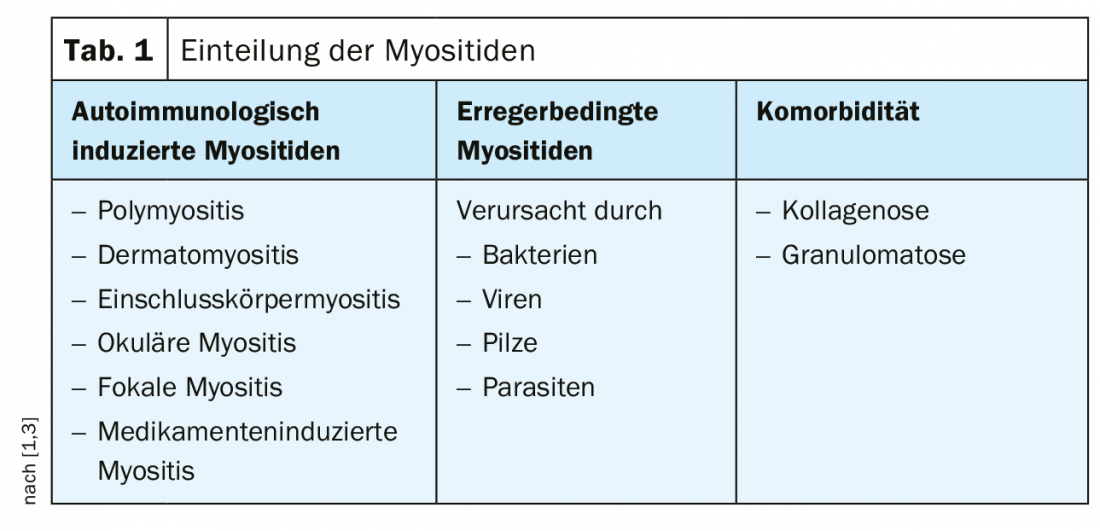
In terms of early diagnosis, differential diagnosis, and differential therapy, inflammatory myopathies can be problematic [1]. Often, image morphologic follow-up is necessary, since a lack of specificity of muscle serum enzymes, reduced graduability of clinical parameters, and the limited informative value of biopsy (small sample volumes, incomplete specificity of the cellular infiltrate) sometimes make an immediate diagnostic assignment primarily impossible. Inflammatory myopathies can be pathogenetically divided into autoimmunologic and pathogen-induced myositis, but can also occur as comorbidity in the context of other diseases (Table 1).
Inclusion body myositis accounts for approximately 20% of inflammatory myopathies, has its disease peak approximately between the ages of 50 and 70, and a sex distribution of 3:1 (males:females). Muscular atrophy, paresis, dysphagia, dysphonia and dysarthria with a slowly progressive course characterize the clinical presentation. Polymyositis and dermatomyositis are relatively rare, with a combined annual incidence of about 1:100,000, and can occur in all age groups, although polymyositis is uncommon in childhood. Main clinical symptoms are dysphagia with 30-50%, muscle pain with 50% and arthralgias with 20-30% share. The important differential diagnostic criteria are summarized in Table 2.
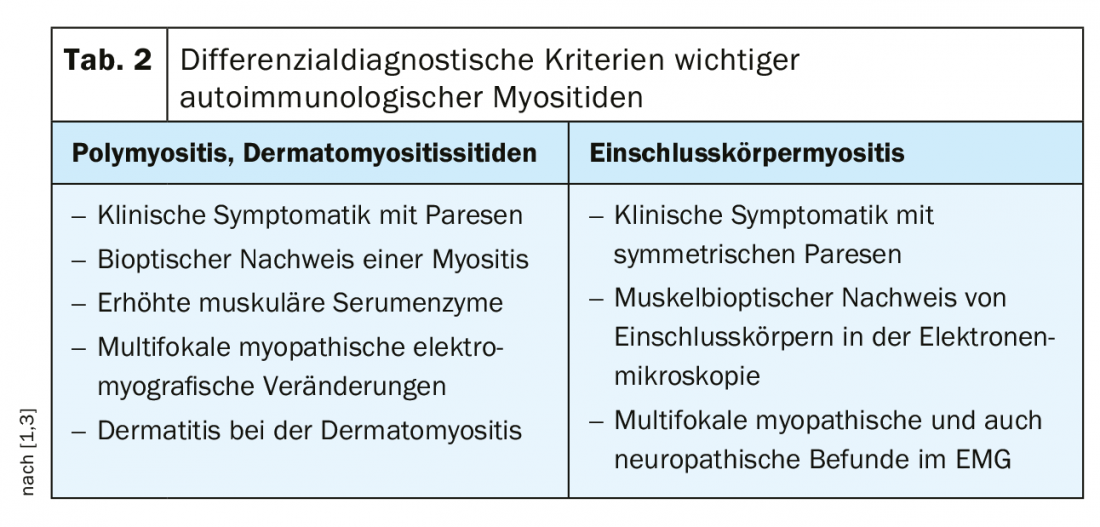
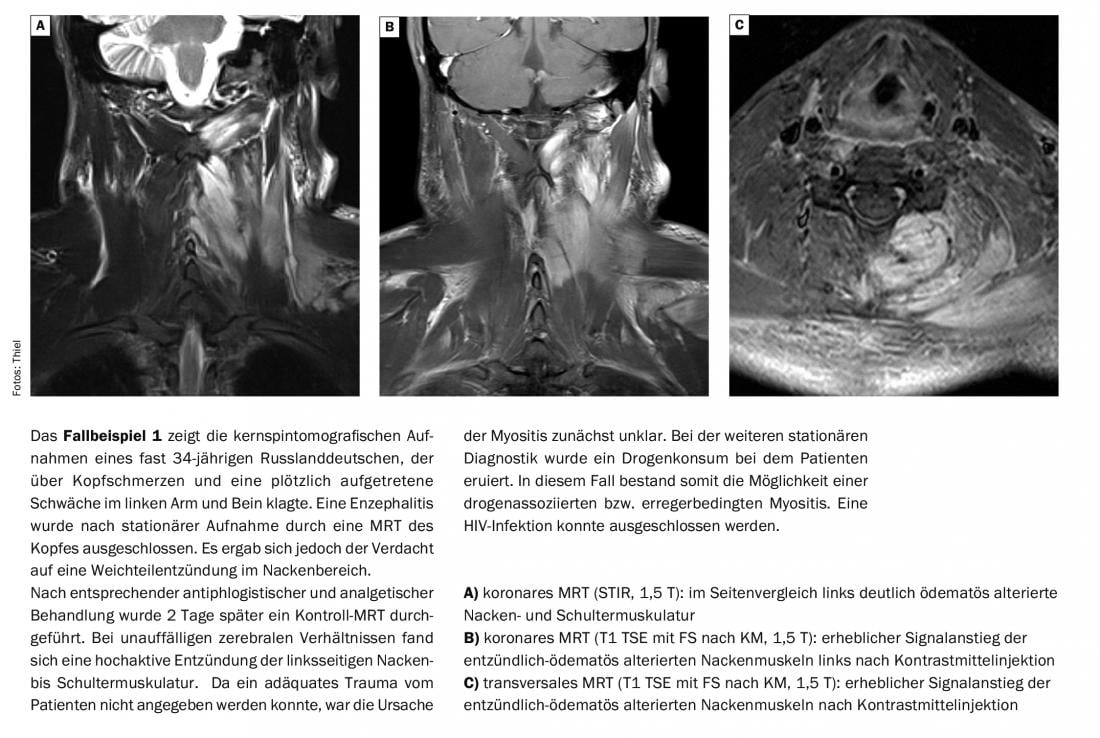
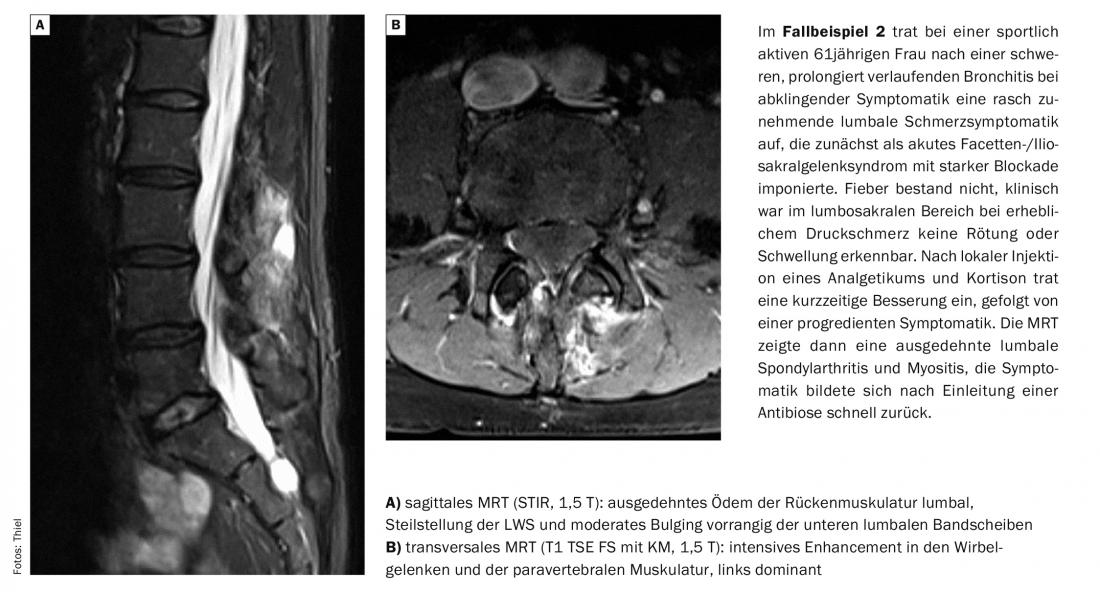
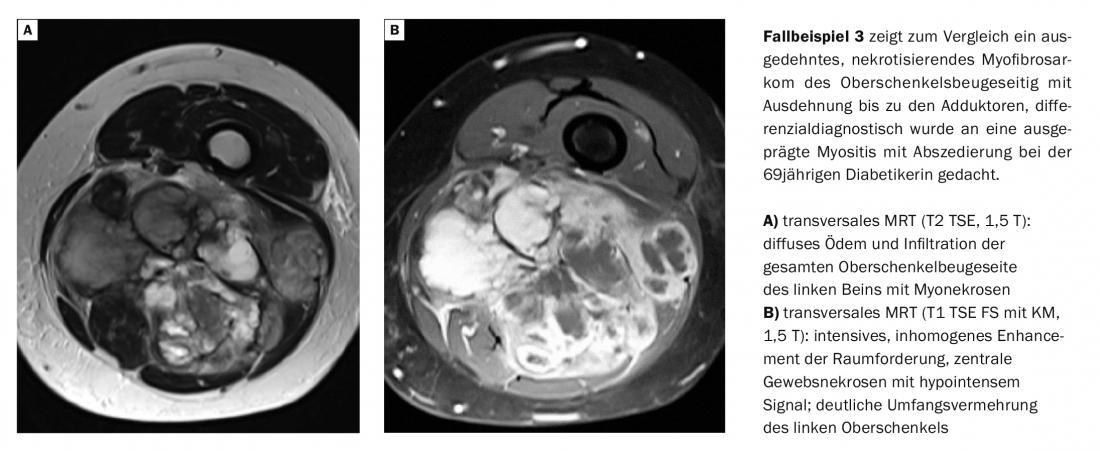
Inflammatory myopathies are increasingly observed as a complication of HIV infection in up to 72% of cases [2]. Image morphologically, abscessing myositis can be difficult to differentiate from myosarcoma with tumor necrosis [3].
Computed tomographic examinations in the primary diagnosis of inflammatory myopathies, like radiographs, ultrasound, and nuclear medicine procedures, are only of complementary value [4]. However, HR-CT has great importance in the context of pulmonary diagnosis in the collagenoses or granulomatoses [5]. Similarly, it is important to exclude inflammatory muscle disease as a comorbidity in malignant and paraneoplastic syndromes. In these cases, PET-CT imaging should be favored [6]. Computed tomography offers advantages over magnetic resonance imaging in the diagnosis of myositis ossificans with visualization of early muscular calcifications [7].
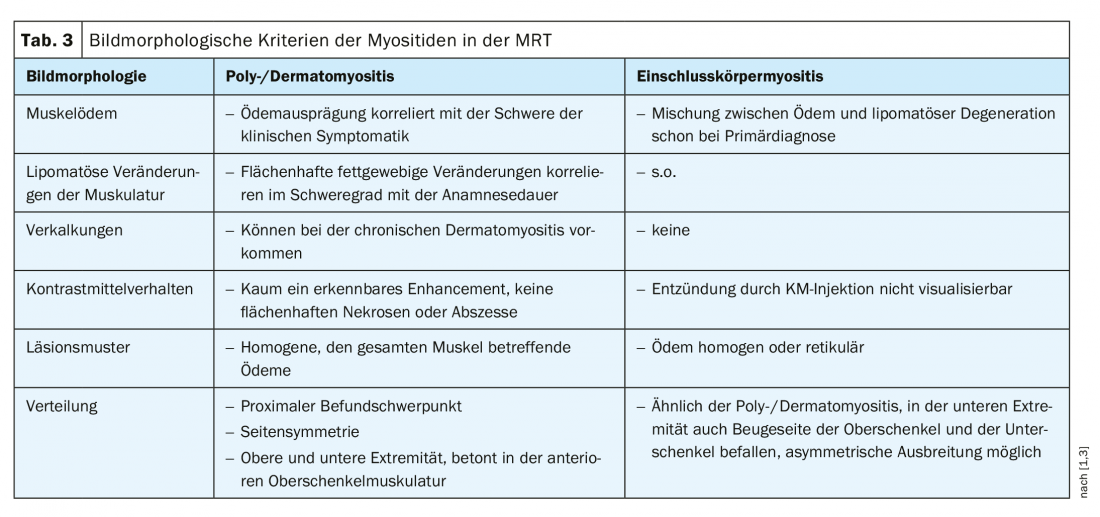
In magnetic resonance imaging (MRI) studies, image morphologic criteria can help differentiate myositis [1,8], which are listed in Table 3.
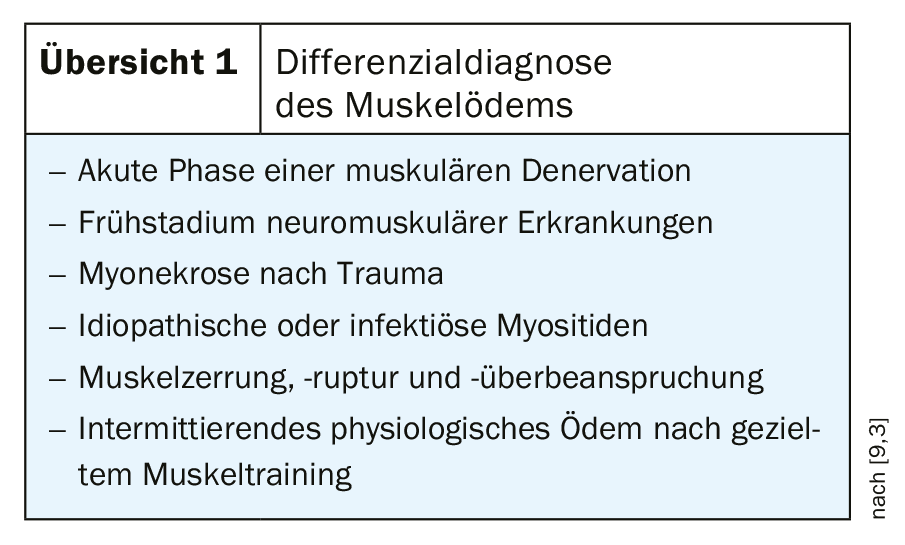
Focal myositis differs in the pattern of involvement (single muscle or muscle compartment affected) and shows marked contrast enhancement without abscessation or tissue necrosis. Individual muscles of the lower leg are primarily affected. Calcifications are common in parasitic myositides, and intense contrast reactions accompanied by tissue necrosis and abscesses are almost regular in pathogen-induced myositides. The edematous tissue reactions require the use of fat suppressive sequences for reliable detection [9]. However, edema detection is not only an expression of inflammation, as overview 1 shows in terms of differential diagnosis.
Magnetic resonance imaging enables prompt diagnosis and symptom-adapted treatment. This can reduce the risks of misdiagnosis and delay in therapy [4]. MRI also represents an important tool in biopsy planning; specific information about the location and extent of muscular inflammation can be obtained. An important criterion for the extension of the biopsy is the MR tomographic finding of the extension of the inflammation to the muscle fascia, which should then be biopsied as well.
Take-Home Messages
- Inflammatory myopathy is divided into autoimmunologic vs pathogen-induced etiology.
- Complementary to determination of muscle serum enzymes, biopsy and other clinical parameters, imaging techniques are important diagnostic tools.
- Computed tomography or PET-CT may be used to clarify comorbidity, and magnetic resonance imaging (MRI) in all other cases.
- Intravenous contrast injection is not mandatory for the diagnosis of myositis, but may be helpful in pathogen-induced muscle inflammation for visualization of an abscess.
Literature:
- Beese M, Winkler G: MRI of the musculature. Stuttgart, New York: Georg Thieme Verlag 1997: pp. 129-172.
- Booth TC, Chhaya NC, Bell JR, Holloway BJ: Skeletal Radiol 2012; 41(11): 1349-1363.
- Thiel HJ: MTA Dialog 9/2013; 14: 840-843.
- Turecki MB, et al: Imaging of musculoskeletal soft tissue infections. Skeletal Radiol 2010; 39(10): 957-971.
- Lundberg IE, Alexanderson H: Technology insight: tools for research, diagnosis and clinical assessment of treatment in idiopathic inflammatory myopathies. Nat Clin Pract Rheumatol 2007; 3(5): 282-290.
- Al-Nahhas A, Jawad AS: PET/CT imaging in inflammatory myopathies. Ann N Y Acad Sci 2011; 1228: 39-45.
- Kim SW, Choi JH: Myositis ossificans in psoas muscle after lumbar spine fracture. Spine (Phila Pa 1976) 2009; 34(10): E367-370.
- Tomasová Studynková J, Charvát F, Jaradosá K, Vencovsky J: The role of MRI in the assessment of polymyositis and dermatomyositis. Rheumatology (Oxford) 2007; 46(7): 1174-1179.
- Burgener FA, Meyers SP, Tan RK, Zaunbauer W: Georg Thieme Verlag 2002: pp. 334.
HAUSARZT PRAXIS 2019; 14(11): 31-33