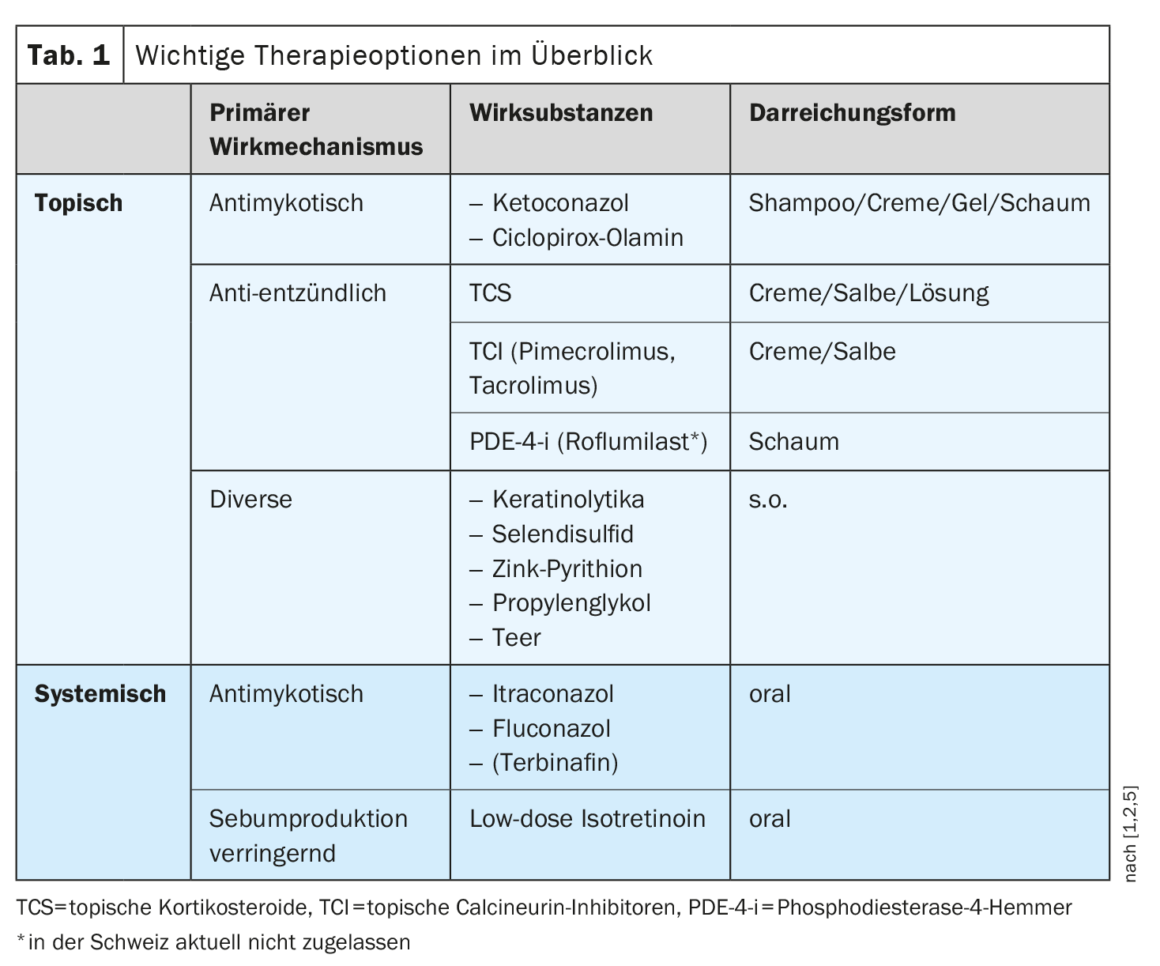
In addition to antifungal shampoos for scalp infestations, topical preparations with keratolytic and anti-inflammatory properties are among the classic measures for seborrhoeic eczema. In adults and older children, products containing TCS, TCI, ketoconazole or ciclopirox-olamine can be used for topical treatment. There are also many other active substances that can be considered. In severe cases, systemic treatment with azoles or low-dose isotretinoin may be considered.
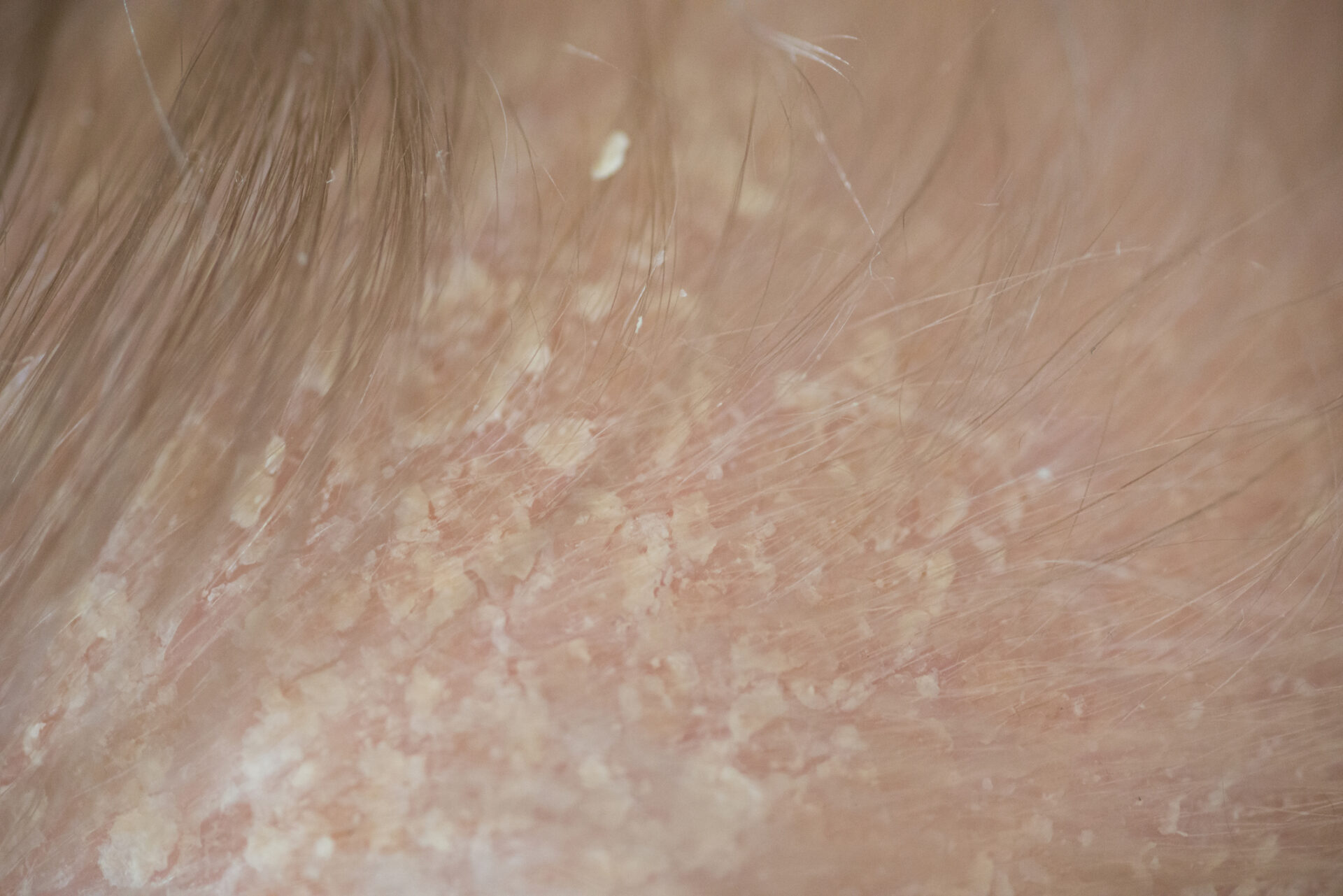
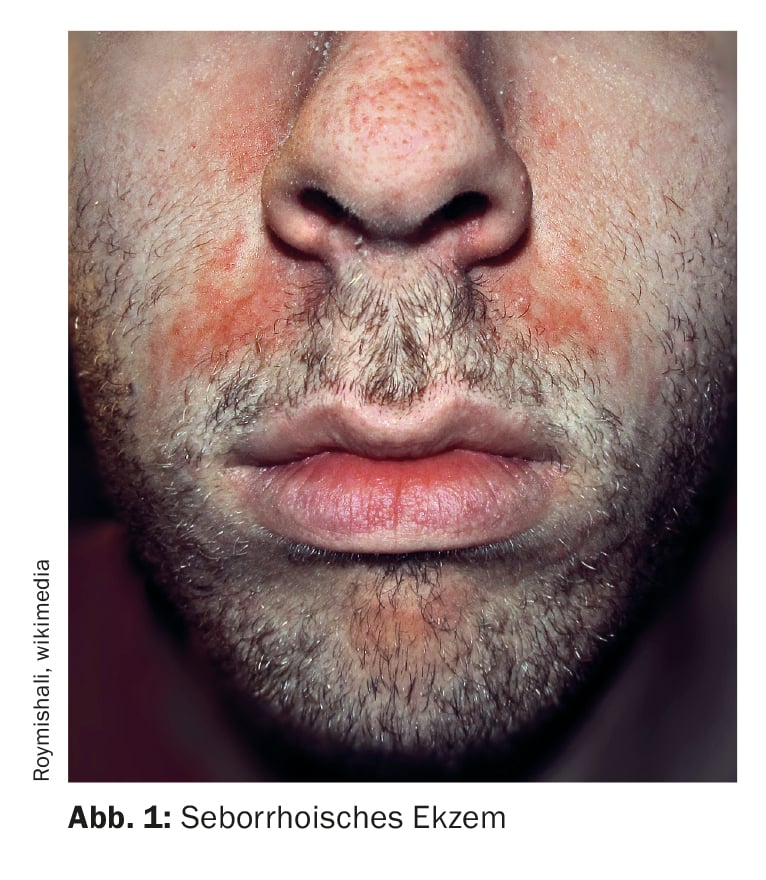
On the occasion of the annual meeting of the EADV (European Academy of Dermatology and Venerology), Prof. Marie L. Saunte MD/PhD, University of Copenhagen (DK) gave a lecture on seborrheic dermatitis [1]. According to current knowledge, the pathophysiology of this chronic recurrent disease is based on the interplay of a genetically determined overactivity of the sebaceous glands and the resulting excessive colonization with the physiological yeast Malassezia furfur. Accordingly, seborrheic dermatitis is classified as a Malassezia-associated skin disease and occurs preferentially in areas of skin rich in sebaceous glands such as the midface, chest, back or skull [2]. The altered skin flora favors inflammatory immune reactions. “Colonization with Malassezia triggers inflammation,” summarized the speaker. The clinical picture is characterized by erythema and small papules/pustules covered with grey, white or yellowish scales.
Current treatment options
The incidence of seborrheic eczema is highest in the following age groups: infants under three months, adolescents and young adults and over 50s [3,4]. Seborrhoeic dermatitis is more common in HIV/AIDS patients and people with neurological disorders (e.g. Parkinson’s disease) and men are generally more frequently affected than women. Seborrhoeic eczema in infants is also known as seborrhoidal dermatitis infantum and is usually self-limiting; seborrhoeic eczema in older children, on the other hand, is characterized by a chronic, recurrent course. The therapeutic approach depends on the severity and ranges from topical to systemic agents, with most patients benefiting most from a multimodal approach [5].
Infants/toddlers: Predilection sites include the hairy scalp (cradle cap, gneiss) and intertriginous areas. Olive oil alone or with the addition of 2% salicylic acid can be used to remove the scales [6]. Afterwards, creams or lotions containing corticosteroids (strength class 1) can be applied for a short time. Vioform zinc oil (0.5%) is recommended for the treatment of intertriginous areas. Symptoms can also be alleviated by adding anti-inflammatory additives (e.g. wheat bran extract) or oil to baths with lukewarm water.
Adults/adolescents and older children: Shampoos with keratolytic and antimicrobial additives (selenium disulfide, zinc pyrithione, salicylic acid or tar) can be used in cases with mild scalp infestation [5]. If this is not sufficient, long-term therapy with washing solutions containing ketoconazole, clotrimazole or ciclopirox can reduce excessive yeast colonization [7]. For seborrheic eczema on the face or body, creams containing ketoconazole or ciclopirox can be considered [7]. Secondary analyses confirm the efficacy and safety of these topical antimycotics [11].
If long-term control of the inflammatory reaction is required, the use of topical steroids (TCS) or topical calcineurin inhibitors (TCI: pimecrolimus, tacrolimus) is recommended [5]. Case reports indicate that the use of TCI can achieve similar efficacy to TCS such as hydrocortisone 1% or betamethasone 0.1% [5]. In addition to an immunomodulating effect, an antifungal effect against Malassezia yeasts has also been demonstrated [2,8]. For non-scaling seborrheic eczema, the intermittent use of weaker TCS (e.g. desonide 0.05% and/or 1% hydrocortisone) twice daily for 5 to 7 days in combination with an imidazole may be effective [5,9,10]. In addition, various salts have also been shown to be effective, such as lithium succinate, which appears to impair the availability of the lipids required for Malassezia growth [12]. In cases of rapidly recurring seborrhoeic dermatitis or if the symptoms prove refractory to the treatment options mentioned, the use of systemic antifungal agents such as itraconazole or fluconazole can provide relief [13].
In clinical studies, 0.3% roflumilast foam – a highly potent and selective phosphodiesterase 4 inhibitor – has proven effective as a new topical treatment option for moderate to severe seborrheic eczema [5,14]. In addition to significant placebo superiority in terms of IGA (Investigator’s Global Assessment) at week 8, topical PDE-4-i significantly reduced itching, scaling and erythema and was generally well tolerated [5,14].
Congress: EADV Annual Meeting
Literature:
- “Malassezia-related skin diseases”, Prof. Marie L. Saunte MD/PhD, EADV Annual Meeting, 10.-14.10.2023
- Saunte DML, Gaitanis G, Hay RJ: Malassezia-Associated Skin Diseases, the Use of Diagnostics and Treatment. Front Cell Infect Microbiol. 2020 Mar 20; 10: 112. doi: 10.3389/fcimb.2020.00112.
- Dessinioti C, Katsambas A: Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Clin Dermatol 2013; 31: 343-351.
- Jackson JM, et al: Unmet needs for patients with seborrheic dermatitis. J Am Acad Dermatol 2022 Dec 17:S0190-9622(22)03307-2.
- Desai S, McCormick E, Friedman A: An Up-to-Date Approach to the Management of Seborrheic Dermatitis. J Drugs Dermatol 2022; 21(12): 1373-1374.
- Meurer M, Aschoff R, Gahr M: Dermatology. Pediatrics 2019: 777-798.
- “Seborrheic eczema”, https://flexikon.doccheck.com/de/Seborrhoisches_Ekzem,(last accessed 16.11.2023)
- Sugita T, et al: A new calcineurin inhibitor, pimecrolimus, inhibits the growth of Malassezia spp. Antimicrob. Agents Chemother 2006; 50: 2897-2898.
- Kastarinen H, et al: Topical anti-inflammatory agents for seborrhoeic dermatitis of the face or scalp. Cochrane Database Syst Rev. 2014;2014(5): CD009446.
- Del Rosso J: Adult seborrheic dermatitis: a status report on practical topical management. J Clin Aesthet Dermatol 2011;4(5): 32-38.
- Okokon EO, et al: Topical antifungals for seborrhoeic dermatitis. Cochrane Database Syst Rev 2015; 25: CD008138 10.1002/14651858.CD008138.pub2
- Mayser P, Schulz S: Precipitation of free fatty acids generated by Malassezia- a possible explanation for the positive effects of lithium succinate in seborrhoeic dermatitis. JEADV 2016; 30, 1384-1389.
- Gupta AK, Richardson M, Paquet M: Systematic review of oral treatments for seborrheic dermatitis. JEADV 2014; 28: 16-26.
- Draelos ZD, Forman SB, Green LJ: Roflumilast foam 0.3% treatment of seborrheic dermatitis is effective and safe and improves patient quality of life: Results from a phase 2 study. JAAD 2022; 87(3), Supplement AB105.
DERMATOLOGIE PRAXIS 2023; 33(6): 32-33 (published on 12.12.23, ahead of print)