Irritable bowel syndrome (IBS) and other functional disorders are among the most common chronic complaints in children and adolescents. A confirmed diagnosis allows the initiation of the necessary therapy. According to the guideline updated last year, the Rome criteria are to be used for this purpose.
Functional abdominal pain can be associated with significant impairment of quality of life [1]. Data from Germany report a frequency of IBS of 4.9% in children 6-10 years of age; girls are more commonly affected than boys [2]. According to the S3 guideline updated in 2021, RDS is present if all 3 of the following points are fulfilled [1]:
- Over >3 months of persistent or recurrent symptoms such as abdominal pain or bloating, usually accompanied by changes in bowel movements
- the patient seeks help because of these complaints and/or is in such strong concern that the quality of life is relevantly affected by them
- there are no changes characteristic of other clinical pictures that are probably responsible for these symptoms.
Functional gastrointestinal complaints in children and adolescents are understood according to Rome IV as disorders of the interaction between the central nervous system and the gut and are often associated with anxiety, depression, stress and psychological trauma [3,4].
Why the Rome criteria should be used
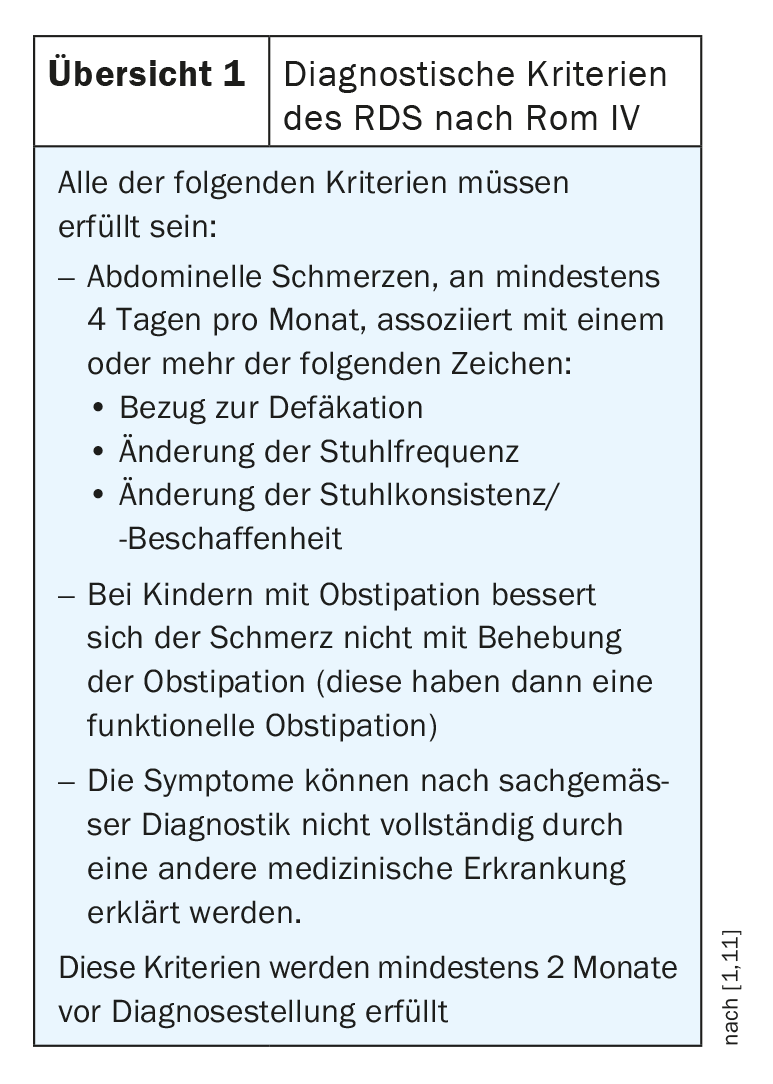
The Rome criteria for children and adolescents (Overview 1) are designed not to diagnose IBS on the basis of symptoms alone, but to gradually exclude other organic pathologies to avoid repeated investigations. The guideline authors state that the main somatic differential diagnoses can be excluded by a simple and limited diagnostic workup strategy.
The most important arguments for the use of the Rome criteria at a glance:
- Applicability and validity of the Rome criteria have been demonstrated by several studies. According to this, by applying the Rome III criteria, more than 8% of children and adolescents with chronic abdominal pain can be classified, and the diagnosis of “irritable bowel syndrome” can be made in about 40-50% of cases [5,6]. Due to changes in the Rome IV definition, the prevalence of diagnoses is expected to be lower but the distribution unchanged [7].
- Alternative consensus criteria or evaluated criteria for children and adolescents do not exist.
- Until the age of about 8-12 years, the localization and character of the complaints cannot be well specified by the children themselves. The diagnosis must therefore be based largely on information provided by the parents. The Rome definition provides some assistance in this regard in the form of observable criteria.
- Most of the few available studies on diagnosis and therapy are based on the Rome definition.
What are the “red flags” to watch out for?
To exclude other diseases with abdominal pain and changes in bowel movements, a careful history and clinical examination must be performed. Alarm symptoms suggestive of possible organic pathology should be targeted: Weight loss, decrease in growth rate; gastrointestinal (including occult) blood loss; significant vomiting; chronic, severe diarrhea; persistent right upper abdominal pain or right lower abdominal pain; unexplained fever; positive family history for inflammatory bowel disease [8]. Psychological and social factors and other possible triggers of the complaints, such as intestinal infections, should also be recorded. The following laboratory tests are recommended:
- BB, CRP and/or ESR, lipase, GPT, gamma-GT, ges IgA, tissue transglutaminase IgA-AK, TSH, creatinine, blood sugar
- Urine status
- Stool for Giardia-lamblia antigen, Dientamoeba fragilis, worms.
- Stool tests for fecal inflammation markers (calprotectin or lactoferrin).
In addition to IBS, the Rome IV criteria clinically define functional abdominal pain, functional dyspepsia, cyclic vomiting, and abdominal migraine [9]. WHEREAS, a continuum of functional abdominal disease is assumed [3,10].
Literature:
- Layer P, et al: Update S3-Leitlinie Irritable Bowel Syndrome: Definition, Pathophysiology, Diagnosis and Therapy. Joint guideline of the DGVS and the DGNM, June 2021 – AWMF registration number: 021/016.
- Gulewitsch MD, et al: Rome III criteria in parents’ hands: pain-related functional gastrointestinal disorders in community children and associations with somatic complaints and mental health. Eur J Gastroenterol Hepatol 2013; 25: 1223-1229.
- Drossman DA: Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology 2016; 19: S0016-5085.
- Schmulson MJ, Drossman DA: What Is New in Rome IV. J Neurogastroenterol Motil 2017; 23: 151-163.
- Baber KF, et al: Rome II versus Rome III classification of functional gastrointestinal disorders in pediatric chronic abdominal pain. J Pediatr Gastroenterol Nutr 2008; 47: 299-302.
- Helgeland H, et al: Diagnosing pediatric functional abdominal pain in children (4-15 years old) according to the Rome III Criteria: results from a Norwegian prospective study. J Pediatr Gastroenterol Nutr 2009; 49: 309-315.
- Saps M, et al: Construct validity of the pediatric Rome III criteria. J Pediatr Gastroenterol Nutr 2014; 59: 577-581.
- Di Lorenzo C, et al: Chronic abdominal pain in children: a clinical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2005; 40: 245-248.
- Saps M, et al: Construct validity of the pediatric Rome III criteria. J Pediatr Gastroenterol Nutr 2014; 59: 577-581.
- Friesen CA, Rosen JM, Schurman JV: Prevalence of overlap syndromes and symptoms in pediatric functional dyspepsia. BMC Gastroenterol 2016; 16: 75.
- Hyams JS, et al: Functional Disorders: Children and Adolescents. Gastroenterology 2016; 15: S0016-5085
HAUSARZT PRAXIS 2022; 17(6): 22