For patients with rheumatic diseases, pain is the central problem. However, recent studies show that influencing pain experience with biologics is possible and that JAK inhibitors can provide rapid, direct improvement in acute, severe pain that is not due to inflammation reduction. However, conventional analgesics should still be used if needed.
Moderate to severe pain, corresponding to a score of 7-10 on the visual analog scale (VAS), usually actually decreases in rheumatoid arthritis (RA) over the course of the disease, which can also be attributed to improved therapies. According to data from the core documentation of the German Rheumatism Center Berlin, 26% of patients still reported feeling severe pain in 2001. In 2018 and 2019, it was only 14 to 15%. Nevertheless, pain continues to significantly affect the quality of life of patients with RA.
Few sufferers reported having low pain or named a score of 4-6 on the VAS pain scale. The proportion of patients with severe pain is high in inflammatory rheumatic diseases. For ankylosing spondylitis, the proportion of those with moderate and severe pain was 17% to 18% in 2019. The values were somewhat lower in patients with lupus. But even here, about 10-11% have severe pain. Regardless of age or disease duration, patients indicated that pain was the problem that most limited their quality of life, ahead of difficulties in coping with everyday life, reduced mobility, or anxiety. Drug therapies are intended to provide relief.
Opioids for pain reduction
For severe pain, patients with RA, ankylosing spondylitis (AS), psoriatic arthritis (PsA), and systemic lupus erythematosus (SLE) are prescribed opioids proportionately to reduce pain. In this regard, a Cochrane analysis [1] found that these were superior to placebo in terms of pain reduction. They were not superior in the number of discontinuations due to inadequate analgesia (RR 0.82; 95% CI 0.34-2.0). The rate of discontinuation of therapy under opioids could be attributed more frequently to side effects such as nausea, vomiting dizziness or constipation. Yet opioid prescriptions are increasing [2]. Therapy recommendations are moving towards the use of opioids for severe pain, as shown not only by the core documentation of the German Rheumatism Center Berlin but also by the American Corrona Registry.
Anti-inflammatory treatment
Pain can also be reduced by successfully treating the inflammation that can trigger it. This was studied in the Canadian Early Arthritis Cohort (CATCH) with 1270 patients who had a mean symptom duration of 5.8 months [3]. As a result, of the patients with early RA who had received one year of anti-inflammatory treatment, only 24% still had permanent pain >4 according to the Numeric Rating Scale (NRS). At the beginning of therapy, the figure was 64%. An NRS score <4 corresponds to the Patient Acceptable Symptom State (PASS) a pain that is just tolerable for patients. Wide Spread pain (o. Fibromyalgia-RA) felt 9% initially and only 5% after one year of anti-inflammatory treatment.
Pain reduction through cytokine modeling therapy
Cytokines play a major role in understanding pain. As messenger substances, they influence pain transmission at different levels, as proinflammatory and anti-inflammatory cytokines, up to the spinal cord as well as ultimately supraspinal. Cytokines are able to cross the blood-brain barrier and send inflammatory signals from the periphery to the central nervous system.
This is possible both through holes in the circumventricular organs and via various transport mechanisms that actively transport cytokines or other substances across the blood-brain barrier. Via the vagus nerve, the signals reach the central nervous system (CNS), so that proinflammatory cytokines arrive there accordingly or also information that can influence and possibly reduce the experience of pain.
Tumor necrosis factor (TNF)-alpha is a messenger substance that promotes inflammatory processes in rheumatic diseases. TNF-alpha inhibitors can block inflammation and are used, among other things, in severe courses of RA. Commercially available biologics for therapies of rheumatic diseases that inhibit the effect of TNF-alpha include adalimumab, infliximab, or golimumab.
Researchers in Erlangen have studied signal transduction in pain. Pressure was deliberately used to induce pain in swollen joints, and then fMRI was used to track where corresponding signals occurred everywhere. This point in time marked “Day Zero”. After only three days of anti-TNF therapy, the responders showed signal reduction and a corresponding change in pain reception in the brain on a repeat fMRI, and there was no change in peripheral inflammation in the joint at that time. The nonresponders did not show such altered responses to pain. This is an indication that anti-TNF-alpha therapy not only inhibits inflammatory processes, but also has an effect on the central nervous system and the perception of pain.
Reduction of Swollen Joint Count by Biologics
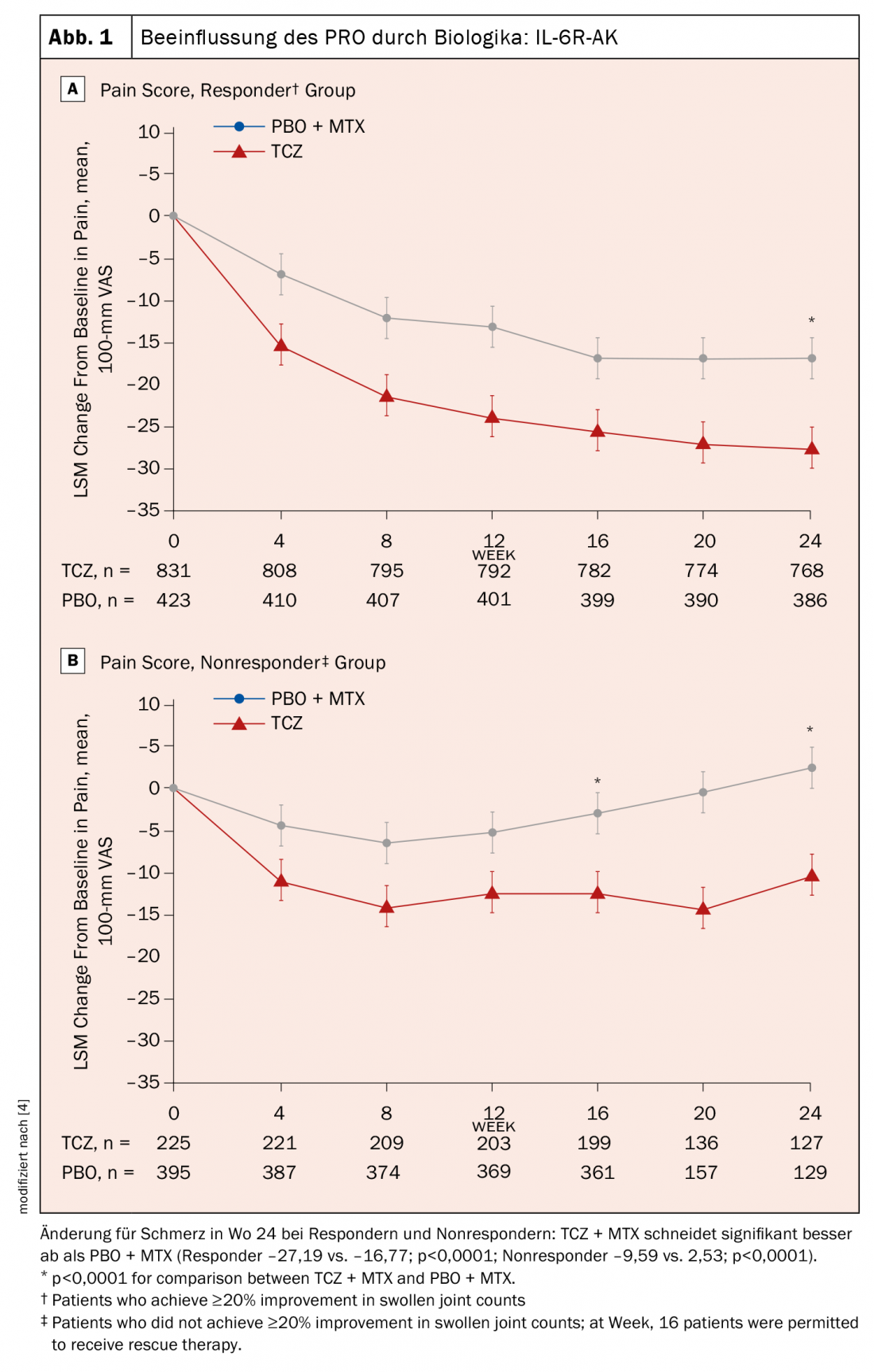
Further evidence of this effect of cytokine therapies comes from an analysis of phase 3 studies of tocilizumab (TCZ) on the impact of biologics on Patient Reported Outcome (PRO): IL-6R-AK. Response to therapy was defined here as a reduction in the number of swollen joints, or Swollen Joint Count (SJC). Comparison between responders and nonresponders, i.e., patients who did not experience at least a 20% improvement in SJC, showed that pain had decreased significantly in responders, especially compared with the placebo group, after 24 weeks. Interestingly, pain was also reduced in the nonresponders compared with the placebo group. Again, interleukin-6 blockade was able to affect pain without affecting inflammation (Fig. 1A+B) [4].
Rapid Pain Reduction by JAK Inhibitors
For JAK inhibitors, the effect on pain, and in particular “Worst Joint Pain” the most severe pain, has also been further investigated using phase 3 studies. With baricitinib, there was sometimes even an improvement in pain as early as day three. From day 17, baricitinib was shown to reduce pain more than adalimumab [5].
In the case of tofacitinib, it was also shown, based on phase 3 studies and with regard to patients with psoriatic arthritis, that only 25% of the pain reduction produced by tofacitinib was due to a decrease in inflammation, C-reactive protein (CRP) levels, and SJC (indirect effect). 74.1% of the pain reduction was shown to be a direct effect on pain, independent of anti-inflammation.
Take-Home Messages
- Pain remains a major problem of patients with rheumatic diseases.
- Use conventional pain medications as needed – opioids only with appropriate treatment plan.
- Biologics show central influence on pain experience.
- Also by JAK inhibitors often rapid improvement of acute pain triggered by inflammation (further anti-nociceptive effects?).
Source: Rheumatologic Pain Management – What’s Beyond Opioids? StreamedUp! Rheumatism Live: Pain; 05/24/2022.
Literature:
- Whittle SL, Richards BL, Husni E, et al: Intervention opioid therapy for treating rheumatoid arthritis pain. Cochrane Database Syst Rev 2011; doi: 10.1002/14651858.CD003113.pub3.
- Häuser W, Bock F, Engeser P, et al: Long-Term Opioid Use in Non-Cancer Pain. Dtsch Ärztebl Int 2014; 111(43): 732-740; doi: 10.3238/arztebl.2014.0732.
- Lee YC, Napadow V, Loggia ML: Functional Connectivity: Dissecting the Relationship Between the Brain and “Pain Centralization” in Rheumatoid Arthritis. Arthritis Rheumatol 2018; 70(7): 977-980; doi: 10.1002/art.40454.
- Sebba A, Han J, Mohan SV, et al: Pain and Other Patient-Reported Outcomes in Patients with Rheumatoid Arthritis Who Did or Did Not Achieve Treatment Response Based on Improvement in Swollen Joints in Tocilizumab Clinical Trials. ACR Convergence 2020, Abstract No.1237.
- Keystone EC, Taylor PC, Tanaka Y, et al: Patient-reported outcomes from a phase 3 study of baricitinib versus placebo or adalimumab in rheumatoid arthritis: secondary analyses from the RA-BEAM study. Ann Rheum Dis 2017; 76(11): 1853-1861; doi: 10.1136/annrheumdis-2017-211259.
InFo PAIN & GERIATry 2022; 4(1-2): 22-23.











