In modern pathogenesis and treatment concepts, psychosocial dimensions are also included in the management of chronic dermatoses. Psychosocial stress is one of the trigger factors of atopic dermatitis and can exacerbate symptoms. This can result in an itch-scratch cycle with negative consequences at various levels. Multimodal therapy including consistent basic care and interdisciplinary coping strategies can bring about relief from symptoms.
Skin diseases have increased sharply in recent years. About 13% of children and 2-3% of adults suffer from atopic dermatitis [1]. It has been repeatedly empirically demonstrated that chronically distressing skin symptoms correlate with psychopathological states such as depressivity, anxiety, dysfunctional coping behaviors, dissociation, withdrawal, and helplessness [2]. “Many primary mental illnesses are stress-related diseases. Persistent dystress also affects the skin via immune modulators,” says Manfred Buchberger, MD, specialist in psychiatry and psychotherapy, Praxisgemeinschaft Binningen [1]. It is a complex structure with multiple interactions. Scientific evidence shows that psychological stress alters the skin’s ability to respond to environmental stimuli via neuroendocrine and immunological changes.
Psyche and skin – a bidirectional interaction
“Skin and soul are closely intertwined and strongly influence each other,” explains Dr. Buchberger [1]. A connection between psychosocial situation and skin condition also appears in colloquial language: phrases such as ‘it doesn’t itch me’ or ‘something gets under the skin’ indicate concrete neuroendocrine activation and interactions with the immune system of the skin: for example, blood flow regulation by adrenergic nerves or sensory stimulation with subsequent neuropeptide release and mast cell activation, i.e. neuroimmunoendocrinologically mediated inflammation [2]. Important pathogenetic factors of atopic dermatitis include genetically determined type 2 inflammation, a weakened skin barrier, and microbial dysbiosis. Psychosocial stress is one of the provoking factors that can contribute to an aggravation of the symptoms and thus increase the stress level. In the mechanisms of this bidirectional interaction, it plays an important role that the skin has a direct connection with the central structures of the neuroendocrine stress response through its dense innervation and a network of blood vessels [2].
Psychosocial stress and the “itch-scratch” circuit
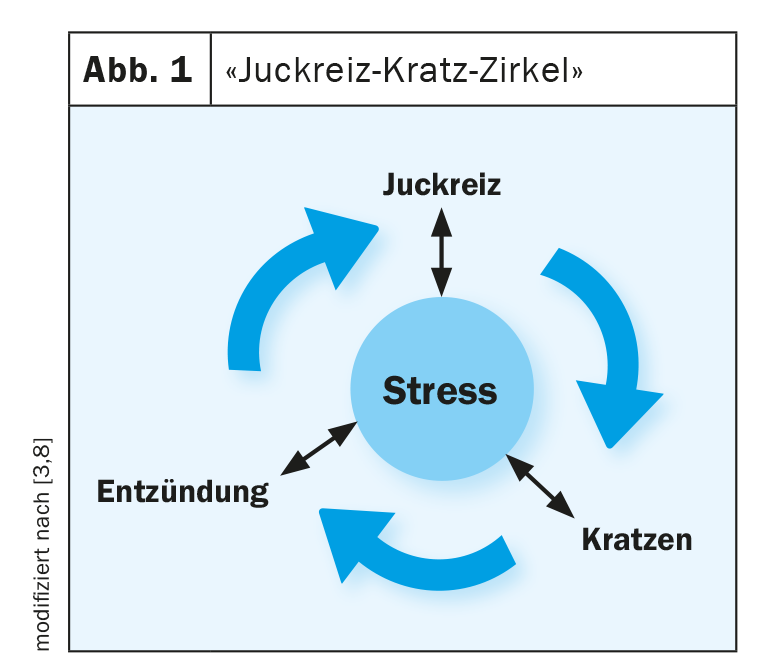
Atopic dermatitis manifests itself in 80% of cases already in the 1st year of life, the first skin symptoms usually appear from the third month of life, reports Jan Izakovic, MD, specialist in dermatology and venereology, Dermatologische Praxis Basel [3]. “Dry skin, itching, rash, and the episodic chronic course are the main characteristics of atopic dermatitis,” said Dr. Izakovic [3]. Trigger factors include skin irritants in cosmetics, weather exposure, perspiration and psychosocial stress, the expert said. Itching is a leading symptom of atopic dermatitis and is very uncomfortable for sufferers. Itchy skin robs sleep, reduces concentration and performance, and can significantly affect the overall quality of life. Scratching as a reaction leads to an aggravation of the symptoms; in this context, one also speaks of the itch-scratch circle (Fig. 1) [2]. As a result, skin damage worsens and more itch-promoting cytokines are released, reinforcing the inflammatory cascade. There can be sleep disturbances and an increased susceptibility to stress, which in turn leads to an escalation of the itch-scratch cycle. “The goal of therapy is to break this vicious cycle,” said Dr. Izakovic [3].
Strengthen skin barrier through basic care – from the inside and outside
If the skin barrier is disturbed, the skin becomes dry and cracked and thus susceptible to inflammation [4]. A defect in the barrier function of the skin is a characteristic of atopic dermatitis and is further exacerbated by a cutaneous inflammatory response [5,14]. Restoration of impaired barrier function is central in the therapeutic management of atopic dermatitis. Therefore, consistent basic therapy in all stages and severities of atopic dermatitis is recommended in the guidelines [6,7]. An important component of this is emollients – externals which are free of active ingredients and have refatting properties. In addition to care products applied to the skin from the outside, however, an adequate supply of nutrients from the inside can also help to protect the skin barrier. Polyunsaturated fatty acids such as γ-linolenic acid (GLA) play an important role in this regard [8]. It has been observed that lowered concentrations of GLA in the blood can lead to itchy eczema [9]. By taking high doses of γ-linolenic acid-containing evening primrose oil, this deficiency can be compensated. In Switzerland, the evening primrose seed oil Epogam® is available for the therapy of atopic dermatitis, which contains the active ingredient γ-linolenic acid. The effect in long-term use is anti-inflammatory and anti-pruritic, at the same time reducing skin dryness [10]. The onset of action begins after 4-8 weeks of daily intake. As a 2014 study by Simon et al. shows, especially those patients in whom the γ-linolenic acid level in the blood increases significantly can benefit [11]. Thus, the decrease in SCORAD correlated with the extent of the increase in γ-linolenic acid levels. Epogam® capsules are approved for use by health insurers in Switzerland, for adults and children from 1 year of age and are well tolerated in long-term therapy [12,13].
|
Basic care through externally and internally applied nutrients Restoration of impaired barrier function is central to the therapeutic management of atopic dermatitis. To achieve this, consistent basic therapy is required at all stages and levels of severity. Replenishing topical topicals without active ingredients are an important part of this. In addition, supply of nutrients from the inside can also contribute to the protection of the skin barrier. γ-Linolenic acid is a polyunsaturated fatty acid, which provides the skin with important nutrients [4]. With long-term use, a skin dryness reducing and antipruritic effect can be obtained in children and adults with atopic dermatitis [10]. |
Patient reduction as an important interdisciplinary therapy pillar
In the WHO bio-psychosocial model, health and disease are understood as the result of the interplay of physiological, psychological and social processes [15]. The extent of impairment is based on the ICF classification of functioning, disability and health [15]. Patient education is an important component of multidimensional approaches to the treatment of chronic recurrent dermatoses. A chronic skin disease is often associated with far-reaching consequences for patients in terms of quality of life, therapy requirements and dealing with the disease in everyday professional and private life. Stigmatization is also a psychological stress factor, which often plays a role in chronic inflammatory dermatoses. Patient education sessions focus on developing strategies for dealing with the impairments caused by the chronic skin disease. In the training sessions, the patient is given a holistic approach and assistance in coping with the disease and its impact on the overall life situation. Improving coping strategies is a prerequisite for long-term improvements in disease progression. For atopic dermatitis, standardized training programs are offered for affected individuals of all ages and parent training for affected young children. By promoting disease management skills, medium- to longer-term goals such as healing or reduction of skin lesions, reduction of distressing itching, and restoration and stabilization of the skin’s protective barrier function should be achieved. The training program for children, adolescents and parents in atopic dermatitis is evidence-based effective (evidence level A according to Cochrane analysis) [15].
Source: Zeller Medical AG
Literature:
- Buchberger M: I’m itching for that! The skin – mirror of the soul? Digital advanced training, Zeller Medical AG, Feb. 11, 2021.
- Peters EMJ: Stressed skin? – Current status of molecular psychosomatic correlations and their contribution to causes and consequences of dermatological diseases. JDDG 2015, DOI: 10.1111/ddg.12957
- Izakovic J: Why am I itching? The skin – mirror of the soul? Digital advanced training, Zeller Medical AG, 11.02.2021
- DAZ: Drugs and Therapy. Gamma-linolenic acid for a strong skin barrier Deutsche Apotheker Zeitung 2005, No. 34, p. 48, 21.08.2005 www.deutsche-apotheker-zeitung.de, (last accessed 12.02.2021)
- Volz T, et al: On the role of the innate immune system in atopic dermatitis. Dermatologist 2015; 66: 90-95.
- Eichenfield LF, et al: Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol 2014; 71: 116-132.
- Werfel T, et al: S2k guideline neurodermatitis (atopic eczema, atopic dermatitis) – abridged version. J Dtsch Dermatol Ges 2016; 14: 92-106.
- Schnopp C: Neurodermatitis training: How can it support sufferers? Allergy Patient Forum, Jan. 27, 2018, www.allergieinformationsdienst.de
- Rupf R: Evening primrose oil in children – a hope for atopic dermatitis. Swiss Medical Society for Phytotherapy 2001, www.smgp.ch, (last accessed Feb. 12, 2021).
- Junghans V: Phytotherapy in the treatment of atopic dermatitis. Dr. Volker Junghans Thesis in the framework of the SMGP skill program phytotherapy, www.smgp.ch (last retrieval 12.02.2021)
- Simon D, et al: Gamma-linolenic acid levels correlate with clinical efficacy of evening primerose oil in patients with atopic dermatitis. Adv Ther 2014; 31(2): 180-188.
- HMPC Assessment report on Oenothera blennis L., Oenothera lamarckiana L., oleum 2018, www.ema.europa.eu (last accessed Feb. 12, 2021).
- Technical information: epogam® 1000 vegicaps soft®, www.swissmedicinfo.ch, (last accessed 12.02.2021)
- Biedermann T, et al: Regulation of T Cell Immunity in Atopic Dermatitis by Microbes: The Yin and Yang of Cutaneous Inflammation. Front Immunol 2015; 6: 353.
- Interdisciplinary S1 guideline: inpatient dermatological rehabilitation. Bayerisches Ärzteblatt 3/2017. www.bayerisches-aerzteblatt.de, (last accessed Feb. 12, 2021)
DERMATOLOGY PRACTICE 2021; 31(1): 28-30
DERMATOLOGY PRACTICE 2021; 31(6): 44-46