A meniscal lesion is a degenerative or traumatic injury to the medial or lateral meniscus. A typical symptom is sudden pain that intensifies when walking. If a meniscal rupture is suspected, imaging techniques are used in addition to checking meniscal signs. Radiological diagnosis can exclude a bony injury. MRI examinations provide excellent visualization of joint structures. Arthroscopy, on the other hand, is nowadays mainly performed for therapeutic purposes.
In the article on cartilage changes of the knee joint, the causes and pathohistological processes of cartilaginous degeneration have already been named. These also apply to degenerative meniscal damage. In principle, meniscus damage can also be the result of traumatic joint impact with previously intact cartilage and meniscus conditions.
For many years, conventional radiographs were the standard of noninvasive joint diagnosis, extended by conventional tomography in the early 1920s [6]. A further improvement in joint diagnostics was achieved after the development of contrast media through arthrography and arthrotomography. Since about 1930, these methods were routinely used. Computed tomography allowed significantly improved visualization of bony and calcified structures, and in combination with intra-articular contrast, also allowed assessment of cartilage surfaces and the course of ligaments.
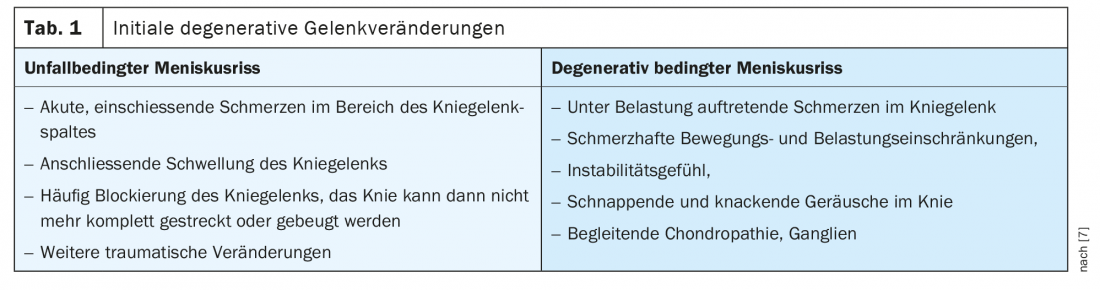
However, magnetic resonance imaging was the first breakthrough in non-invasive imaging of all joint-forming structures. Indirect MR arthrography represented a further improvement in the assessment of cartilage and meniscal structures over the years, but was associated with intravenous contrast agent application and increased examination time [4]. The continuous development of hardware and software in magnetic resonance imaging diagnostics today allows a diagnostically very good and reliable statement about the inner joint structures without any invasiveness. The symptoms of a meniscal tear [7] can vary and depend on the type of origin (Table 1).
The history and clinical examination are indicative and may lead to a tentative diagnosis. Over decades, certain criteria of physical examination have proven themselves [2], especially the positive Steinmann signs. However, meniscal tears are not always the sole cause of symptoms; in particular, several degenerative changes play a role in the complexity of symptoms in older patients (cartilage damage, resulting spongiosa edema of the bony stress zones, synovitis, bursitis, hypertrophic plicae, ligamentous damage).
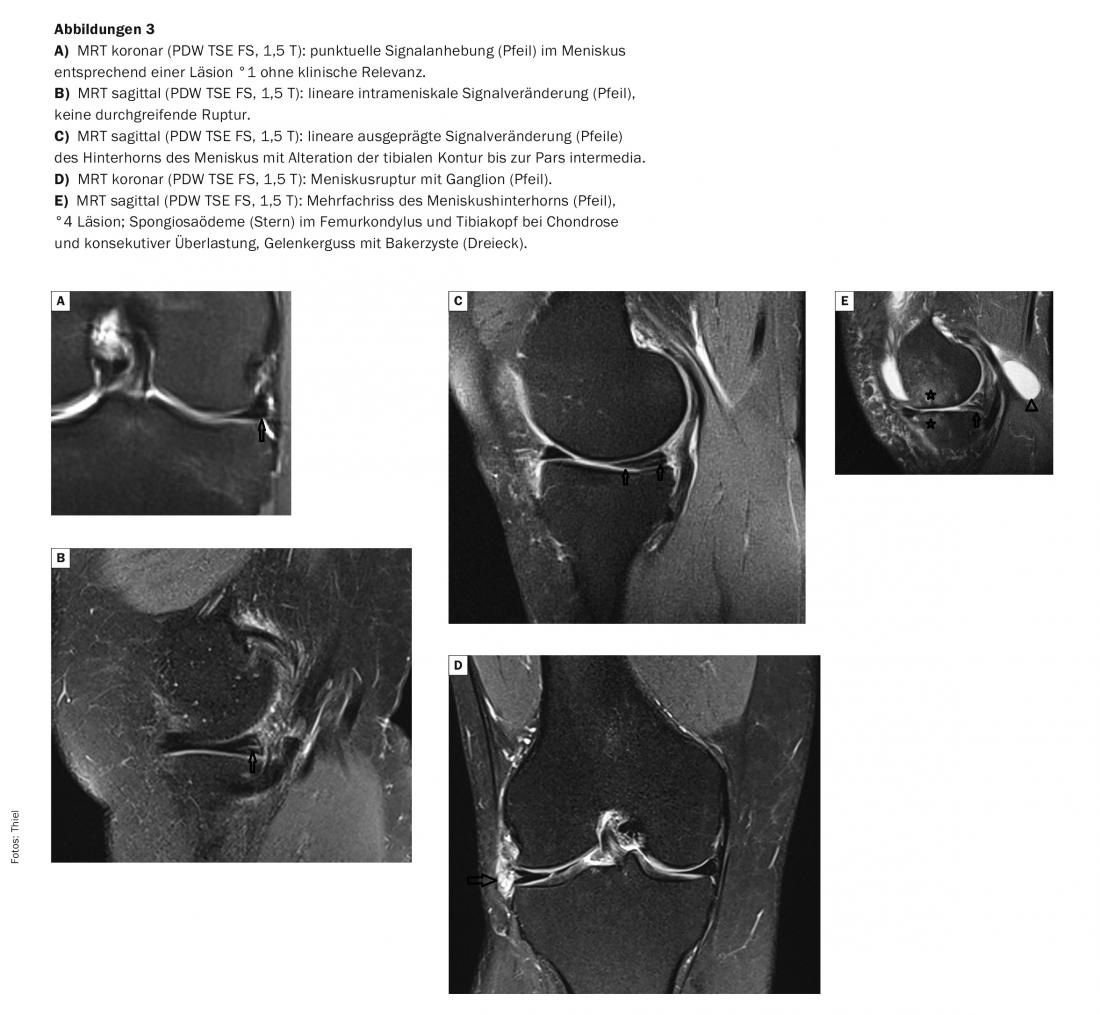
In MRI, the diagnostic criteria of meniscal damage classification have been proven for about 25 years [5] and are listed in Table 2. The method is the imaging modality of choice and has a decisive influence on further therapy planning [3]. In recent years, there has been a paradigm shift toward conservative measures in the treatment of meniscal damage [1]. The declared aim is to maintain or establish mechanically stable joint conditions and load-bearing capacity.
Radiographs have no diagnostic value in the direct detection of a meniscal tear, but can visualize the extent of bony changes in the context of osteoarthritis. Also, if there is significant calcification of the cartilage or meniscal structures, chronic damage must be assumed (Fig. 1).

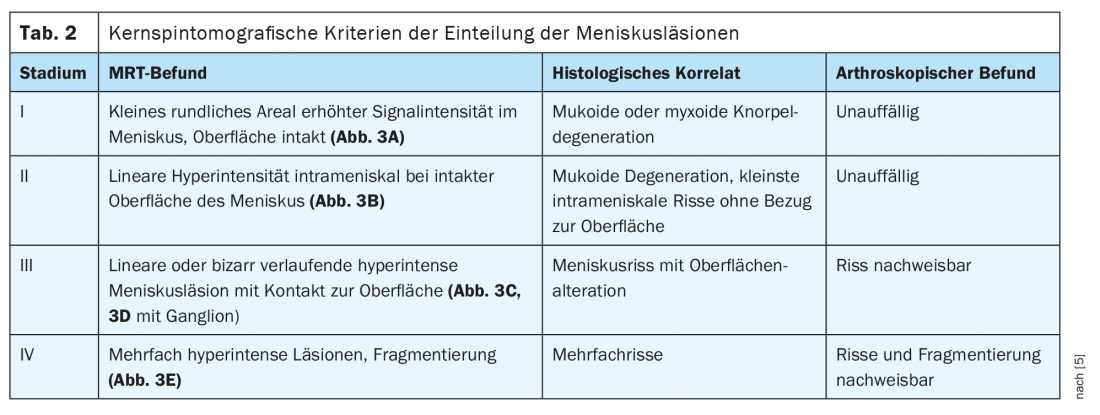
Computer tomographic examinations also play no role in the diagnosis of cartilage and meniscus structures (Fig. 2). The importance in the detection of small calcified or bone-dense corpora libera remains unchanged, as well as in fracture diagnostics.
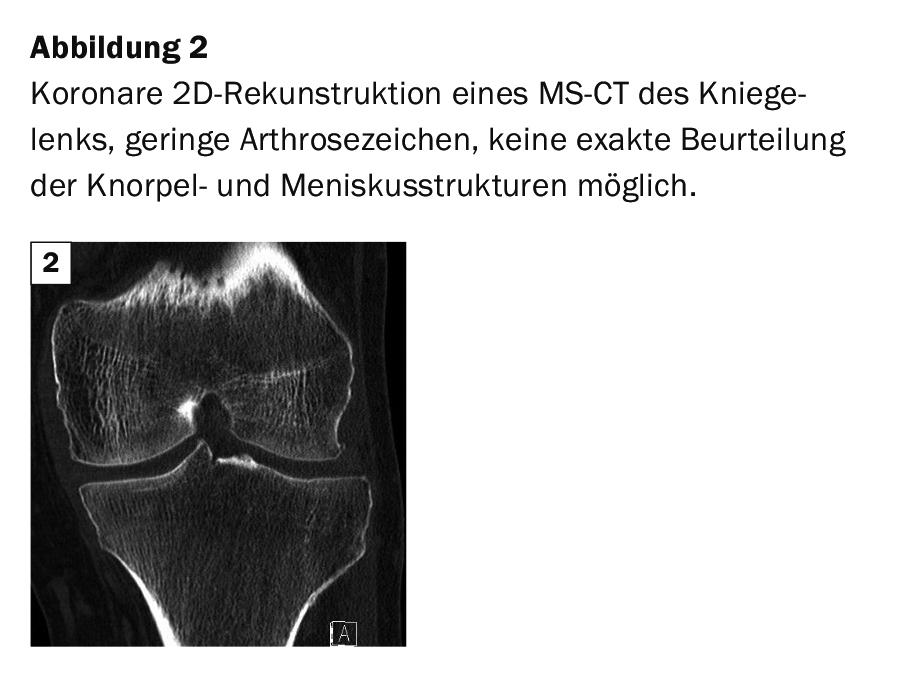
Magnetic resonance imaging provides excellent visualization of all joint structures. Indirect MR arthrography, used for many years in knee joint diagnostics as a noninvasive method, has become less important. Meniscal damage can be reliably demonstrated on native MR examinations (Fig. 3A through E) .
Case studies
In case study 1, a 78-year-old patient had a painful limitation of movement -with known gonarthrosis. Case 2 documents minor osteoarthritis on MS-CT, and the cartilage and meniscal structures cannot be decisively assessed. The examples 3 show different stages of meniscal damage without adequate trauma. Except for Example 3A with meniscus lesion °1, pain persisted, sometimes with limited weight-bearing capacity and reduced mobility (especially in case 3E).
Take-Home Messages
- The knee joint is one of the most frequently affected joints in degenerative changes.
- MRI as an imaging technique is the noninvasive method of choice to comprehensively visualize the changes in the interior of the joint.
- MR tomography quantifies the different stages of meniscal degeneration and ruptures.
- X-ray examination and computed tomography provide specific supplementary information (e.g., intra-articular calcifications, corpora libera), but cannot verify the exact extent of meniscal damage.
Literature:
- Beaufils P, Pujol N: Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res 2017; 103(85): S227-244.
- Bronstein RD, Schaffer JC: Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions. Am Acad Orthop Surg 2017; 25(5): 365-374.
- Nguyen JC, De Smet AA, Graf BK, Rosas HG. MR imaging-based diagnosis and classification of meniscal tear. Radiographics 2014; 34(4): 981-999.
- Thiel HJ: Indirect MR arthrography. mta 13, 1998: 644-648.
- Thiel HJ: Cross-sectional diagnosis of the joints. Part III: Computer and magnetic resonance imaging diagnosis of degenerative changes of the knee joint. mta Spectrum 7, 2001: 308-310.
- Thiel HJ: Cross-sectional diagnosis of joints (I). mta Spectrum 4, 2001: 159-161.
- www.endoprosthetics-guide.com/knie/meniskusriss
HAUSARZT PRAXIS 2021; 16(2): 39-40











