Lactose intolerance is the most common enzyme deficiency in humans. Fructose intolerance is also on the rise due to increased fructose content in the diet. Therapy for both forms is often a change in diet.
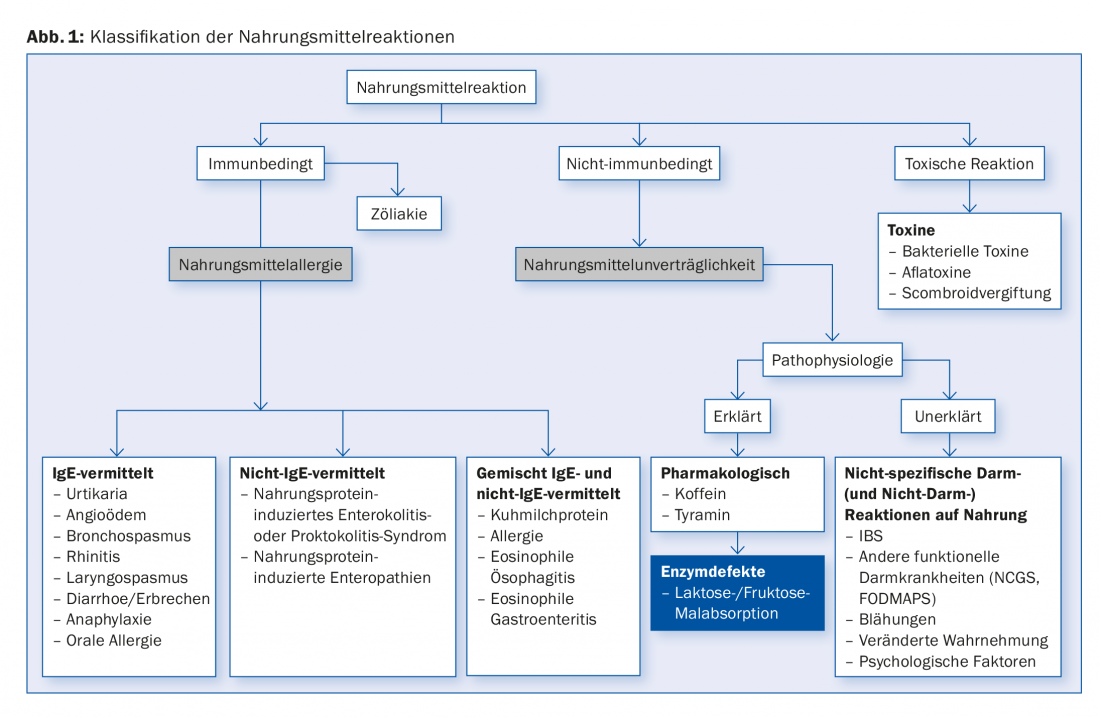
Patients often describe reactions to food during consultations. A distinction can be made between immune-related (food allergies), non-immune (food intolerances) and toxic reactions ( Fig. 1). It is assumed that 1-20% of the population suffer from food intolerance. The following article will focus on the subgroup of enzyme defects in food intolerances. This includes in particular lactose and fructose malabsorption.
Lactose intolerance – pathophysiology and epidemiology
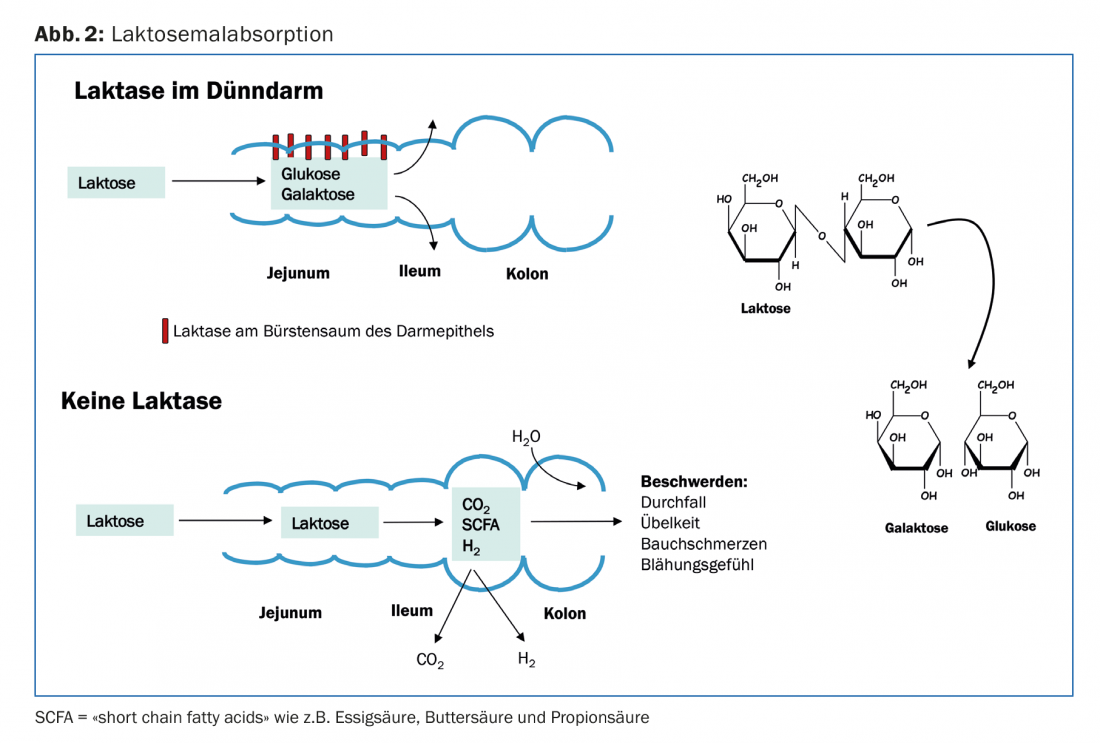
Lactose intolerance is the occurrence of numerous symptoms of various kinds after ingestion of food containing lactose. In particular, the enzyme lactase (strictly speaking, it is lactase-phlorizin hydrolase) plays an important role. This enzyme cleaves the dietary disaccharide β-galactose-1,4-glucose (lactose) in the mucosal brush border cells of the jejunum into the components D-galactose and D-glucose. These two monosaccharides are then absorbed in the small intestine, whereas lactose cannot be absorbed there. If the lactose molecule reaches the large intestine, it is fermented there by colon bacteria. The resulting fermentation products are hydrogen, carbon dioxide and short-chain fatty acids (acetic acid, butyric acid and propionic acid) (Fig. 2) . After consumption of lactose-containing foods, lactase deficiency results mainly in gastrointestinal symptoms such as flatulence and bloating, abdominal pain and osmotic diarrhea. However, symptoms may be absent, or there may be nonspecific symptoms such as headache, dizziness, depressed mood, chronic fatigue, and difficulty concentrating.
The intolerance to lactose is based on various causes. Very often hypolactasia is found in lactose intolerant patients. This lactase deficiency is the most common enzyme defect worldwide. In more than half of the world’s population, there is evidence of a slow loss of lactase function after weaning. Current prevalence figures for Switzerland are unfortunately not available; however, it is estimated that 15-25% of the total population in Europe suffers from lactose intolerance. Prevalence rates are much lower in northern Europe (2%) and much higher in the Mediterranean region (25-75%). Among Africans and Asians, almost 100% are affected by lactose intolerance [1,2].
Subdivision and genetics of lactose intolerance
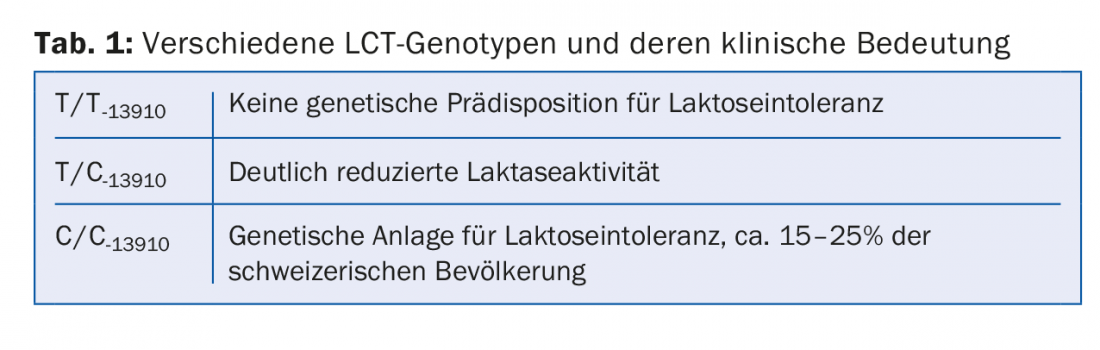
In lactase deficiency, a primary form is distinguished from a secondary form. In the primary form, a distinction is again made between the common adult form, lactase deficiency in premature births (lactase is not produced until the 33rd week of pregnancy) and the rare congenital lactase deficiency. Lactase deficiency of the primary adult form is understood to be a genetic predisposition in which there is a decreasing effect of the lactose-splitting enzyme lactase in the course of life. Here, enzyme activity decreases continuously after infancy and then reaches definitive expression in adolescence or early adulthood. However, previous studies have not been able to provide precise information on when hypolactasia initially becomes noticeable. The gene responsible for the activity of lactase is called LCT-1 gene. This genetic form of lactose intolerance is called primary lactose intolerance (or primary genetic adult hypolactasia). A single nucleotide polymorphism with exchange of thymidine for cytosine at position -13910 plays a crucial role (Table 1).
Primary lactose intolerance is distinguished from secondary lactose intolerance (also lactose maldigestion). This refers to the inability of the small intestine to break down lactose correctly, although the affected patient has the genetic prerequisites for correct lactase production. The cause here is damage to the brush border epithelium in the jejunum. Typical causes of secondary lactose intolerance are gastrointestinal diseases such as celiac disease, infectious gastroenteritis (viruses, giardiasis, enteropathogenic E. coli), Crohn’s disease with jejunal involvement, but also drug side effects, e.g. from antibiotics or immunosuppressants. Treatment of the underlying disease and thus restoration of normal function of the intestinal mucosa lead to tolerance of foods containing lactose.
Diagnosis of lactose intolerance
Oral lactose tolerance test: After drinking 50 g of lactose (equivalent to one liter of milk), blood glucose levels are measured after 60 and 120 minutes. With sufficient lactase activity with cleavage into glucose and galactose, there should be a blood glucose rise of at least 20 mg/dl above basal. This test is relatively complex and not very specific and sensitive.
H2 breath test with lactose: After lactose is ingested, end-expiratory H2 concentration is measured after 30, 60, 90, and 120 minutes (occasionally up to 240 minutes). The test is positive if there is an increase of >20 ppm (pixels per minute) above basal in end-expiratory breath. False-positive values may occur if patients have a bacterial overgrowth of the small intestine or oral cavity. For example, smoking and chewing gum before the examination can lead to increased values. False-negative values, on the other hand, are present when methane-producing bacteria occur in the intestine. These bacteria rapidly recycle the hydrogen produced, so that H2 is only exhaled in low quantities.
Lactase activity in small intestinal biopsies: Lactase activity can be measured in biopsies from the small intestine. Sensitivity and specificity are considered to be rather low.
Genetic test: As mentioned above, PCR testing can be used to measure the polymorphism of the LCT gene. The sensitivity is similar to that of the H2 breath test. The test is not covered by health insurance in Switzerland and the patient should be informed of the costs incurred of approximately CHF 180.
Fructose intolerance
In the small intestine, fructose is absorbed into the body via a transport protein (GLUT5). This transport protein represents a limiting factor for the absorption capacity of fructose from food. Similar to lactose intolerance, fructose enters the colon and is fermented by intestinal bacteria, which can lead to bloating, abdominal pain, and osmotic diarrhea in half of patients [3]. Additional symptoms may include depression and occasionally a folic acid or zinc deficiency can be detected. There are also no reliable figures for fructose malabsorption (intolerance to fruit sugar) in Switzerland. It is estimated that 25-30% of the population suffer from fructose intolerance [4]. However, these data are controversial. Several possible factors are mentioned as to why there is an increase in this disease. The intake of fructose and sugar alcohol has increased many times over in recent decades. This is related to a significant increase in fructose-rich foods and also to the general current recommendation that people should eat a diet rich in fruit. Current gastroenterology literature discusses fructose as an eating defect. Our diet is so rich in fructose and sugar substances and so poor in fats that one can almost speak of a physiological reaction (“fructose overload”) when there is an excess of fructose [5,6]. Diagnosis is made by breath test after oral exposure to 20-50 g fructose.
Therapy
In the case of the sugar utilization disorders lactose intolerance and fructose intolerance, the daily food selection, but also the amount of food in particular, have a significant influence on tolerance in humans. It is important for those affected to know that they are not suffering from a potentially life-threatening condition and, for example, in the case of lactose intolerance, they can often tolerate dairy products with relatively little lactose (due to the addition of lactase-producing bacteria) such as cheese and yogurts. Education about physiological limitations of the digestive tract is the first therapeutic goal in affected patients. Qualified nutritional therapy plays a decisive role in this. Important recommendations such as “fruits and vegetables five times a day” should be followed, but patients with intolerances should also be made aware that the focus is more on getting enough vegetables and not so much on getting enough fruit. Vegetables are tolerated much better than fruit by patients with fructose intolerance. In addition to fructose-containing fruits (especially local fruits), juices, smoothies, and fructose syrup are a source of excessive fructose consumption. Patients affected by lactose intolerance can also take the enzyme lactase in the form of chewable tablets. It should be taken 30 minutes before eating meals containing lactose. It should also be noted that a dairy-free diet results in significantly reduced calcium intake and care should be taken to ensure sufficient calcium intake.
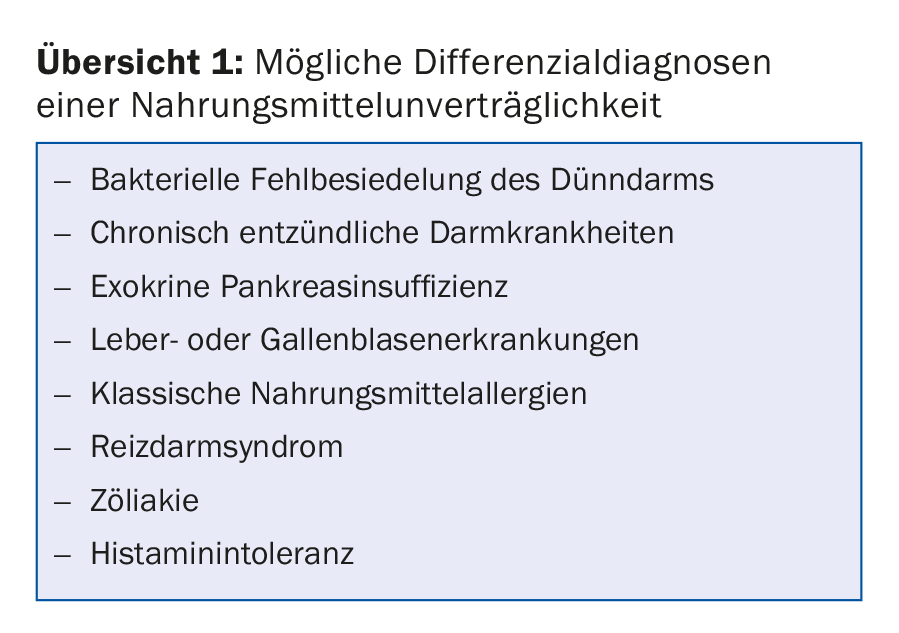
Differential diagnostics
If symptoms persist in patients despite a period of abstinence without dietary error, the period should not be artificially prolonged. In no case should the diet then be even stricter, in the sense of “even more sugar-free”. A rapid expansion of the various nutritional components has proven effective here. This is especially true for patients with fructose malabsorption. Further restriction in the sense of a fructose-free diet will – contrary to the assumption of many patients – not bring long-term improvement. In children, persistent symptoms are more likely to be due to dietary errors that subside after dietary adjustments and attention to macronutrients (!) and dietary control accompanied by a dietary and symptom protocol. Freedom from symptoms after maternity leave is not always given in adults. If the symptoms remain the same, the phase of testing should still follow in order to achieve a higher intake of fructose and sorbitol and a significant expansion of the food selection. If there is no significant decrease in symptoms after strict abstinence and consideration of gastroenterological recommendations, other diseases should be considered. These are summarized in overview 1.
Literature:
- Terjung B, Lammert F: Lactose intolerance: new aspects of an old problem. Dtsch Med Wochenschr 2007; 132: 271-275.
- Wermuth J, et al: Lactose intolerance. Schweiz Med Forum 2008; 8: 746-750.
- Ledochowski M, Eisenmann A: Fructose malabsorption. ZKM 2010; 3: 17-21.
- Latulippe ME, Skoog SM: Fructose malabsorption an intolerance: effects of fructose with and without simultaneous glucose ingestion. Crit Rev Food Sci Nutr 2011; 51(7): 583-592.
- Ledochowski M, et al: Fructose- and sorbitol-reduced diet improves mood and gastrointestinal disturbances in fructose malabsorbers. Scand J Gastroenterol 2000; 35(10): 1048-1052.
- Schäfer C, et al: Fructose malabsorption: Statement of the Study Group for Food Allergy of the German Society for Allergology and Clinical Immunology AG Nahrungsmittelallergie in der Deutschen Gesellschaft für Allergologie und klinische Immunologie (DGAKI). Allergo J 2010; 19: 66-69.
HAUSARZT PRAXIS 2018; 13(7): 30-33