Lipedema is a painful, disproportionate increase in fat in women; on legs and arms, as well as hips and buttocks. Lipedema has been officially classified as a disease in the ICD catalog for several years. The diagnosis is made on the basis of clinical criteria. Liposuction is currently covered in Switzerland if the pain associated with lipedema does not respond adequately to intensive conservative therapy (compression and manual lymphatic drainage) and a recommendation is made by a trusted physician. In addition to surgical and conservative procedures, dietary changes and exercise intensification are among the other pillars of therapy.
Lipedema is a painful, sometimes chronic progressive disease characterized by a fat distribution disorder with often significant disproportion between slender trunk and voluminous extremities. The disease is defined by circumscribed, symmetrically localized subcutaneous adipose tissue proliferation on the lower and upper extremities, as well as the hips and buttocks. Characteristic are increased pain on touch and pressure, spontaneous pain and a feeling of heaviness in the affected areas of the body. The “edema” contained in the name is not present in the sense of the medical meaning (=water accumulation in the tissue).
Diagnostic classification
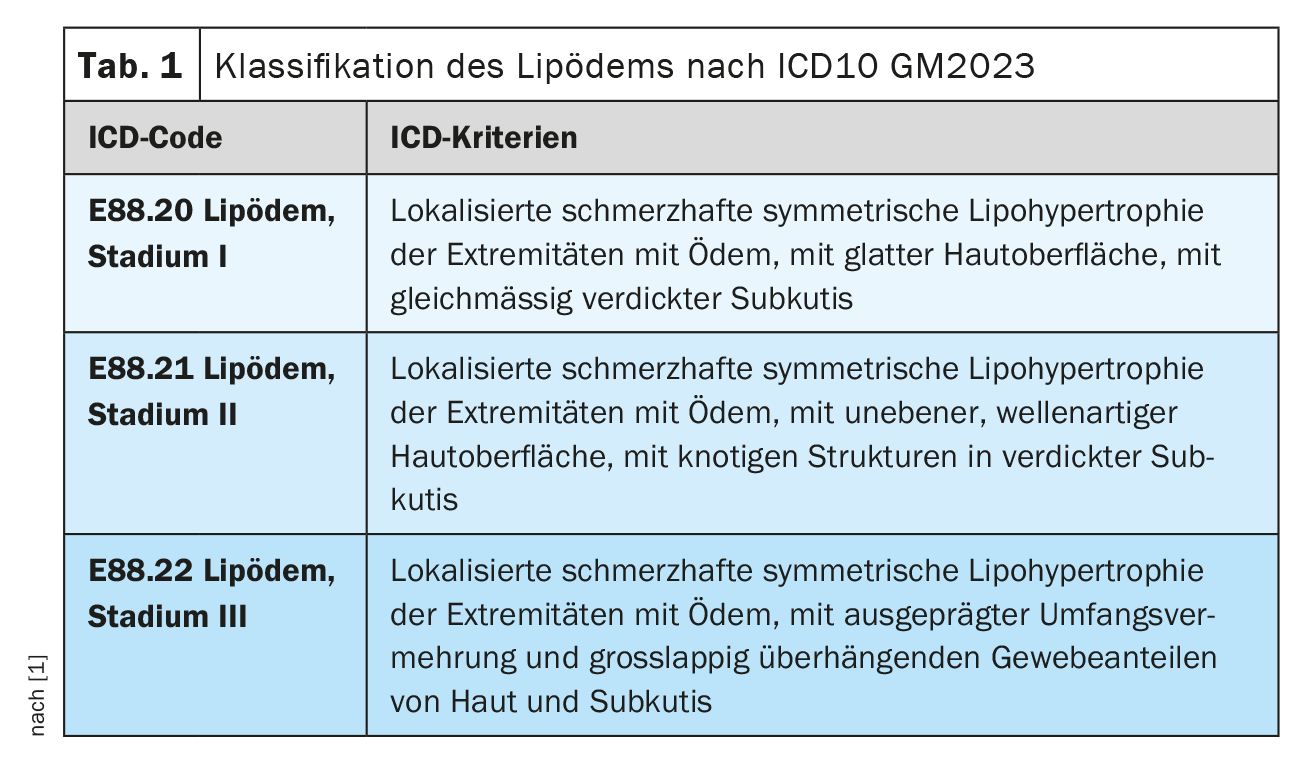
Since 2017, the disease lipedema is internationally statistically classified in the ICD catalog (International Classification of Diseases) . In the ICD10 catalog – German Modification, the disease lipedema is listed stage-dependent (stage I – III) ( ICD10-GM2023: E88.20 – E88.22) (Table 1) [1]. The following ICD11 catalog for mortality and morbidity statistics (MMS) has already been approved by the WHA72 (World Health Assembly) in May 2019. adopted. This ICD catalog in its 11th revision came into force on January 1, 2022 with a five-year transition period, and is in principle applicable in a first German-language draft version (ICD11: EF02.2). The current, direct German translation of the definition from English: “Lipedema is characterized by a non-push-in diffuse ‘fatty’ swelling, usually confined to the legs, thighs, hips, and upper arms. It can be confused with lymphedema. Lipedema can also occur on the scalp.” A clear misconception must be made about the inclusion of the scalp (Engl.: scalp) can be assumed. A staging was not used at all.
The disease affects almost exclusively women and occurs during phases of hormonal changes, such as puberty, during and after pregnancy, or more rarely during menopause. It is assumed that about 5-10% of Swiss women suffer from lipedema. Unfortunately, valid epidemiological data from larger studies are not yet available. Familial clustering is observed in about 60% of cases. Individual case reports of men affected by lipedema are associated with excessive hormonal imbalances. The etiology of the disease is as yet unknown. The pathomechanisms and especially the specific role of hormones or hormone receptors remain unclear, and are subject to research efforts. The increase in subcutaneous adipose tissue is due to hyperplasia and hypertrophy of fat cells in the area of the affected extremities.
The diagnosis of lipedema is made exclusively on the basis of clinical criteria. Anamnesis, inspection and palpation lead to the typical characteristics here:
- Female patient
- Onset of disease in phases of hormonal change (puberty, pregnancy, menopause)
- Disproportionate, symmetrical fat tissue proliferation exclusively on the extremities (excluding hands and feet)
- Leading symptom: pain (pain on touch, pressure and spontaneous pain)
- Feeling of heaviness and tension
A large variety of previously used synonyms for this adipose tissue disorder corresponded more clearly to the key symptom of pain: lipomatosis dolorosa, lipohypertrophia dolorosa, lipohyperplasia dolorosa, adipositas dolorosa, lipalgia, adiposalgia, painful lipedema syndrome, painful columnar leg.
The name Lipedema, chosen in 1940 by the two American first descriptors Edgar V. Allen and Edgar A. Hines, was used to describe the disease.
Lipedema (dt.) has been established continuously and worldwide in the last decades. Even with the recent frequent discussion of the deviation of the name from the general medical meaning of the term edema (retention of water in body tissue), it should be interpreted and retained in lipedema as a misnomer, or swelling of fatty tissue (ancient Greek: οἴδημα, German: Schwellung). The term lipedema is “simple”, and therefore understandable and easily remembered by all professionals confronted with this clinical picture, as well as patients and family members.
Differential diagnostics
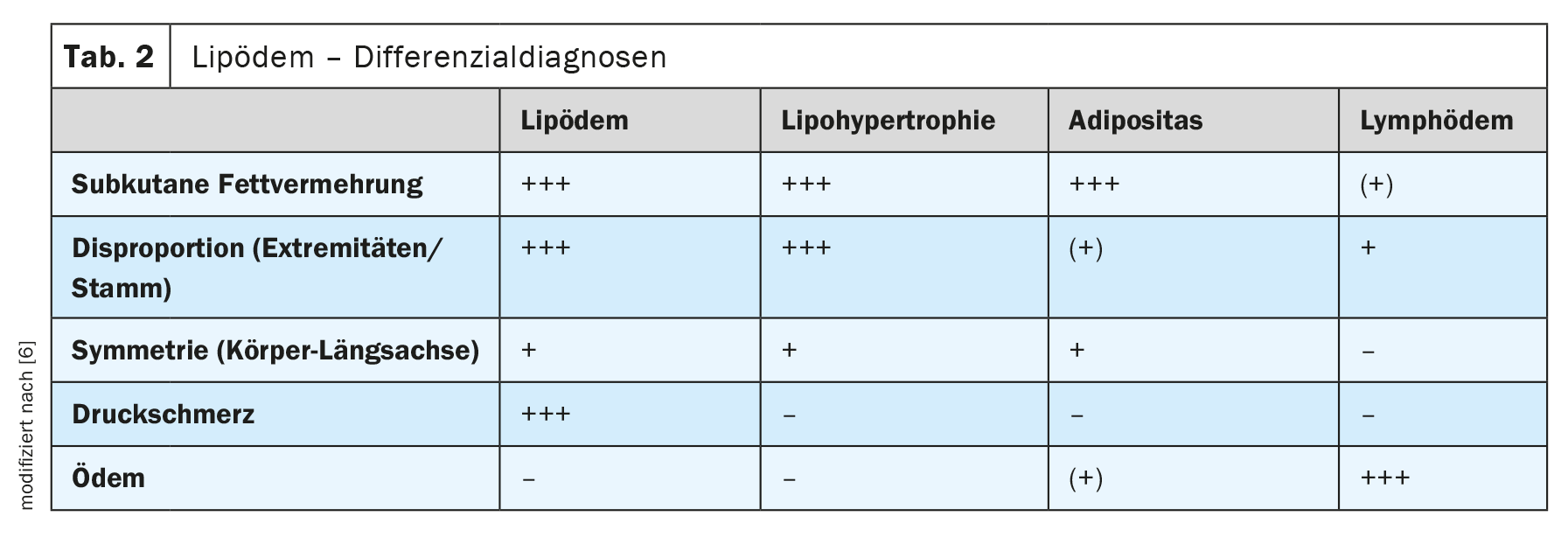
Differentially, all female body shapes and diseases with volume and circumferential increases in the lower and upper extremities must be considered. Lipohypertrophy, obesity and lymphedema are the main differentiators (Table 2). The differentiation of lipedema is based on clinical features: Fat proliferation, disproportion, symmetry, pressure pain and edema.
The leading criterion in lipedema is pain in the affected extremities. Lipedema is by definition not present without pain symptoms. In lipohypertrophy, an aesthetic fat distribution disorder (breeches symptomatology) without any pathological value, edema and pressure pain are absent. Obesity usually does not show disproportion, but associated edema is possible. Pressure pain is not present in subcutaneous tissue obesity. The diagnosis of lymphedema is based on the edema, which is usually asymmetrical.
Other differential diagnoses include phlebedema (edema and signs of chronic venous insufficiency), myxedema in thyroid dysfunction (doughy edema), and the combined disorders: Lipedema with secondary lymphedema, lipedema with concomitant obesity, obesity with secondary edema (obesity-associated edema).
Obese patients with accompanying restless legs syndrome, fibromyalgia syndrome, or other rheumatological or neurological pain disorders are frequently presented to a lipedema center. However, in the case of anamnestic and/or currently absent disproportionate fat proliferation on the lower extremities, lipedema is already excluded.
Progress monitoring
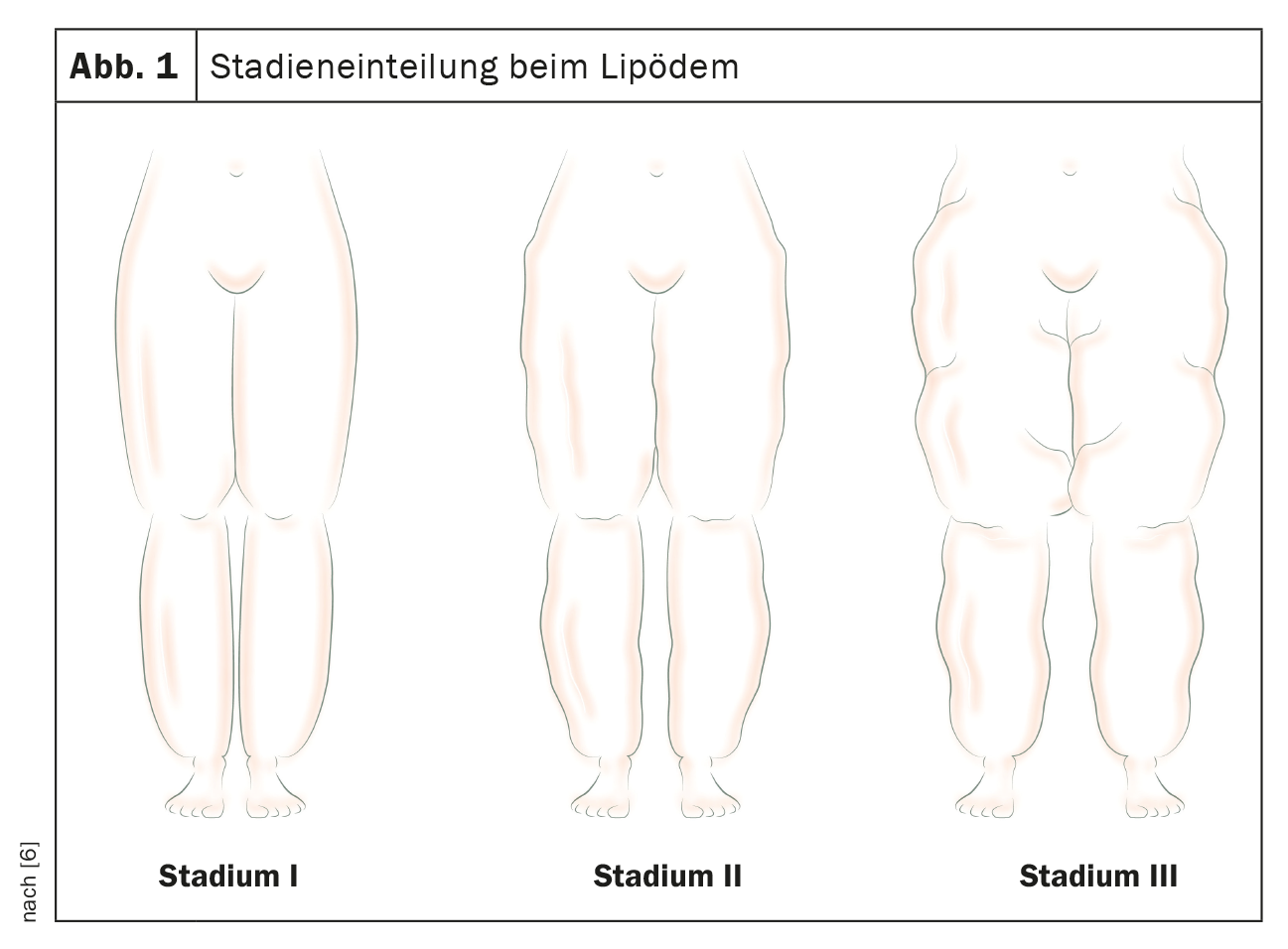
The disease lipedema is partly chronic-progressive, individually very different and unpredictable. The classification is based on the one hand on localization and on the other hand on morphology (stage I-III) (Fig. 1). In the lower extremities, a distinction is made between the whole leg, thigh and lower leg types, and in the upper extremities between the upper arm, whole arm and forearm types. In each case, the order mentioned reflects the frequency of occurrence in a decreasing trend.
The stage can be defined by the following morphological characteristics:
- Stage I: Smooth skin surface with uniformly thickened, homogeneously imposing subcutis
- Stage II: Uneven, predominantly wavy skin surface, nodular structures in thickened subcutaneous area
- Stage III: Pronounced circumferential proliferation with overhanging tissue portions (dewlap formation)
A smooth transition from stage I to stage II or stage III is possible depending on the course of the disease. However, the intensity of symptoms in lipedema does not correlate with the level of the stage. The pain can be much more pronounced in stage I than in advanced stages II or III, which is probably why the staging has been omitted from the new ICD11 classification. As a rule, photographic documentation cannot do justice to the symptoms and suffering of the patients; unfortunately, in many cases the aesthetic component is in the foreground.
In the initial documentation, it is useful to collect the following body values: body weight, body heights, waist and hip circumferences. The body mass index (BMI) can be calculated with this, but is often misleading due to incorrectly high values, with fat masses sometimes present exclusively in the leg area. Also suitable for monitoring the progress of lipedema patients are the determination of the waist-to-height ratio ( WHtR), the waist-to-hip ratio (WHR), and circumference and volume measurements of the extremities (perometry).
Morphologic examinations and functional studies of the lymphatic system are not diagnostic in lipedema and therefore are not required in routine clinical practice. Even the frequently used high-resolution sonography does not show specific criteria in the diagnosis of lipedema.
Treatment of the disease is aimed at symptom relief or freedom (pain, disproportion) and prevention of complications. In advanced stages, the risk of complications increases (maceration, bacterial and mycotic skin infection, erysipelas, lymphedema, foot and leg deformities with valgus-gonarthrosis, gait disturbances with functional effects).
Therapy guidelines
There is no known causal therapy for lipedema. The symptomatically effective measures are combined individually and adapted to the symptoms. In the currently valid version of the German S1 guideline lipedema – AWMF register number: 037-012 (10/2015), the guideline-compliant therapy of the disease consists of a total of four pillars [2].
Conservative therapy: This includes complex physical decongestive therapy (CPD), with an initial decongestive phase by means of bandaging (1-2 weeks) and an immediately subsequent maintenance phase with 1-2× weekly manual lymphatic drainage treatments (MLD) in combination with consistent, daily compression therapy (flat-knitted corsetry class II), exercise therapy and skin care. Apparent intermittent compression (AIK) can be used to support decongestion, but it cannot replace MLD and compression.
Surgical therapy: This is clearly defined as fat tissue reduction by means of liposuction under tumescent local anesthesia (vibration-assisted technique or waterjet technique ) using blunt microcannulas that are gentle on the tissue, and if necessary the subsequent removal of excess skin and tissue flaps by means of plastic surgery measures.
Dietary change: An accompanying dietary change is often useful even in normal-weight patients, but in any case for body weight reduction in cases of concomitant overweight or obesity. Blood glucose and insulin spikes should be avoided, and sufficient breaks between meals should be observed (isoglycemic diet). There is no generally applicable, lipedema-specific dietary recommendation.
Exercise intensification: Increasing physical activity is recommended. Exercises in the water (swimming, aqua-jogging, aqua-aerobics, aqua-cycling, etc.) are particularly effective. In water, joints are relieved of body weight, lymphatic flow is stimulated by water pressure, and more energy is expended by exercising against the resistance of the water. Furthermore, sports exercises with movement on the trampoline are favorable.
In individual cases, psychotherapeutic support can be very useful. Many patients feel stigmatized by the disease, with its disproportionate appearance, and also its conservative therapy, the daily wearing of compression garments and the time-consuming regular lymphatic drainage. In addition, it is not uncommon for doctors and family to have advised weight reduction and more exercise for years, but the underlying clinical picture was not recognized. Patients felt guilty and helpless, unable to address their apparent obesity. All the motivation did not help. Very good to explain that eating disorders or real overweight, as well as depression still add to it.
Drug therapy or diuretic therapy is not indicated in the treatment of lipedema. Concomitant analgesic treatment is usually ineffective.
The currently valid version of the German S1 guideline Lipedema – AWMF register number: 037-012 (10/2015) is under revision to S2k guideline (consensus-based), and is expected in early 2024.
Among other things, we look forward with great interest to the future conservative therapy recommendations and, in particular, the explanations of their mode of action in the demonstrable absence of edema. In fact, however, the current, guideline-compliant, conservative lipedema treatment provides many patients, with consistent implementation, a significant reduction in symptoms in the following respects: pain, heaviness and tightness. Manual lymphatic drainage therapy should be performed exclusively with accompanying compression therapy for decongestion. Compression therapy can be applied to the legs as well as to the arms. For large caliber jumps (ankle, knee, thigh, and hip circumferences), only a custom-made, flat-knit Class II compression garment (with stitching) is comfortable to wear without constriction. Often the corsetry is made in two parts: e.g. capri pants and knee stocking, or cycling pants and thigh stocking to simplify the daily application of the stiff fabric material and to promote acceptance. Compression therapy is unsuitable for fat reduction and does not influence possible progression of the disease. The conservative therapy accompanies the patient for the rest of her life and sometimes massively restricts the quality of life.
A permanent reduction of the increased fatty tissue in lipedema, by up to 85% of the mass, can be achieved exclusively by means of the surgical measure: liposuction. The indication for the surgical procedure should be given if conservative therapy fails in terms of sufficient pain reduction. Liposuction of the diseased fatty tissue must be performed using a liposuction technique that is gentle on connective tissue, blood vessels and lymphatic vessels. Vibration-assisted liposuction (PAL, powerassisted liposuction) with tumescent local anesthesia or waterjet-assisted liposuction (WAL, waterjetassisted liposuction) without tumescent local anesthesia can be used. Accompanying analgesia makes the surgical procedure easier for both patient and surgeon. The procedure leads to pronounced improvements in pain symptoms, freedom of movement, body shape, and thus quality of life and self-esteem in patients. In some cases, conservative therapy can then be dispensed with completely. The cure of the disease lipedema is currently not possible even by means of surgery; however, postoperative recurrence is an extremely rare event.
Radical, total liposuction treatment of the extremities is contraindicated due to the blood and lymphatic vessel traumatizing procedure and the resulting long-term damage with chronic lymphedema, scars after iatrogenic ulceration, and skin circulatory disturbance, based on benefit and risk considerations. From an aesthetic point of view, the radical surgical approach results in skeletonized, sometimes grotesquely skinny-looking extremities and a subsequent increase in circumference in the trunk area (subcutaneous and visceral fat tissue). This again causes a disproportionate silhouette and in turn has, in part, considerable psychological effects on the patients.
Health policy situation
Due to the insufficient scientific studies worldwide on the surgical therapy of the disease lipedema to recognize liposuction as a benefit of the statutory health insurance in Germany, a trial guideline liposuction was issued by decision of the Joint Federal Committee G-BA in January 2018 [3]. As a result, the multicenter LIPLEG study (registry number: NCT04272827): Liposuction for Lipedema in Stages 1, 2 and 3, was initiated in Germany on 08.02.2021 under dermatological management [4]. The evaluation of the results collected from 450 participants is intended to answer the question of the benefits of liposuction for lipedema compared with conservative, symptom-oriented treatment alone – especially with the use of complex physical decongestive therapy (CPD). The planned end date of the study is 01.09.2025.
In Switzerland, on July 1, 2021, Appendix 1 of the Health Care Benefits Ordinance (KLV) Compulsory Health Care Insurance Remuneration Obligation for Certain Medical Services was amended as follows [5]:
Kapitel 1.1 Liposuktion zur Behandlung von Schmerzen bei Lipödem – Leistungspflicht in Evaluation bis 31.12.2025: «Wenn die mit dem Lipödem verbundenen Schmerzen ungenügend auf intensive und dokumentierte konservative Therapie (konsequente Kompressionstherapie, manuelle Lymphdrainagetherapie) von mindestens zwölf Monaten Dauer ansprechen. Kostenübernahme nur auf vorgängige besondere Gutsprache des Versicherers, der die Empfehlung des Vertrauensarztes oder der Vertrauensärztin berücksichtigt. Indikationsstellung interdisziplinär durch mindestens zwei der folgenden Fachärzte oder Fachärztinnen für Angiologie, Plastisch-Rekonstruktive und Ästhetische Chirurgie, Endokrinologie/Diabetologie oder Dermatologie. Durchführung durch einen Facharzt oder eine Fachärztin mit profundem Wissen mit der Technik der Liposuktion.»
Take-Home Messages
- Lipedema is a disease (ICD10 GM2023: E88.20 – E88.22)
- Clinical diagnosis: no pain – no lipedema
- S1 Guideline: www.awmf.de (No. 037/012) – as of 10/2015, currently under revision.
- Conservative therapy does not stop progression
- Surgical therapy in case of failure of conservative therapy with regard to pain symptoms
- Recognized surgical methods:
– Liposuction vibration-assisted under tumescent local anesthesia
– Liposuction in water jet technique - Cost absorption of liposuction by health insurances possible after approval of costs
Literature:
- DIMDI: ICD-10-GM, Version 2023 , www.dimdi.de/static/de/klassifikationen/icd/icd-10-gm/kode-suche/htmlgm2023/block-e70-e90.htm,(last accessed 08.06.2023).
- AWMF: Guidelines: Lipedema. Registration number 037-012.
www.awmf.org/leitlinien/detail/ll/037-012.html,(last accessed 19.05.2023) - LIPLEG Study, www.g-ba.de/studien/erprobung/lipleg-studie,(last accessed May 19, 2023).
- Podda M, et al: A randomised controlled multicentre investigator-blinded clinical trial comparing efficacy and safety of surgery versus complex physical decongestive therapy for lipedema (LIPLEG). Trials 2021; 22(1): 758. doi: 10.1186/s13063-021-05727-2.
- Federal Office of Public Health (FOPH): Annex 1 of the Ordinance on Health Care Services (KLV), www.bag.admin.ch/bag/de/home/versicherungen/krankenversicherung/krankenversicherung-leistungen-tarife/Aerztliche-Leistungen-in-der-Krankenversicherung/anhang1klv.html,(last accessed 19.05.2023).
- Hirslanden Klink St. Anna AG, LipödemZentrum Zentralschweiz,
Meggen.
HAUSARZT PRAXIS 2023; 18(11): 10–14